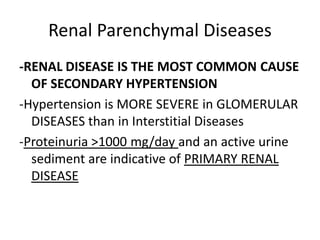
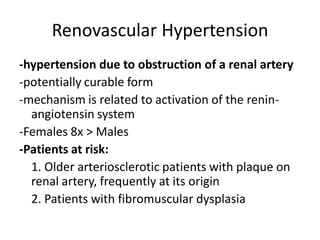
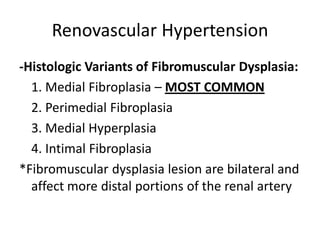
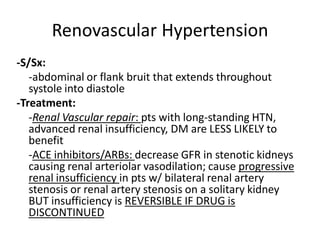
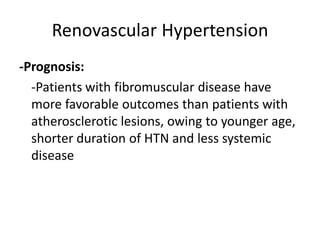
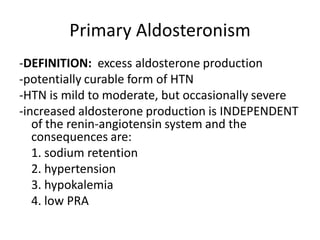
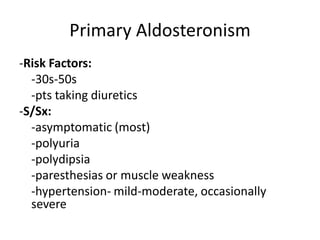
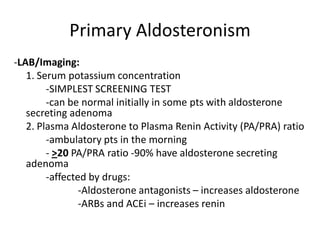
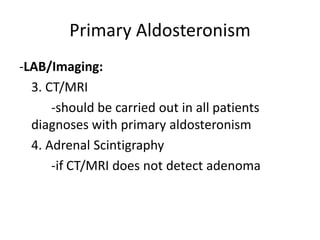
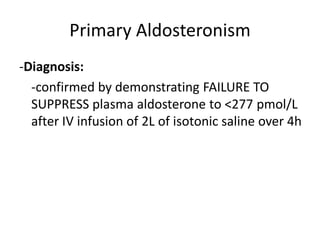
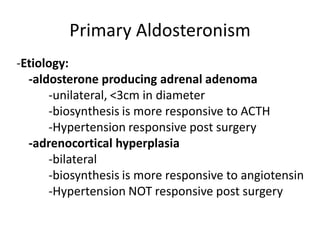
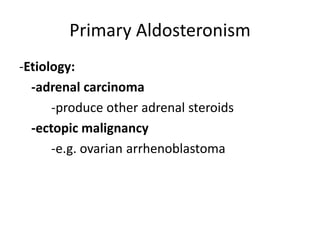
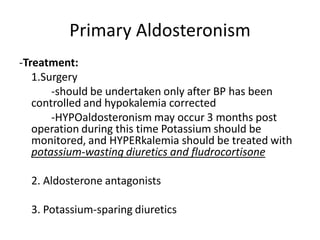
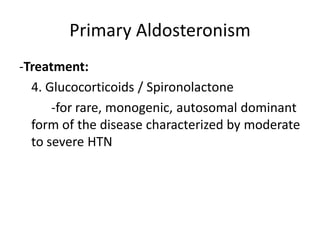
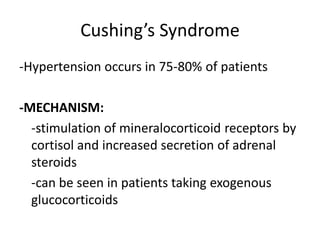
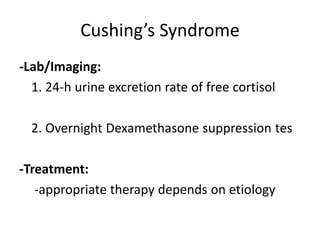
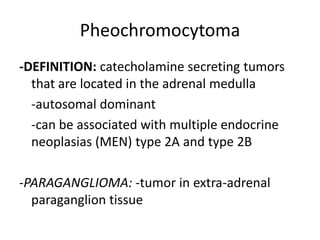
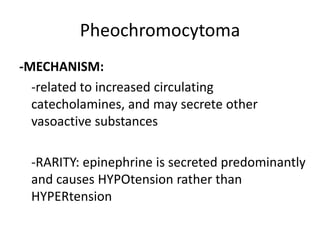
The document discusses secondary hypertension, defining it as elevated blood pressure due to an underlying disorder. The most common causes of secondary hypertension include renal parenchymal diseases, primary aldosteronism, Cushing's syndrome, pheochromocytoma, and renovascular hypertension. It provides details on the definition, causes, signs and symptoms, diagnostic tests, treatment options, and prognosis for each of these common causes of secondary hypertension.