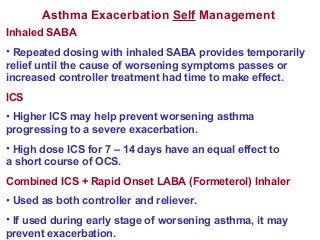
Asthma exacerbations are episodes where asthma symptoms progressively worsen, requiring a change in treatment. They are usually caused by viral infections, allergens, or poor adherence to controller medications. Management may begin with self-management using short-acting bronchodilators. For more severe exacerbations, oral corticosteroids may be needed. In the hospital, treatments include oxygen, inhaled bronchodilators, corticosteroids, and sometimes magnesium sulfate. Proper management can prevent exacerbations from worsening.