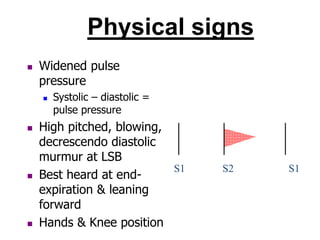
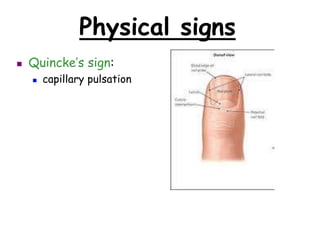
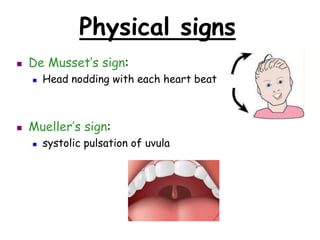
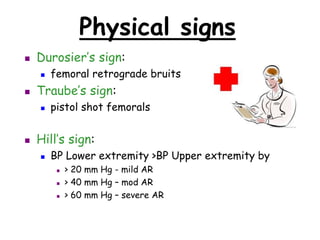
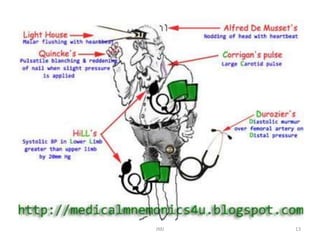
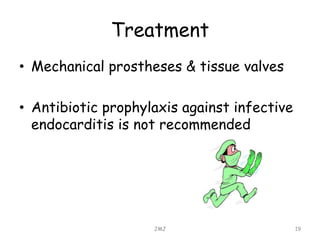
This document discusses atrial regurgitation, including its causes, pathophysiology, symptoms, signs, investigations, and treatment. It can be caused by diseases of the aortic valve like endocarditis or conditions affecting the aortic root like Marfan's syndrome. The pathophysiology involves blood refluxing from the aorta back into the left ventricle during diastole, enlarging the ventricle. Symptoms typically only develop late due to left ventricular failure and include angina and dyspnea. Physical exam may reveal a bounding pulse, displaced apex, and diastolic murmur. Investigations like echocardiogram can confirm the diagnosis. Treatment focuses on the underlying cause, and surgery is