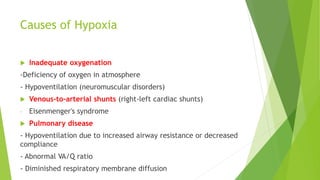
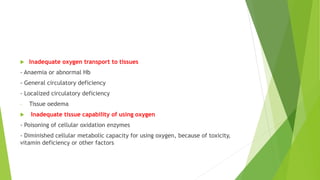
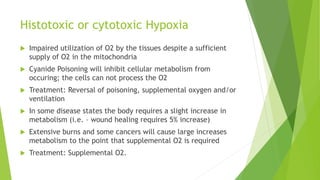
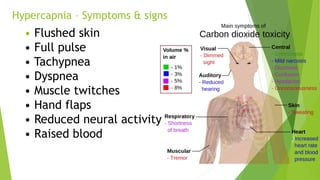
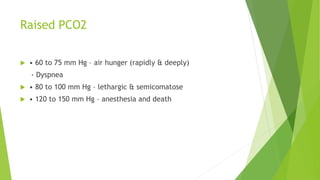
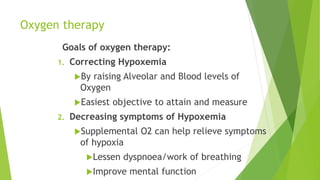
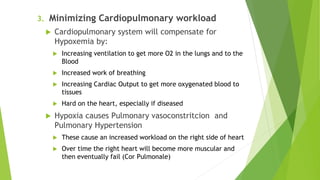
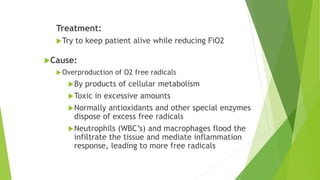
Hypoxia refers to inadequate oxygen supply at the tissue level. It can be caused by problems with oxygen delivery, transport, or cellular uptake. Effects of hypoxia range from impaired mental function to cell death. There are several types of hypoxia depending on the underlying cause, such as atmospheric, anemic, or circulatory hypoxia. Oxygen therapy aims to correct hypoxemia by raising oxygen levels, reducing symptoms, and minimizing cardiovascular strain. Care must be taken to avoid oxygen toxicity from prolonged high concentrations.