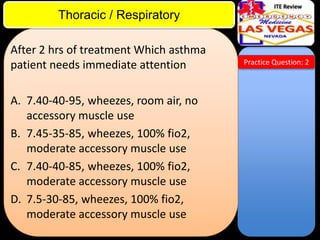
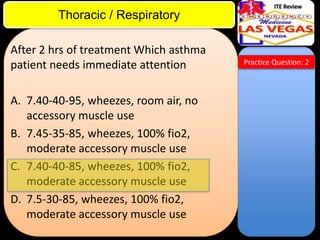
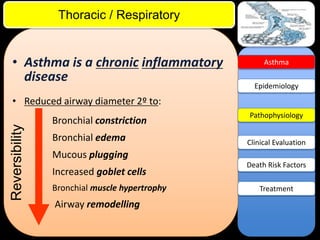
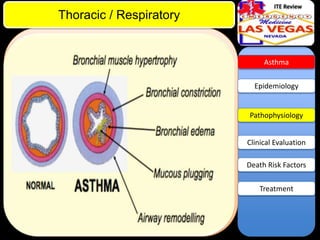
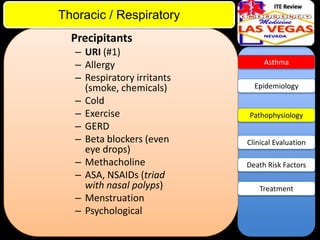
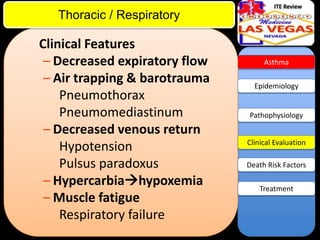
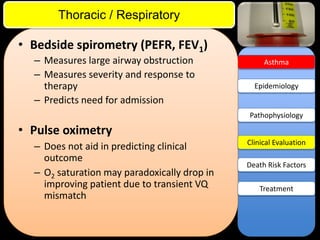
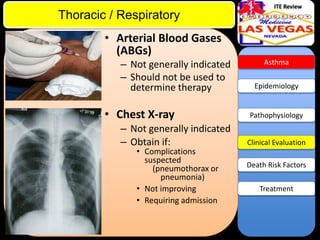
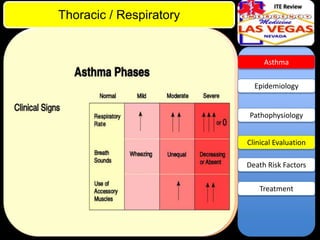
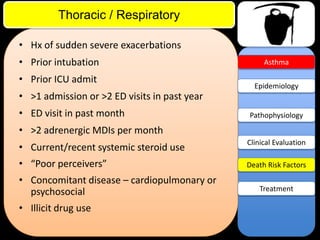
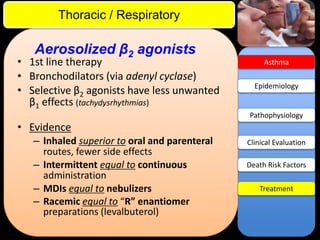
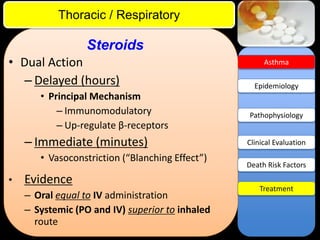
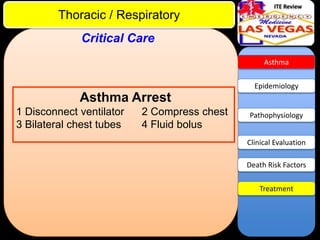
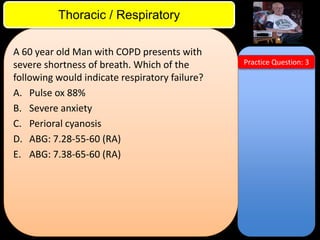
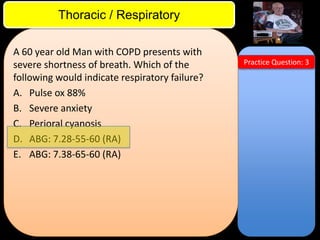
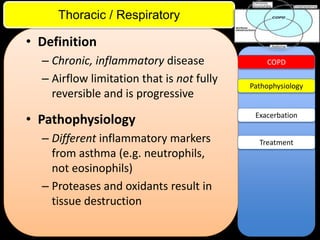
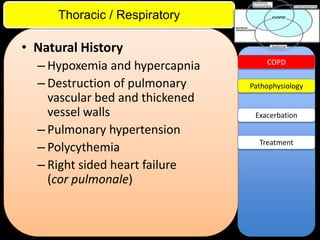
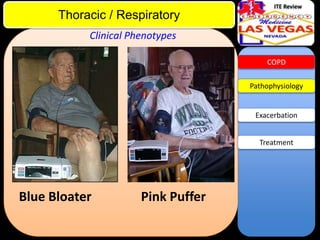
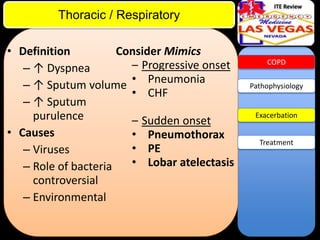
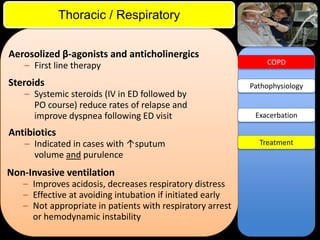
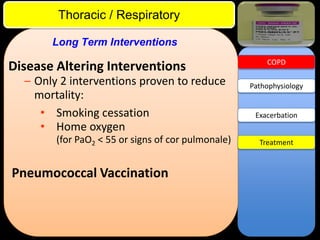
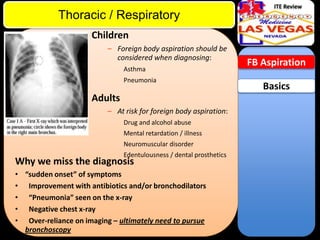
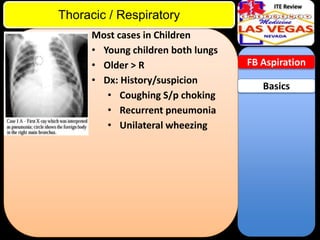
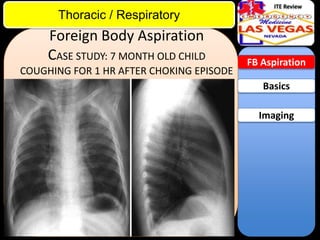
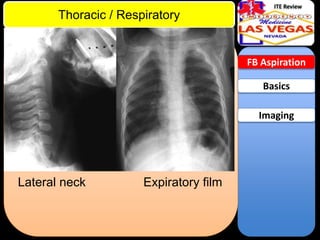
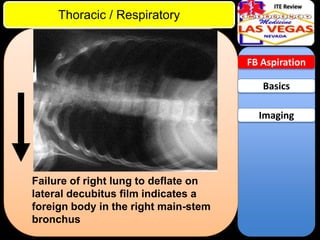
