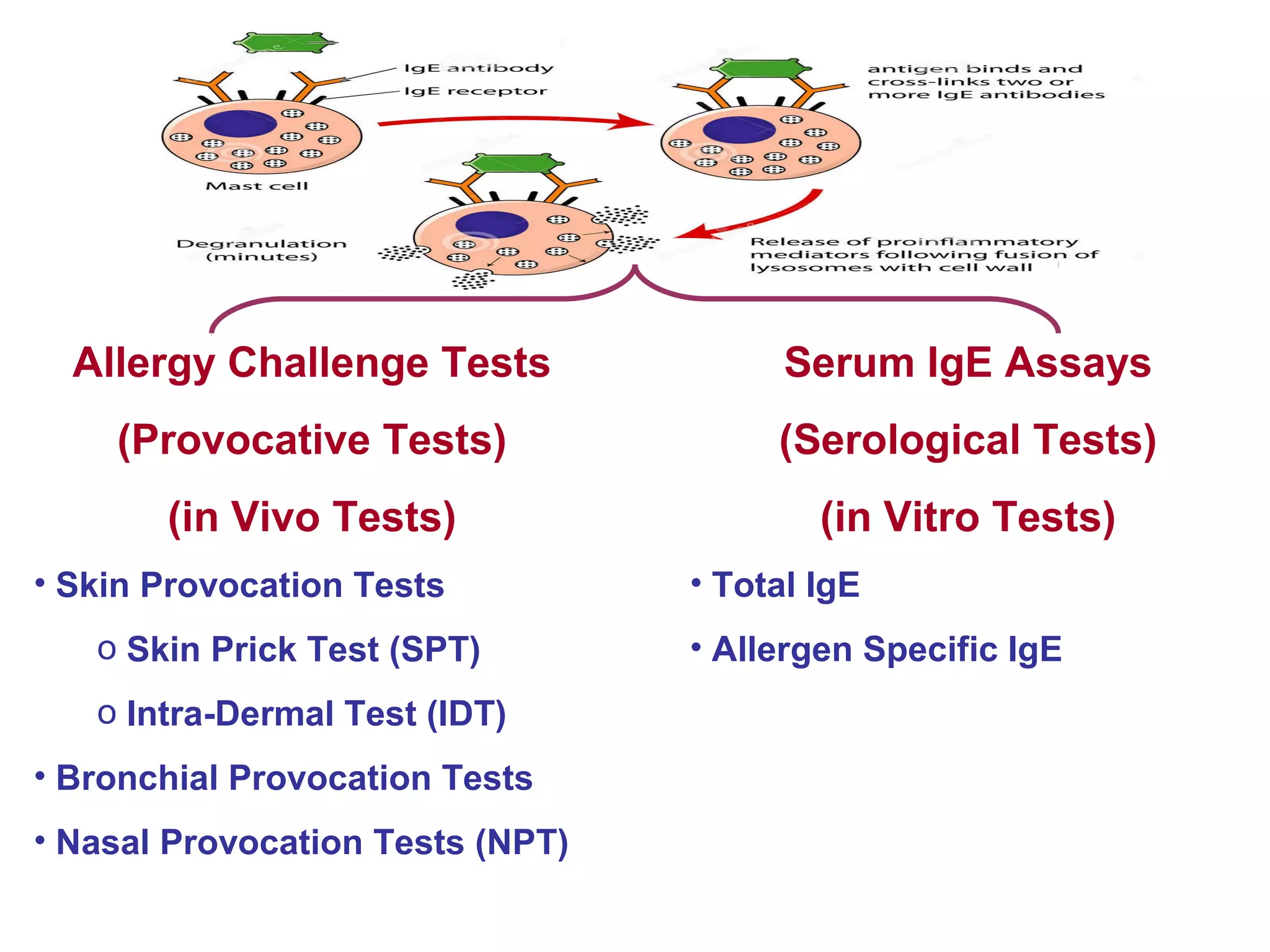
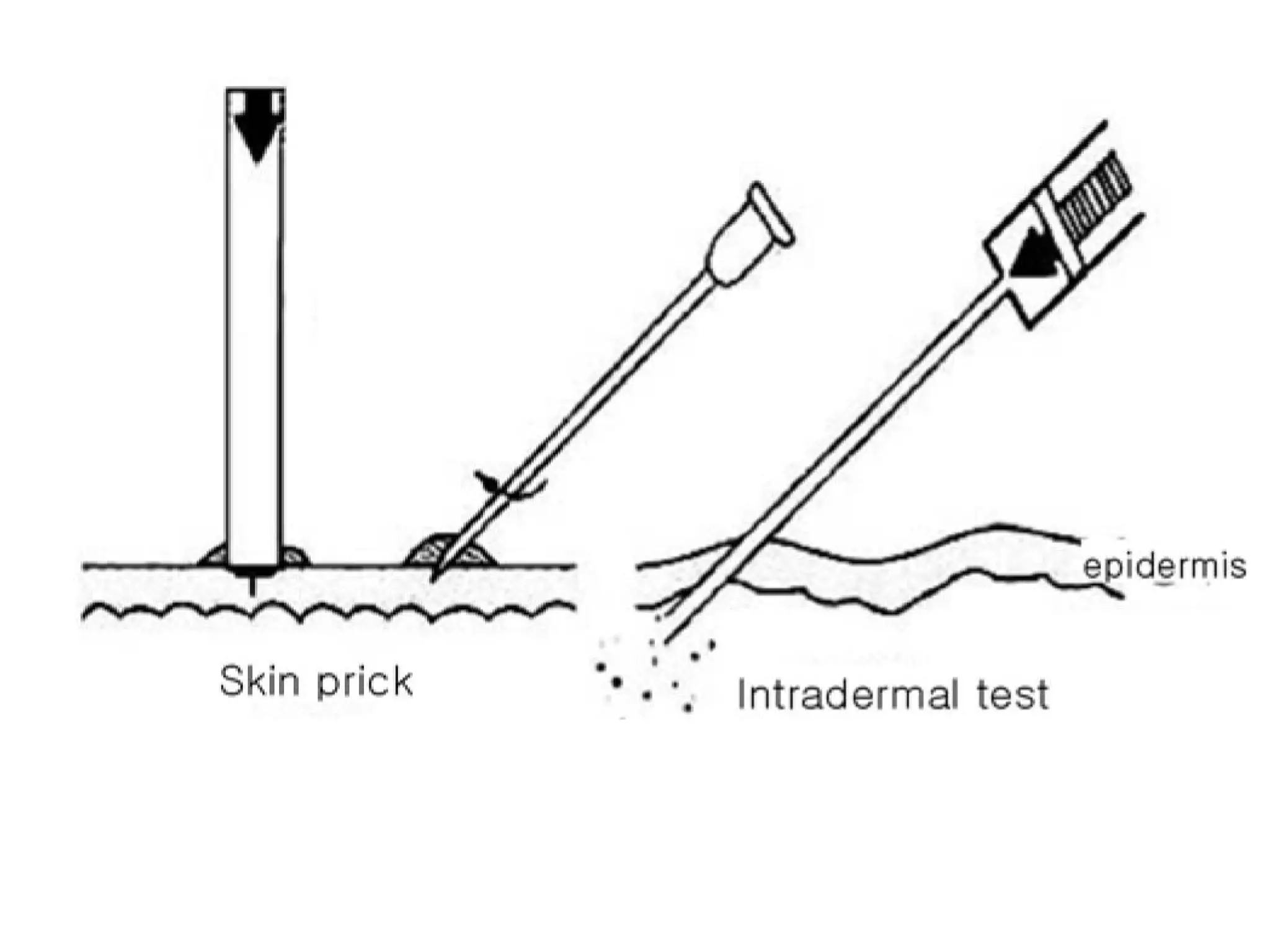
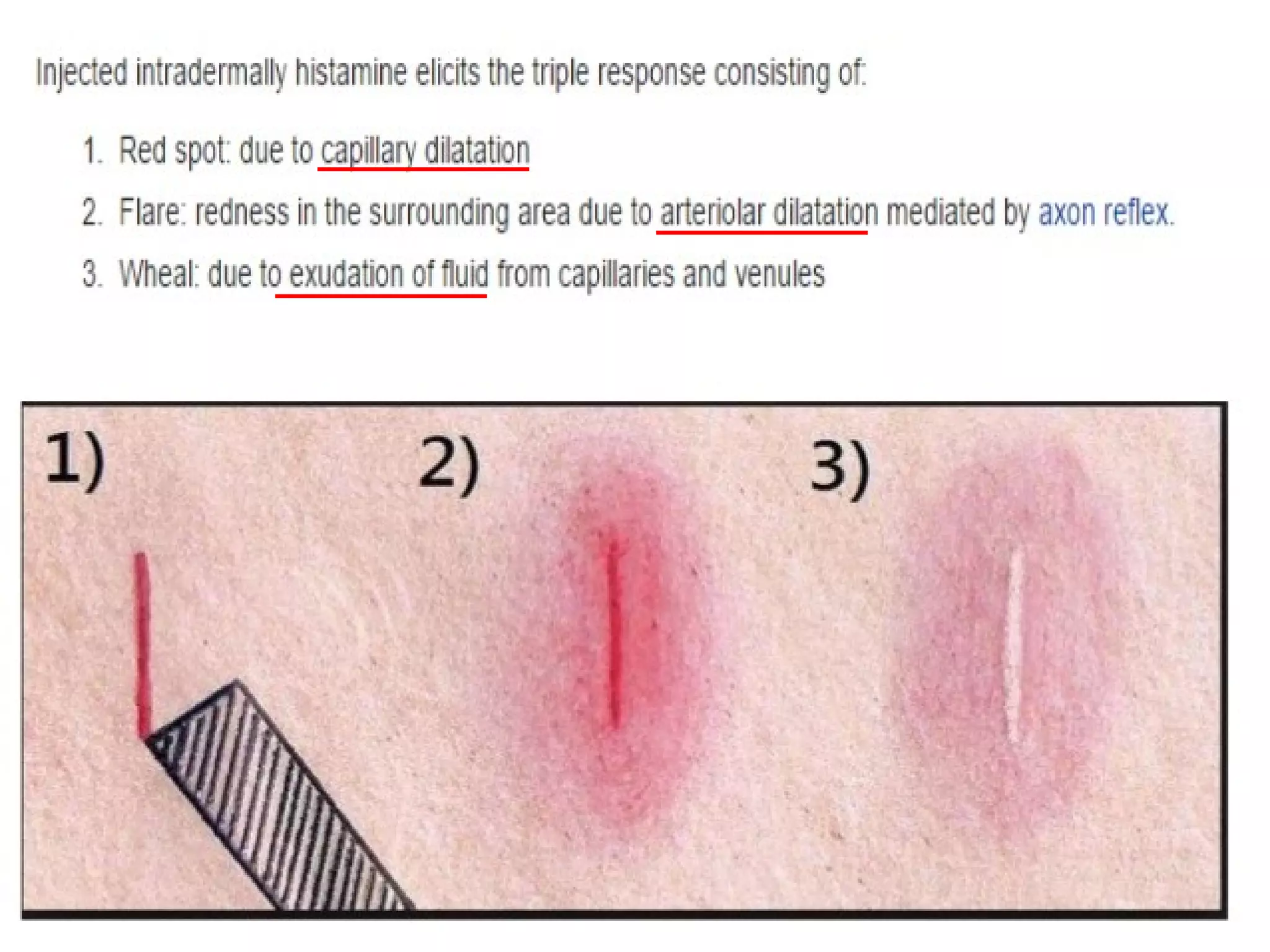
