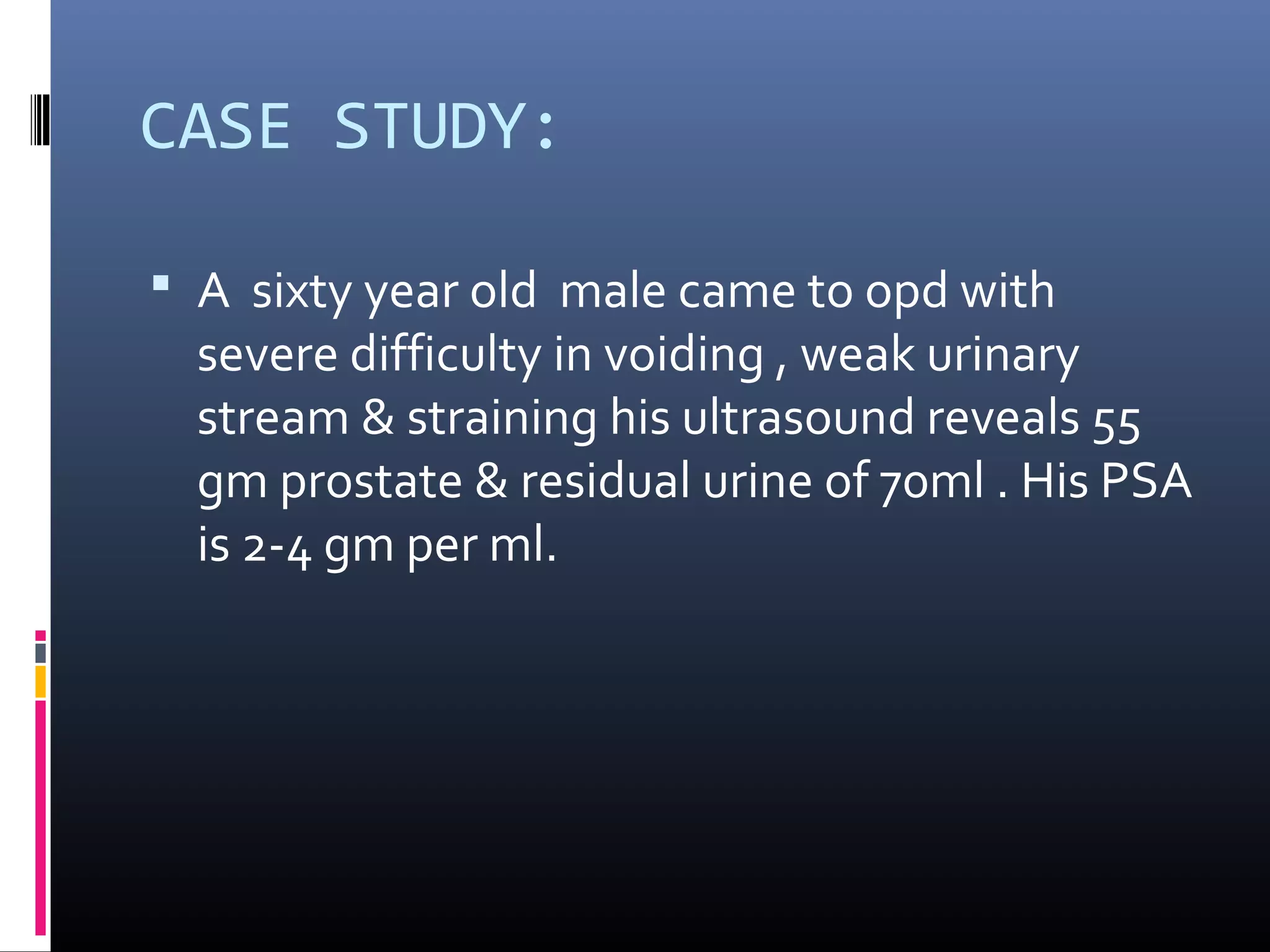
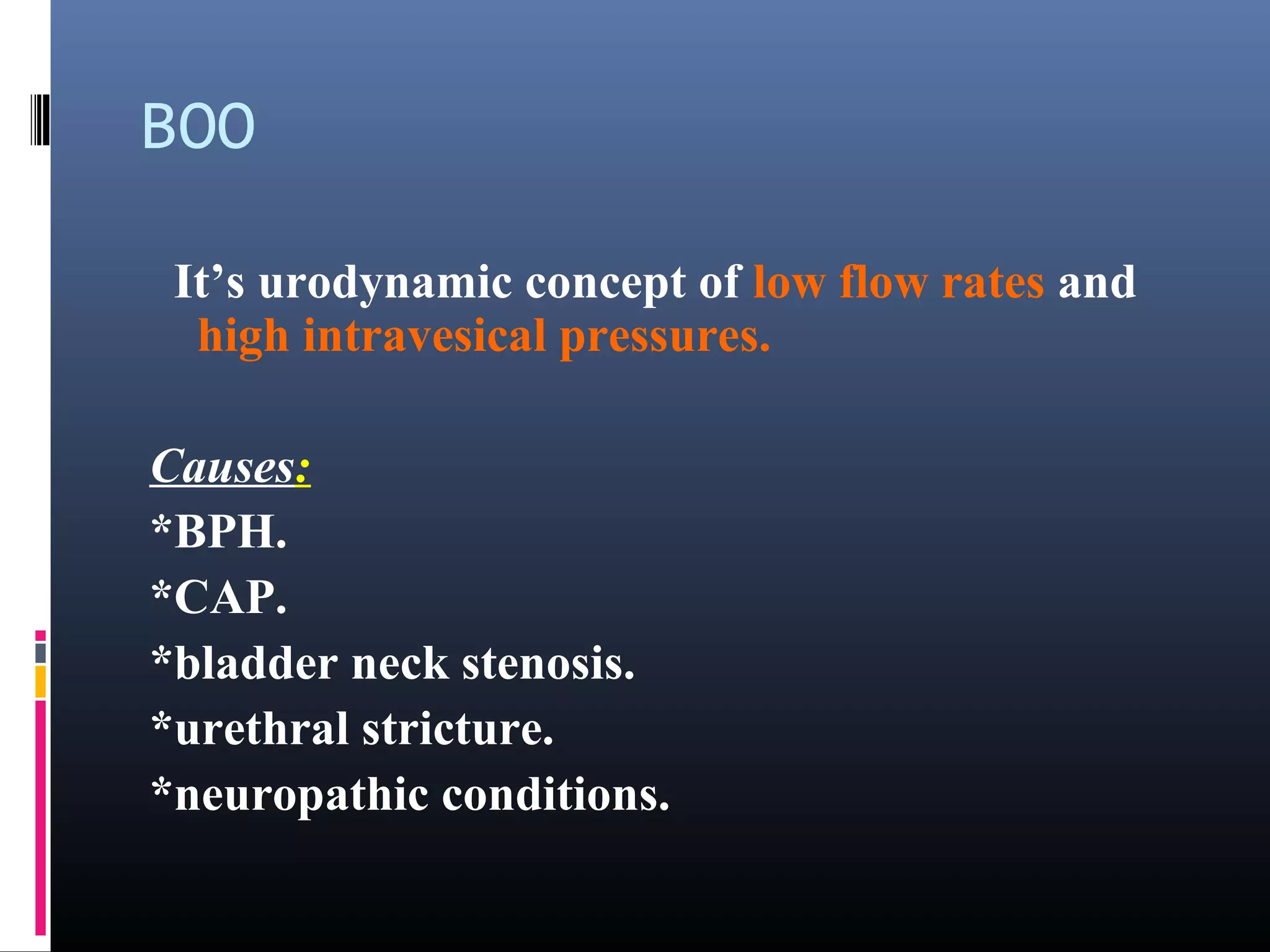
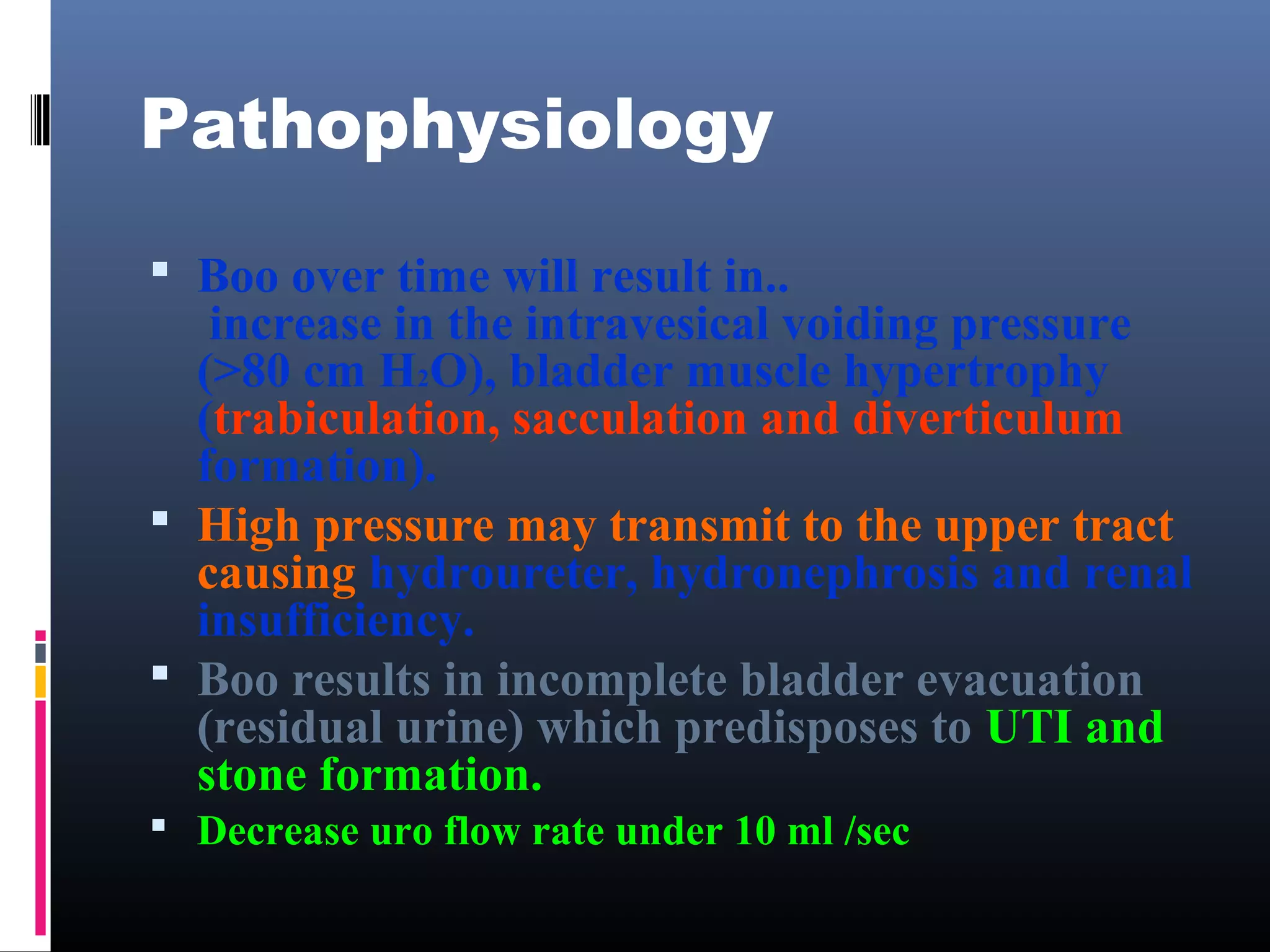
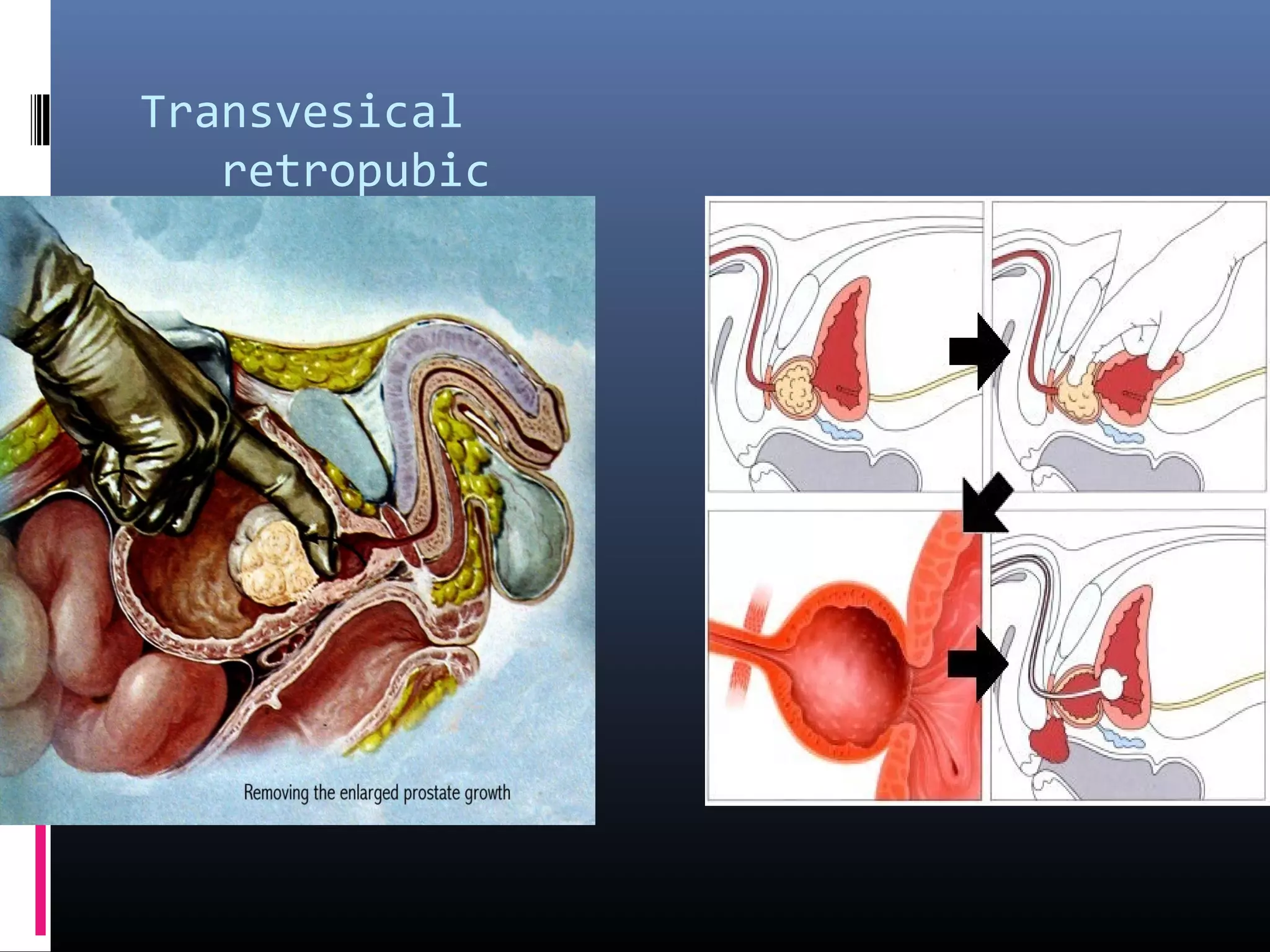
This document discusses benign prostatic hyperplasia (BPH) and its treatment. It begins with a case study of a 60-year-old male patient presenting with urinary difficulties. It then defines bladder outlet obstruction and discusses the pathophysiology and symptoms of BPH, including increased voiding pressures and residual urine. Treatment options covered include lifestyle changes, medications like alpha blockers and 5-alpha-reductase inhibitors, and procedures like transurethral resection of the prostate. Complications of treatment are also summarized.






![IPSS [international prostatic symptom score]](https://image.slidesharecdn.com/bladderoutletobstruction-180130153330/75/Bladder-outlet-obstruction-12-2048.jpg)











![Complications:
Early:
Hemorrhage.
Infection.
Wound infection[in open prostatectomy]](https://image.slidesharecdn.com/bladderoutletobstruction-180130153330/75/Bladder-outlet-obstruction-29-2048.jpg)