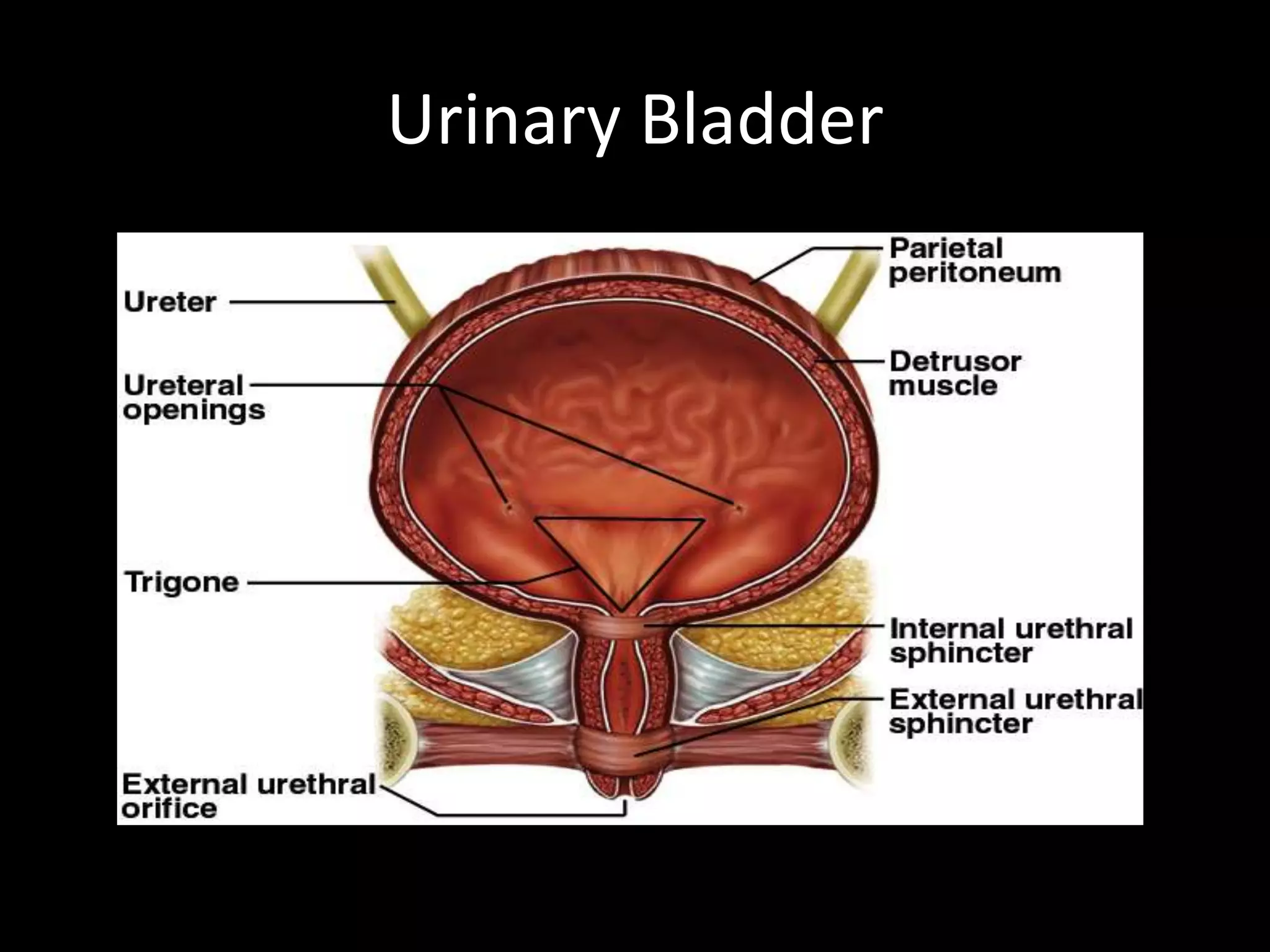
