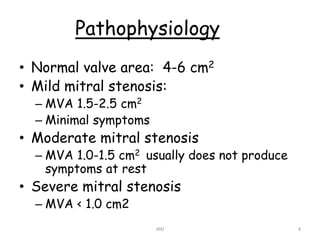
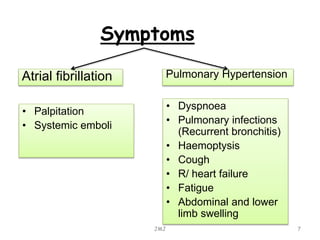
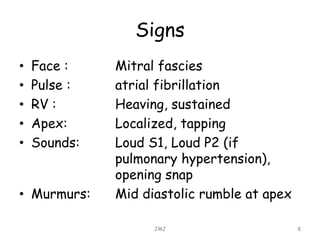
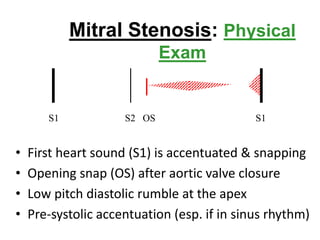
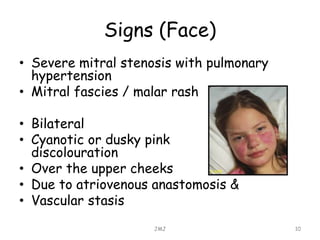
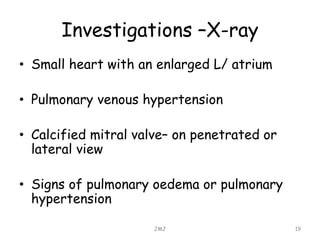
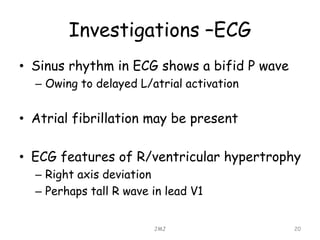
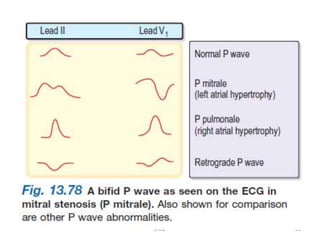
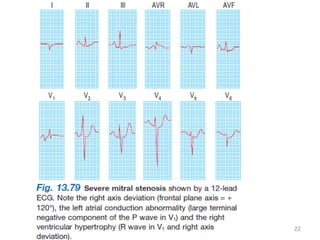
Mitral stenosis is commonly caused by rheumatic heart disease which leads to inflammation and fusion of the mitral valve leaflets, reducing the mitral valve orifice area. Severe mitral stenosis, defined as a mitral valve area less than 1.0 cm2, can cause pulmonary hypertension, pulmonary edema, atrial fibrillation, and right heart failure as the heart tries to maintain sufficient cardiac output against the back pressure. Physical exam may reveal signs of pulmonary hypertension like a loud pulmonary component to S2, as well as a tapping apex, opening snap, and mid-diastolic rumble on cardiac auscultation. Echocardiography can determine the severity of mitral stenosis and assess