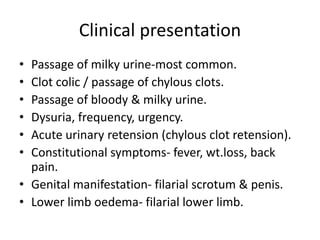
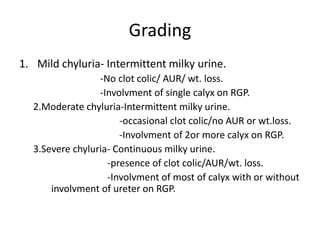
Chyluria is a condition characterized by the presence of chyle or fatty lymph in the urine, causing it to appear milky white. It is most commonly caused by filarial infections in parts of Africa and India. The condition results from obstruction or insufficiency of the lymphatic system, causing retrograde flow of lymph into the urinary tract. Diagnosis involves urine tests to detect triglycerides and lymph. Treatment options include medication to treat underlying causes, sclerotherapy to scar lymphatic vessels, and surgery such as lymphatic disconnection or lymph node-vein anastomosis if more conservative treatments fail.