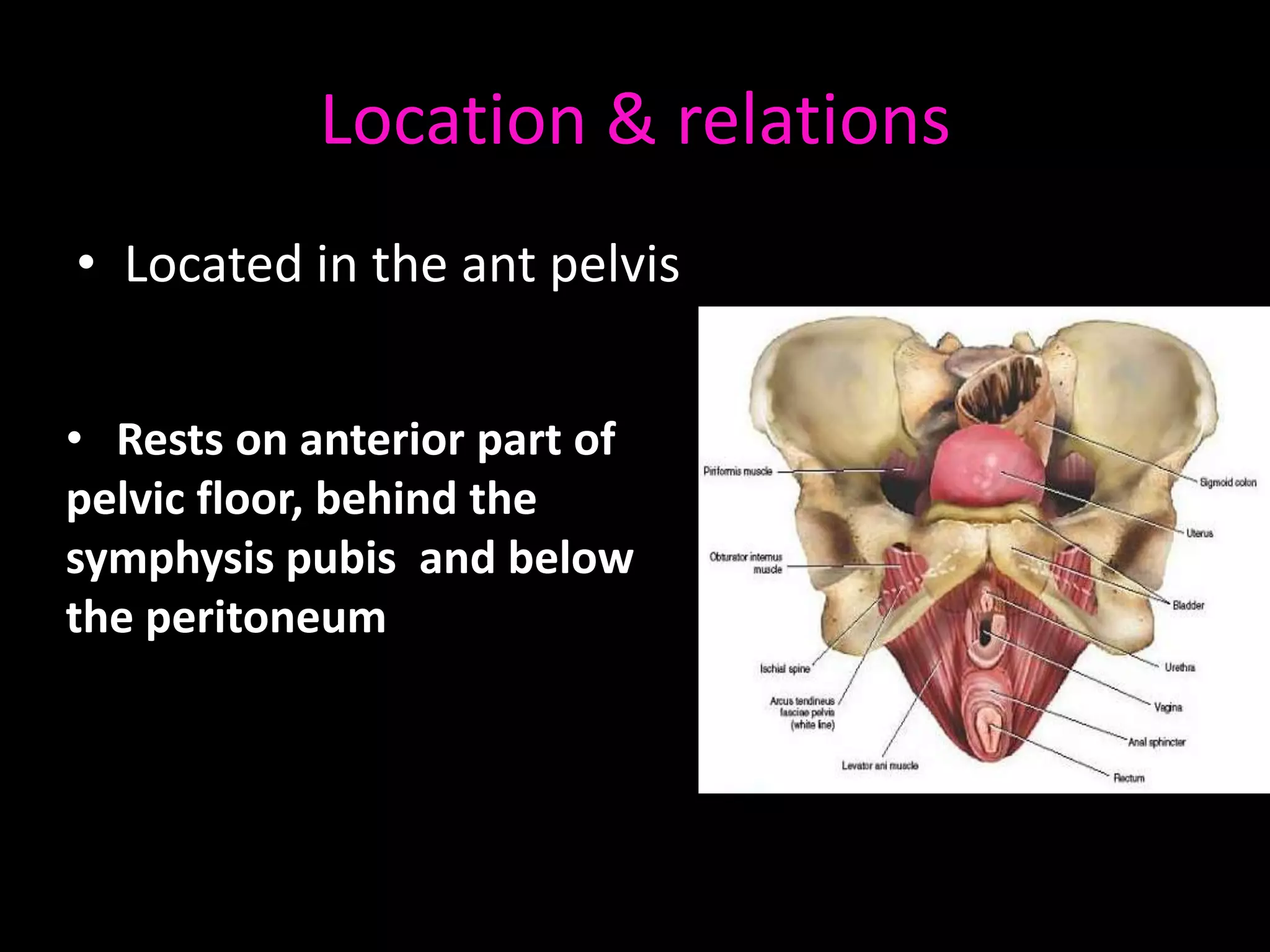