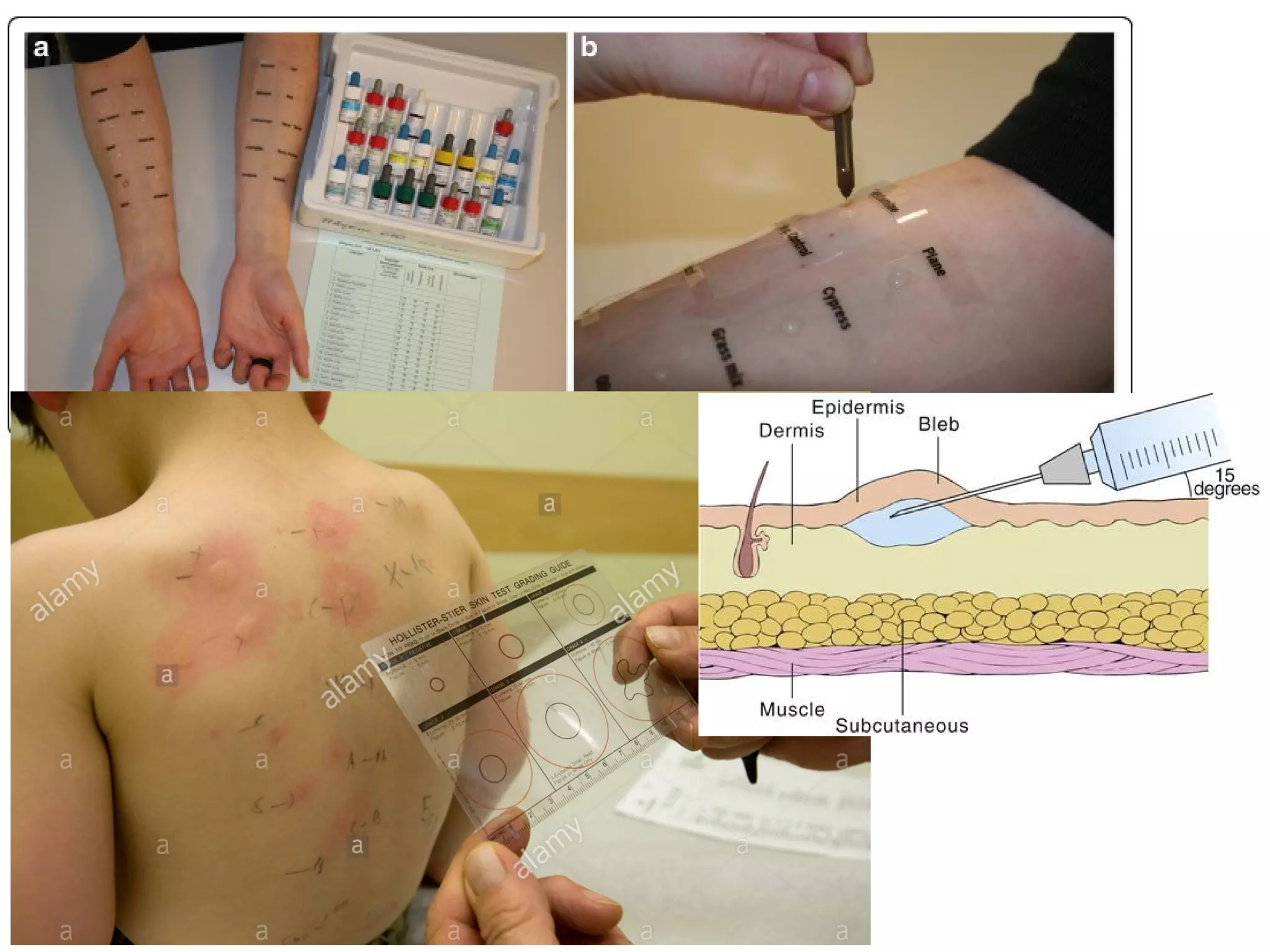
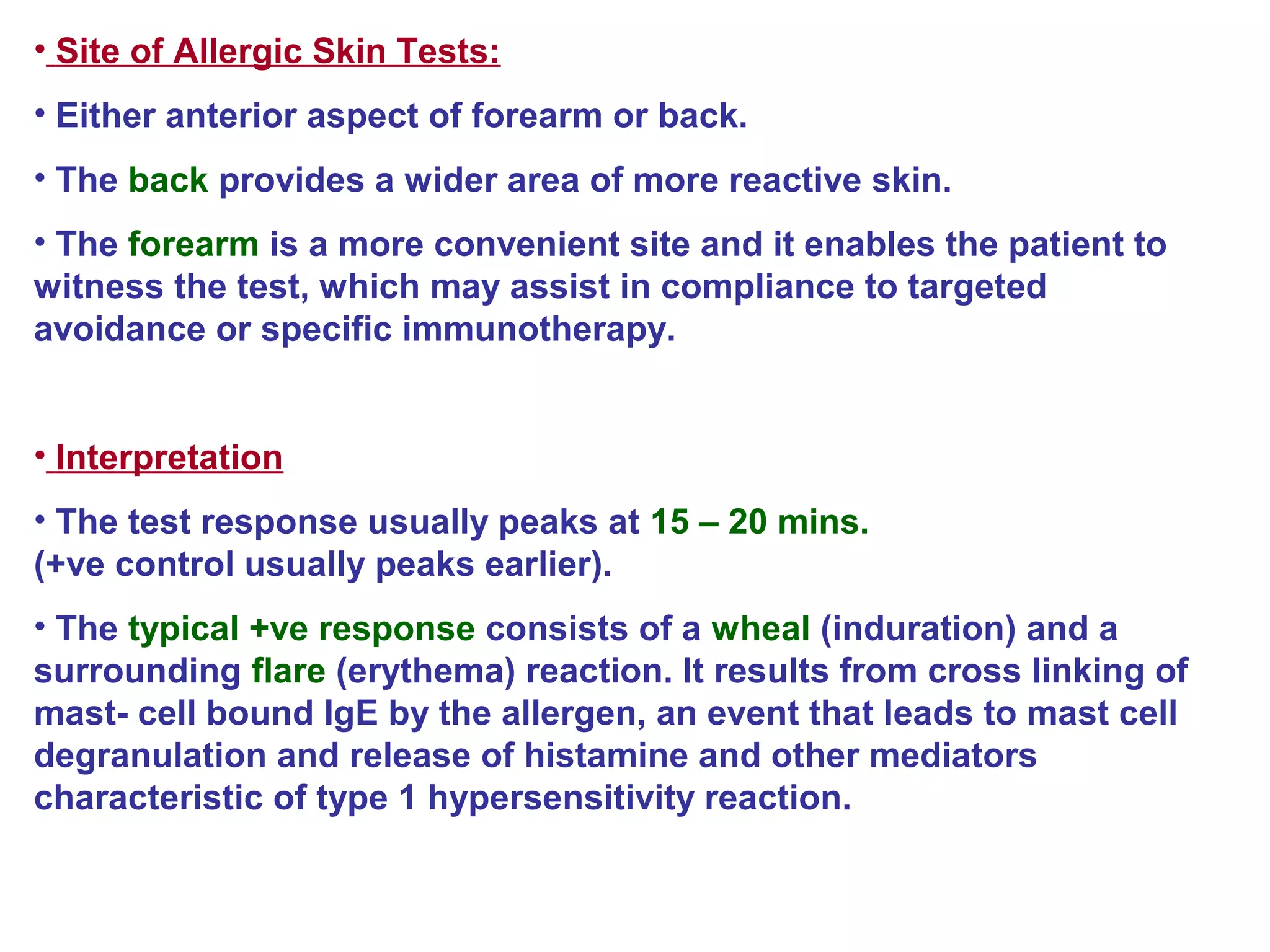
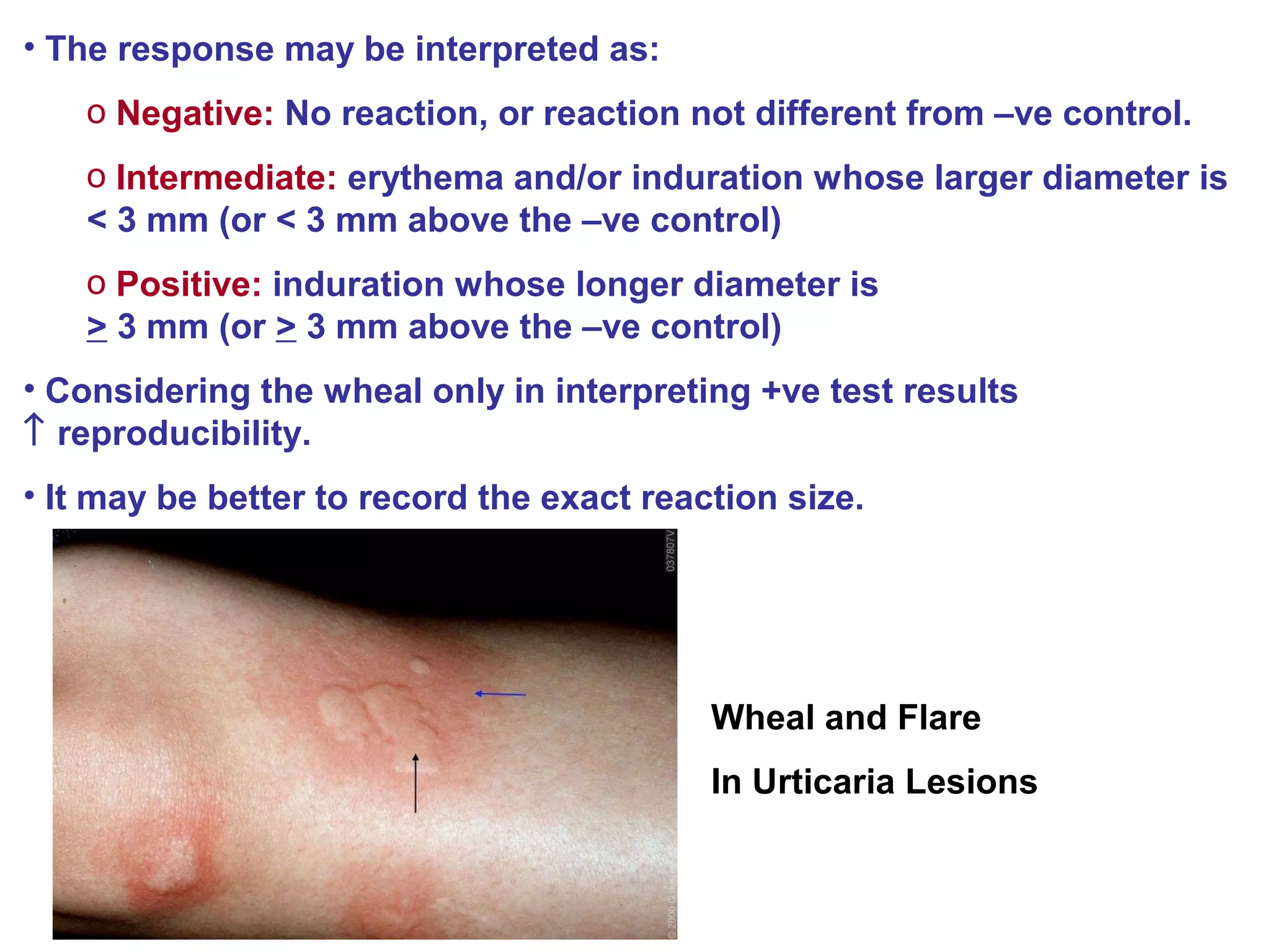
