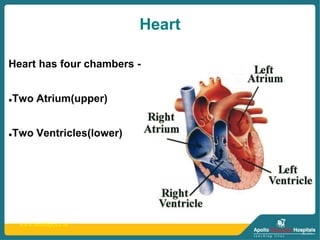
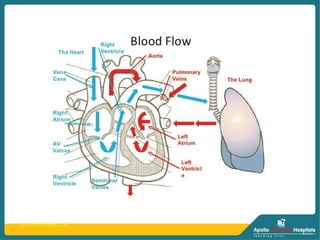
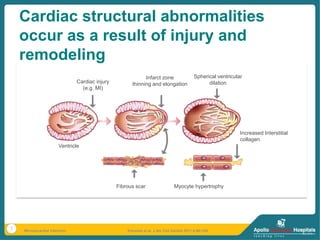
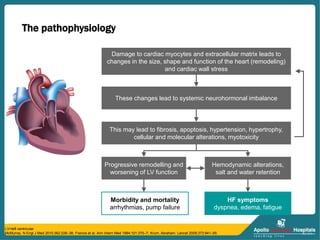
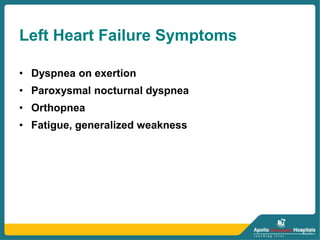
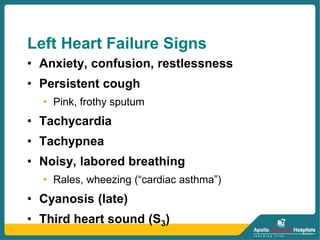
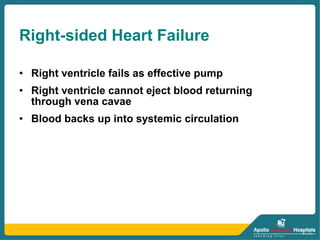
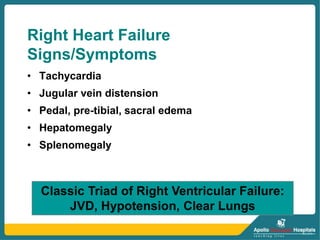
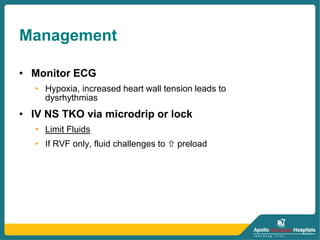
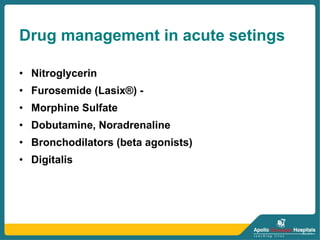
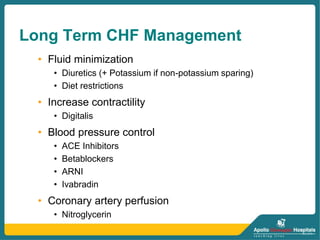
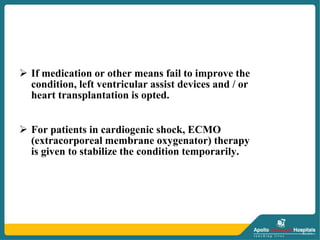
Heart failure occurs when the heart is unable to pump enough blood to meet the body's needs. It can develop when the heart muscle is damaged, such as from a myocardial infarction. There are two main types - left heart failure which causes blood to back up in the lungs, and right heart failure where blood backs up in the body. Symptoms depend on whether it is left or right heart failure, and include shortness of breath, fatigue, swelling, and coughing. Treatment focuses on reducing cardiac workload, increasing blood oxygen levels, and limiting fluid buildup through medications, oxygen therapy, and monitoring for arrhythmias.