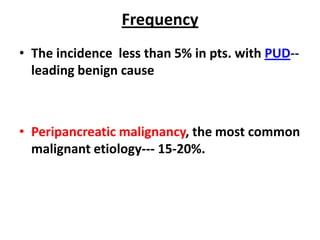
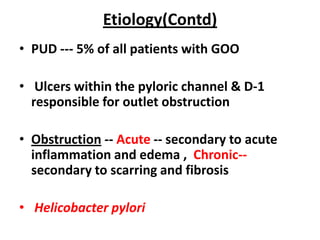
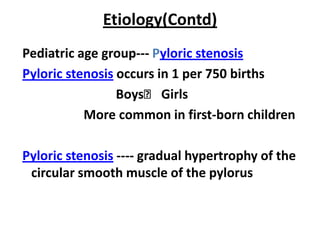
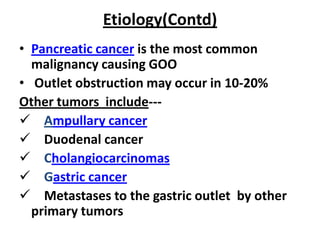
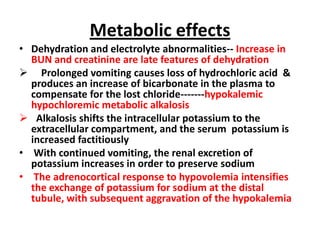
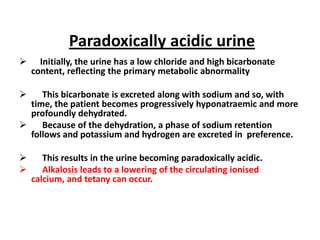
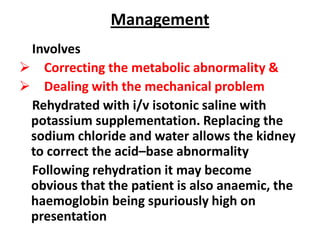
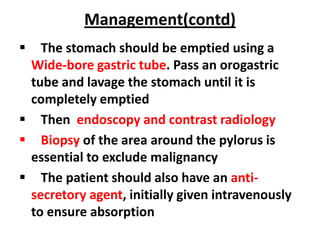
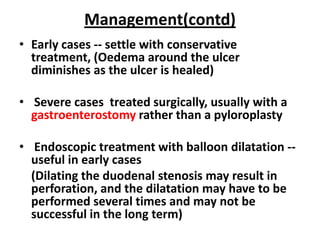
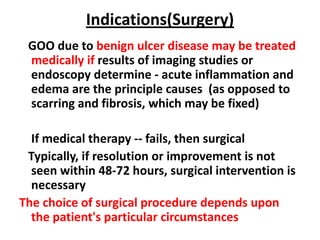
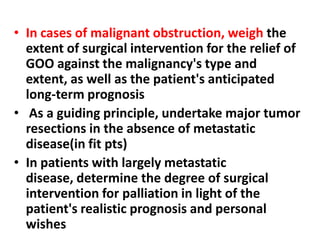
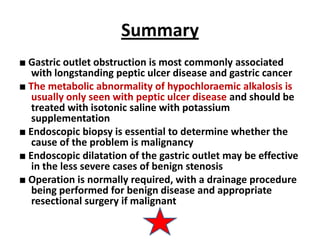
Gastric outlet obstruction is caused by benign or malignant diseases that obstruct gastric emptying. Common benign causes include peptic ulcer disease while pancreatic cancer is a frequent malignant cause. Patients experience nausea, vomiting and weight loss. Diagnosis involves distinguishing functional from mechanical causes and identifying the underlying etiology. Treatment focuses on rehydration and correcting metabolic abnormalities as well as addressing the mechanical obstruction through endoscopic or surgical interventions.