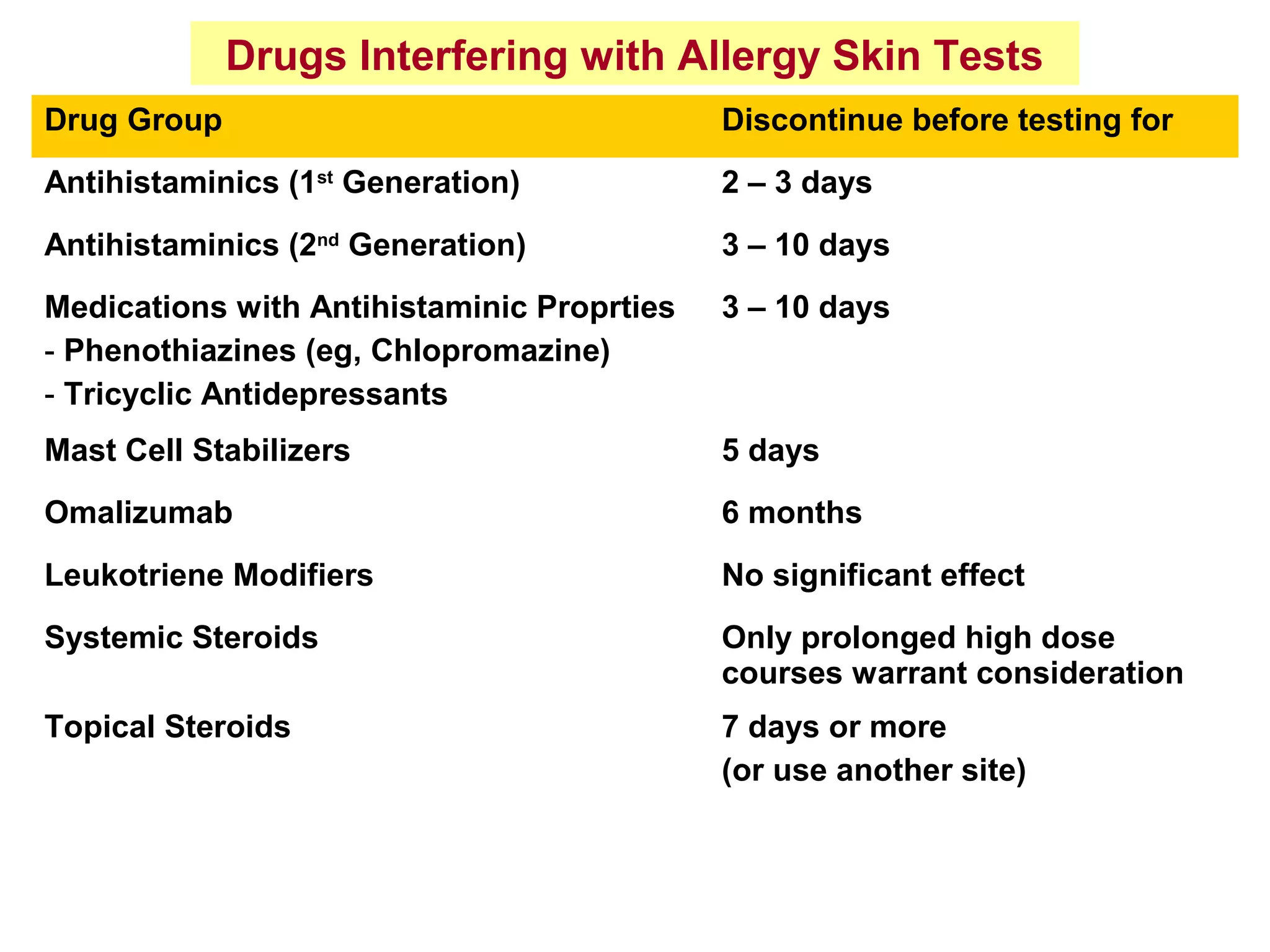
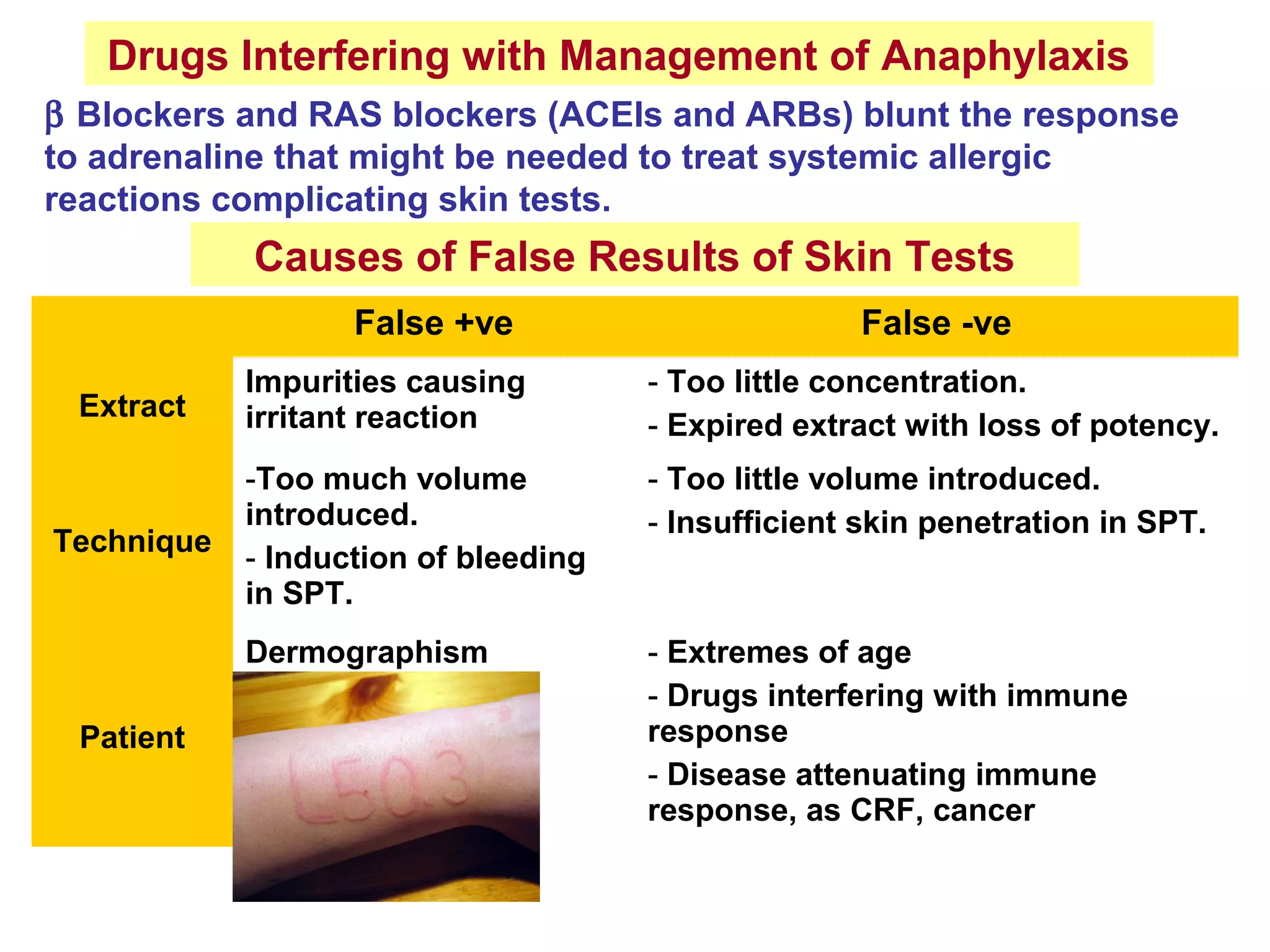
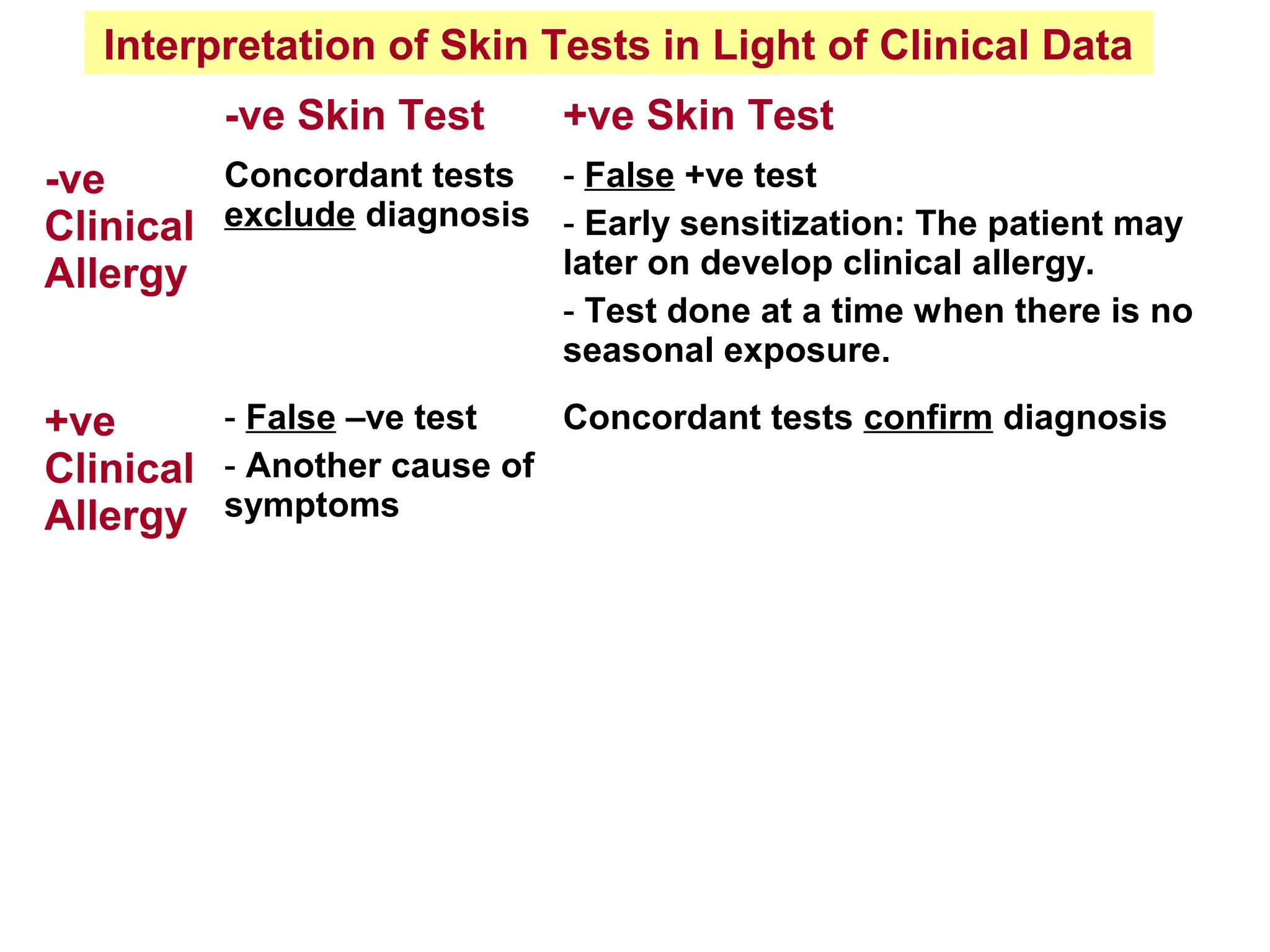
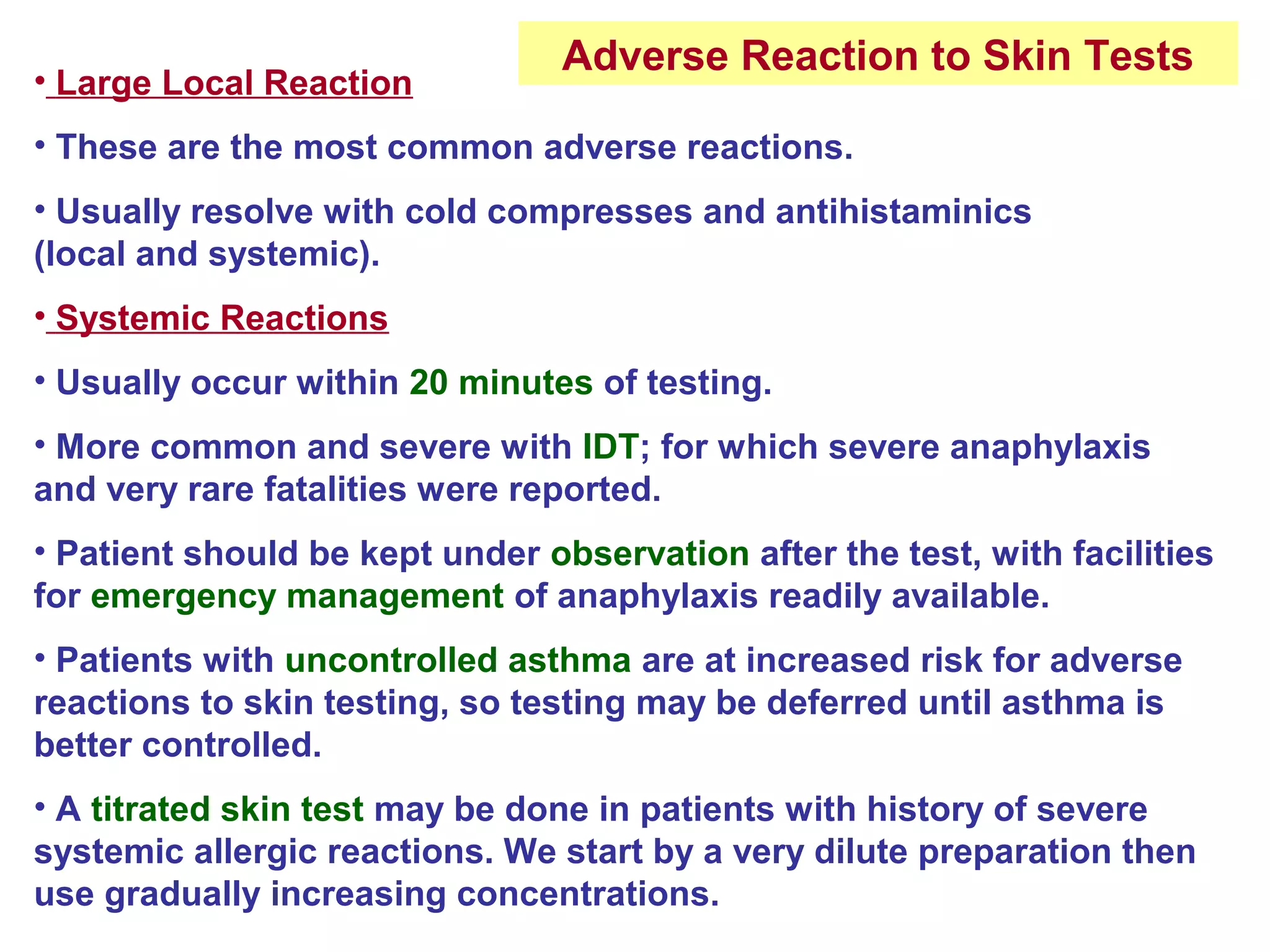
