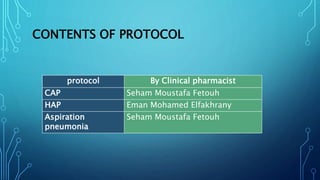
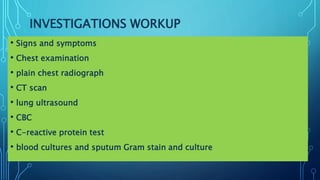
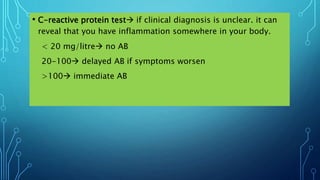
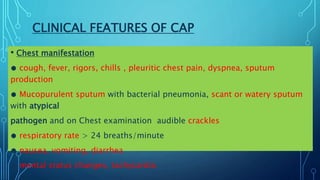
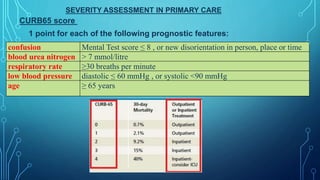
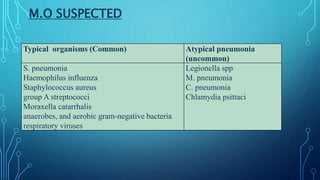
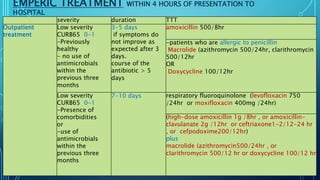
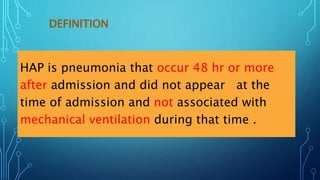
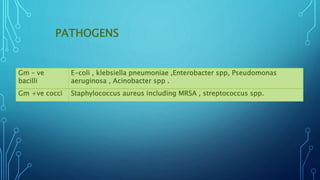
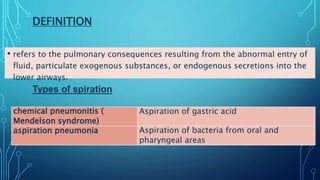
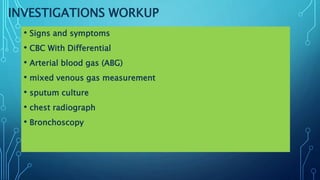
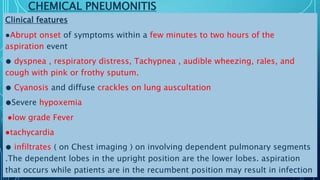
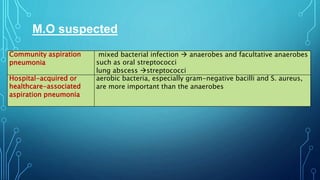
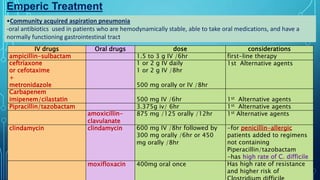
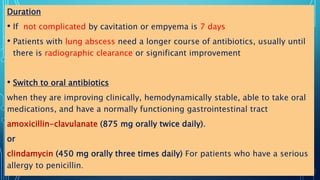
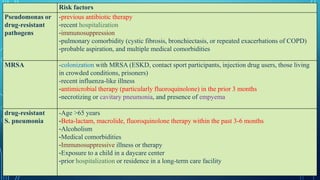
This document outlines protocols for treating various types of pneumonia, including community-acquired pneumonia (CAP), hospital-acquired pneumonia (HAP), and aspiration pneumonia. It details definitions, clinical features, common pathogens, investigations and workup, severity assessments, empirical antibiotic treatment options and durations, and monitoring considerations for each type. Empirical treatment regimens are tailored based on severity and risk factors. Duration of treatment typically ranges from 7-10 days but may be longer for complicated cases.