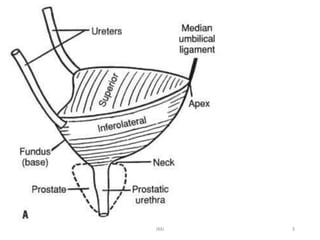
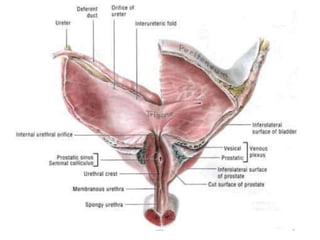
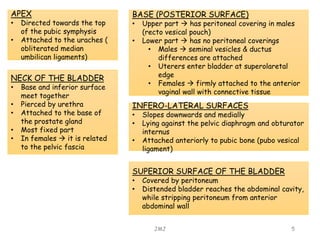
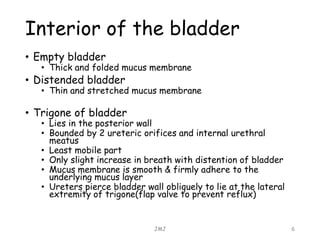
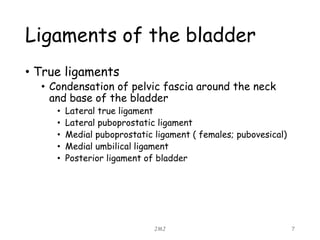
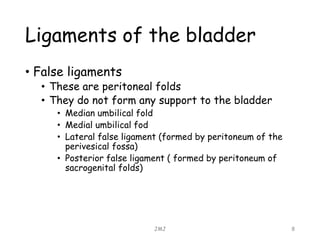
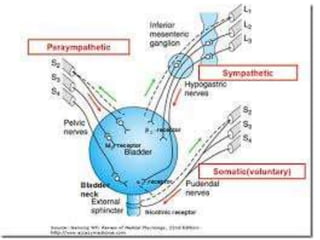
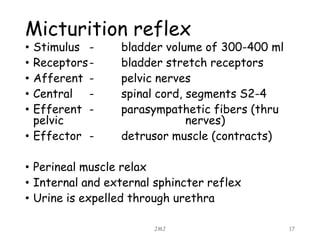
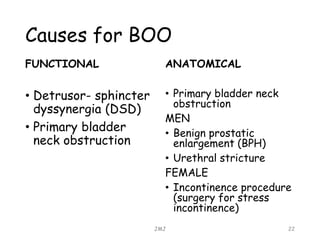
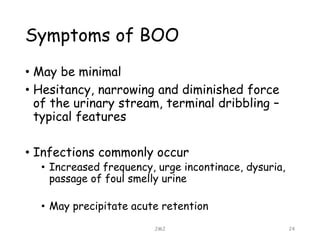
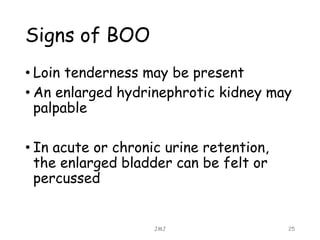
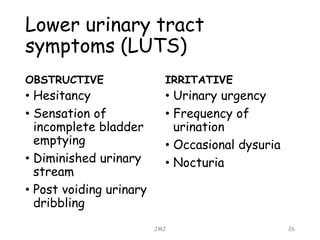
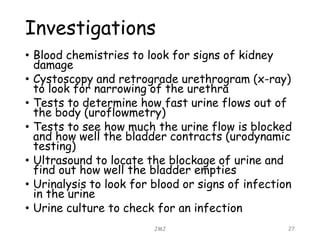
This document provides an overview of bladder anatomy, function, and bladder outlet obstruction. It describes the key parts of the bladder including relations to other organs. Normal micturition and factors that assist storage are explained. Causes of bladder outlet obstruction include anatomical and functional issues. Common symptoms include hesitancy, weak stream, and urinary tract infections. Investigations help locate the site of obstruction and assess kidney and bladder function.