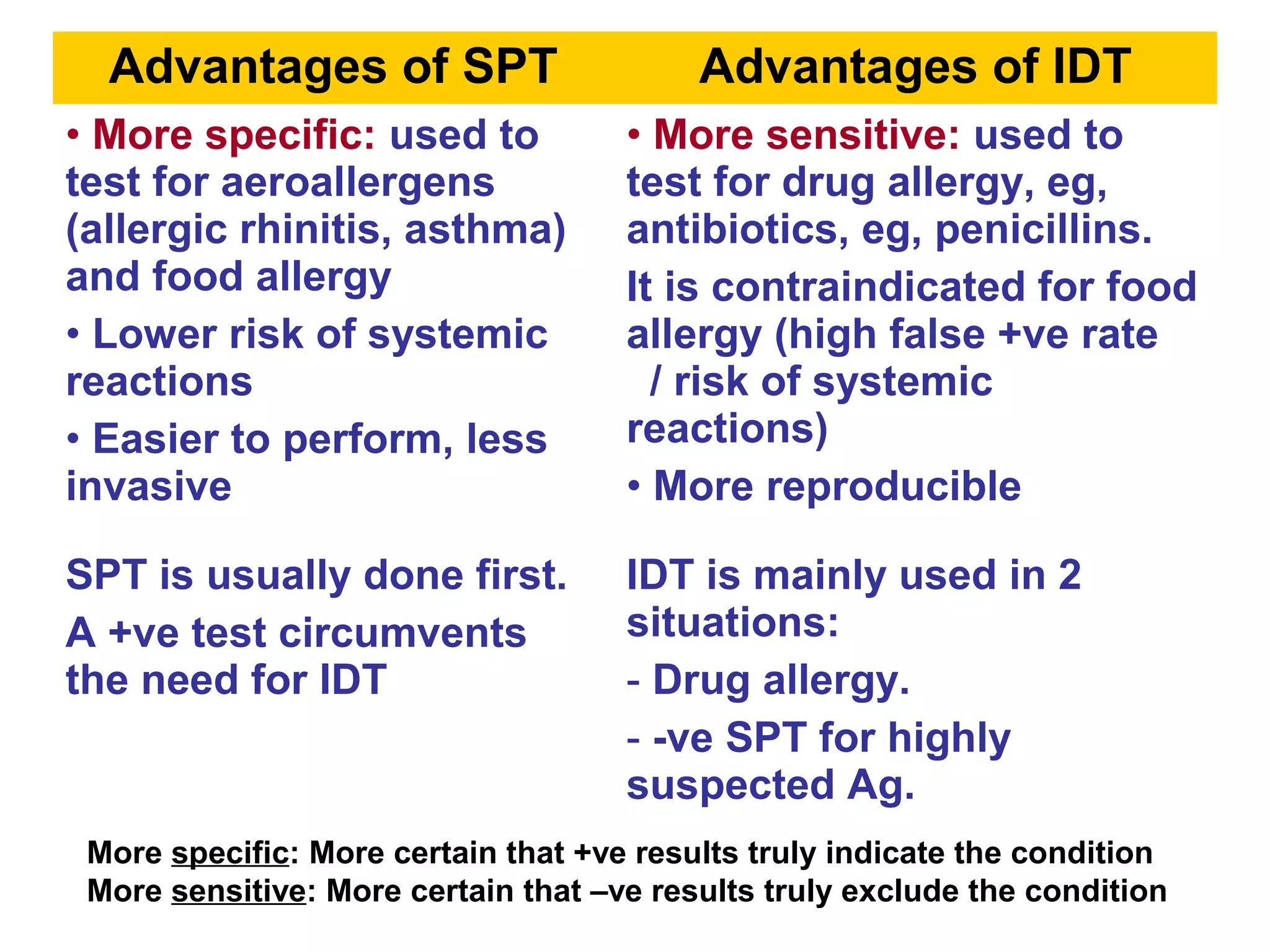
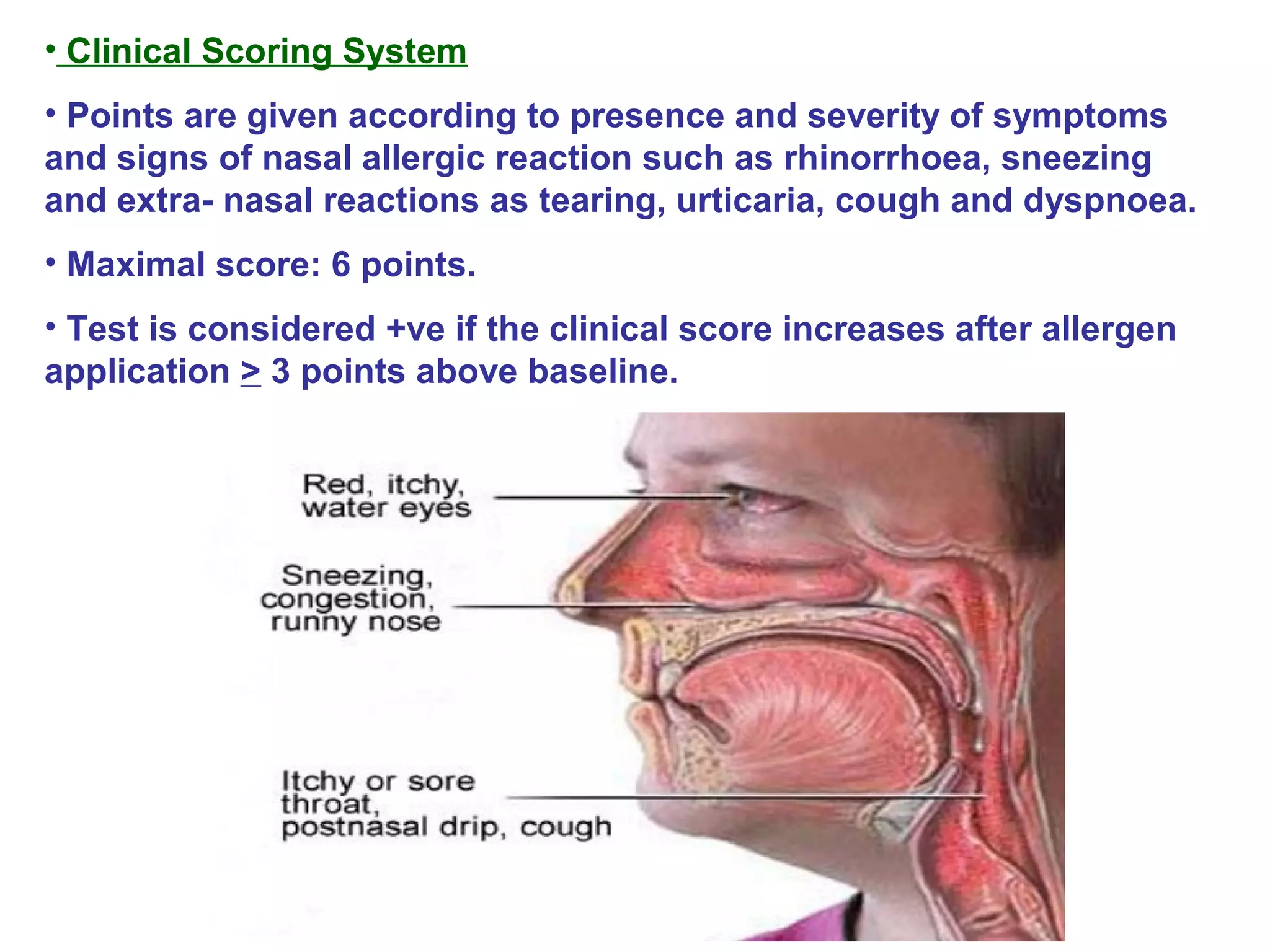
This document provides information on different types of allergy tests, including skin prick tests, intradermal tests, serum IgE assays, nasal provocation tests, and bronchial provocation tests. It describes how each test is performed, interpreted, and its advantages and disadvantages. Allergy tests are used to identify specific allergens that may be causing a person's symptoms in order to guide allergen avoidance and immunotherapy treatments. Precautions must be taken with allergy challenge tests due to the risk of systemic allergic reactions.