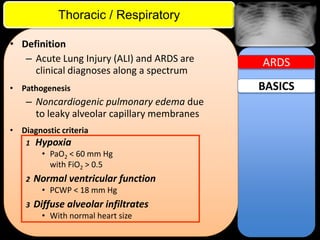
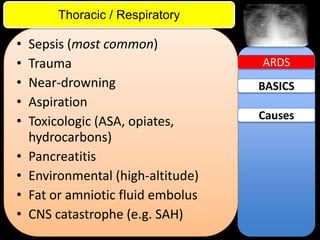
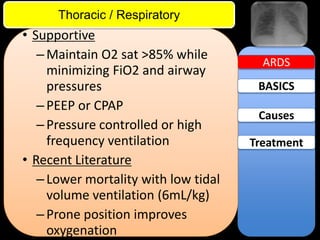
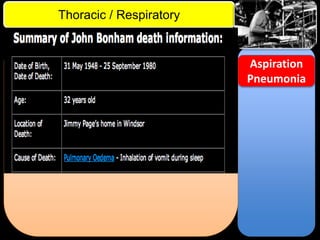
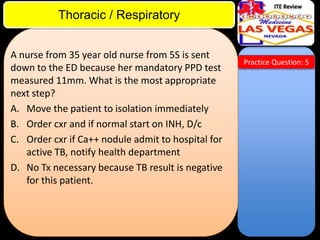
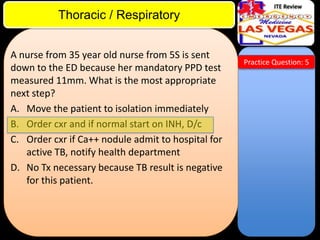
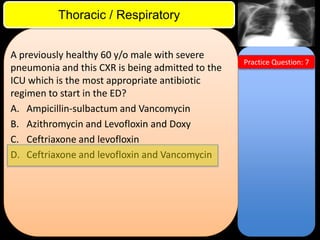
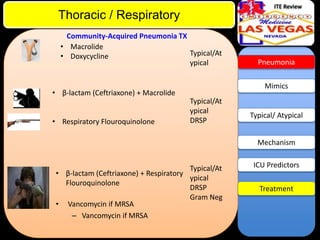
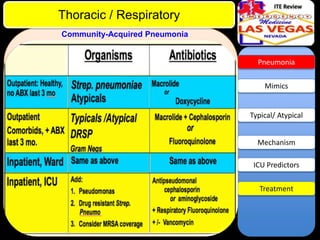
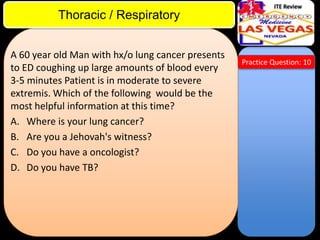
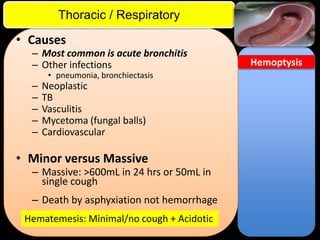
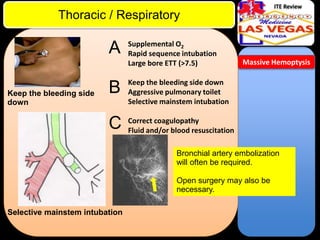
This document contains lecture slides from Dr. J.D. McCourt on various thoracic and respiratory topics. It includes practice questions, discussions of conditions like asthma, COPD, foreign body aspiration, and ARDS. For one practice question, the document indicates that an ABG with a pCO2 of 55 mmHg would indicate respiratory failure in a patient with COPD presenting with shortness of breath. It also provides overview information on the definitions, pathophysiology, presentations, treatments and more for several common pulmonary conditions.