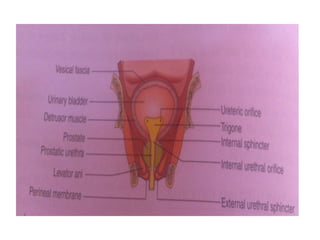
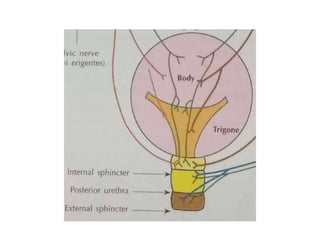
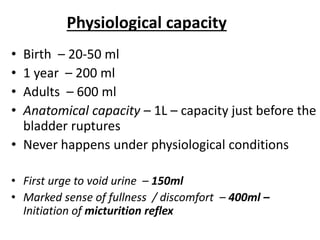
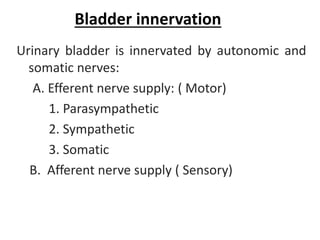
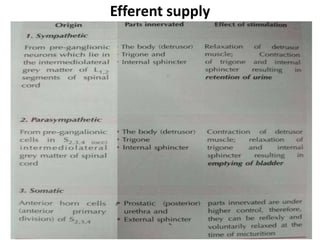
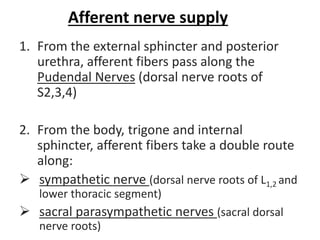
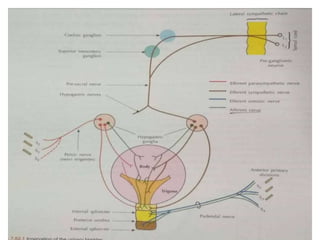
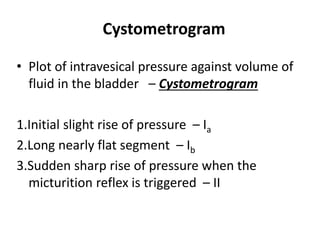
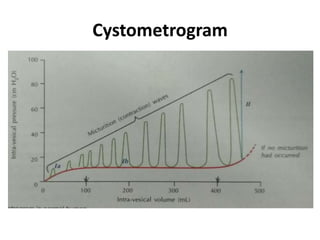
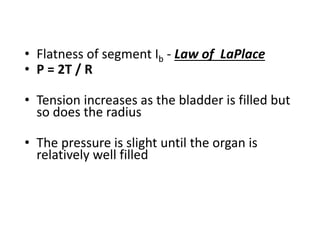
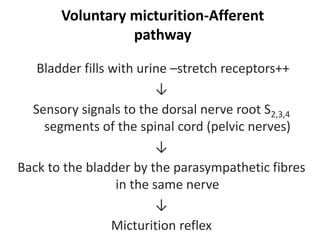
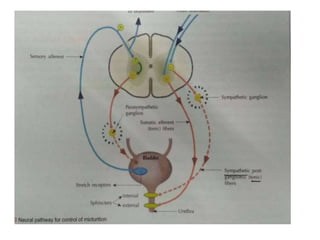
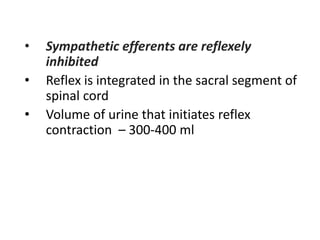
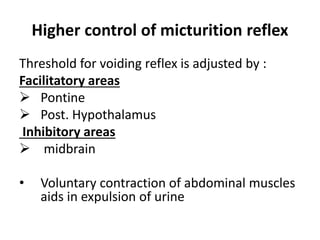
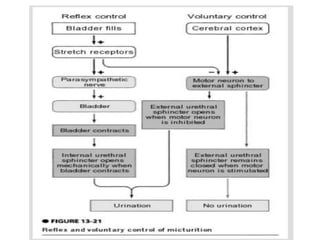
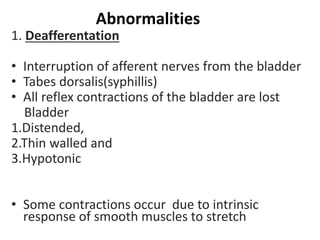
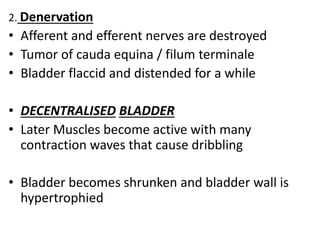
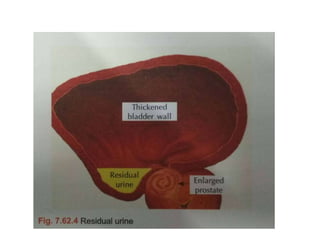
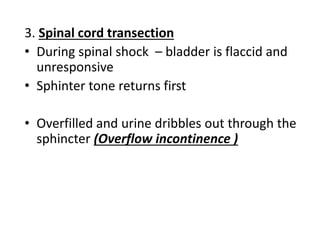
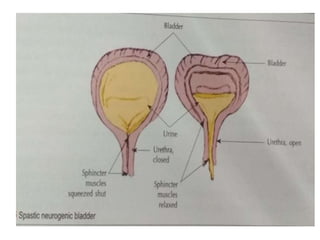
The urinary bladder stores urine and empties through micturition. It has a muscular wall and is innervated by both the autonomic and somatic nervous systems. During filling, afferent nerves signal bladder fullness to the spinal cord. Above 300-400ml, the micturition reflex is triggered, causing detrusor muscle contraction and internal sphincter relaxation for voiding. Higher brain centers can facilitate or inhibit this reflex. Abnormalities like denervation can cause an overactive or underactive bladder unable to empty fully.