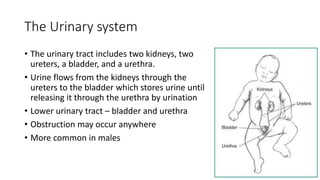
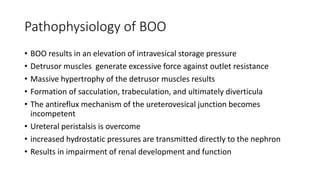
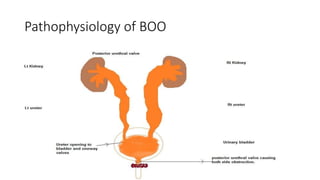
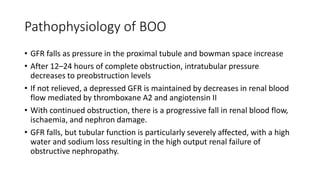
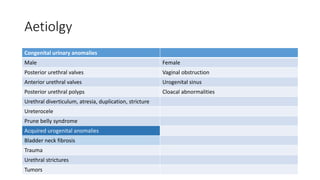
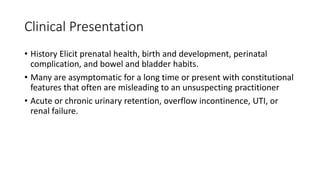
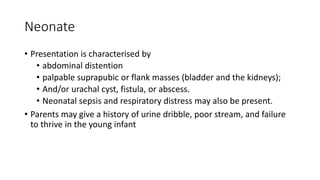
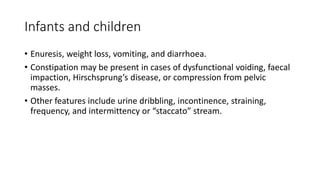
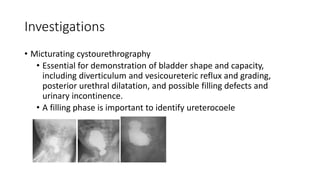
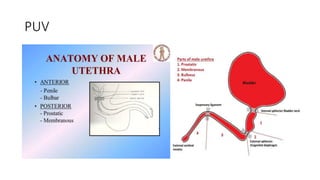
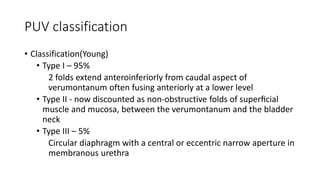
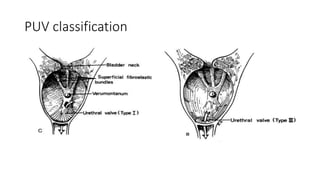
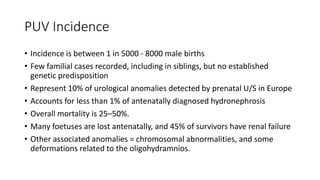
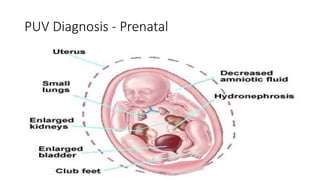
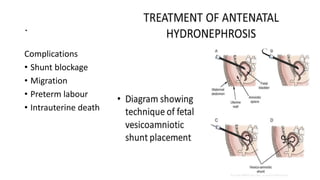
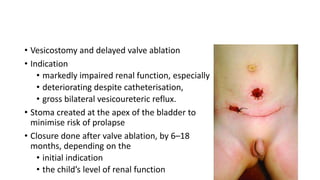
This document discusses bladder outlet obstruction (BOO). It begins by defining BOO and describing that it can be partial or complete. It then discusses the various causes of BOO including congenital and acquired factors. The pathophysiology of BOO is explained, noting how it can lead to renal damage over time if not treated. The document outlines the evaluation and management of BOO, including various imaging modalities and the importance of early surgical treatment to prevent long term renal issues. Posterior urethral valves are highlighted as a common cause of BOO in boys.