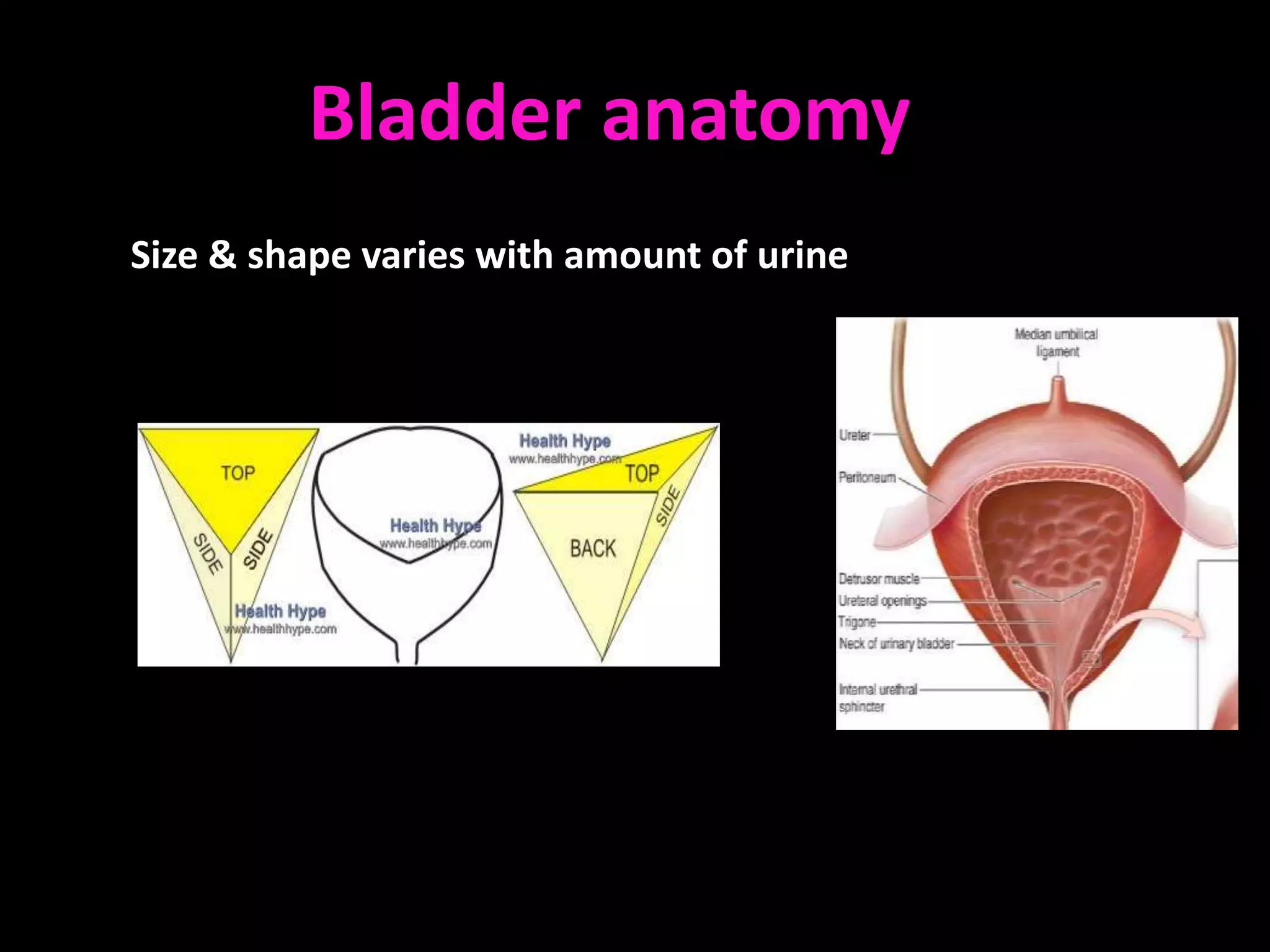
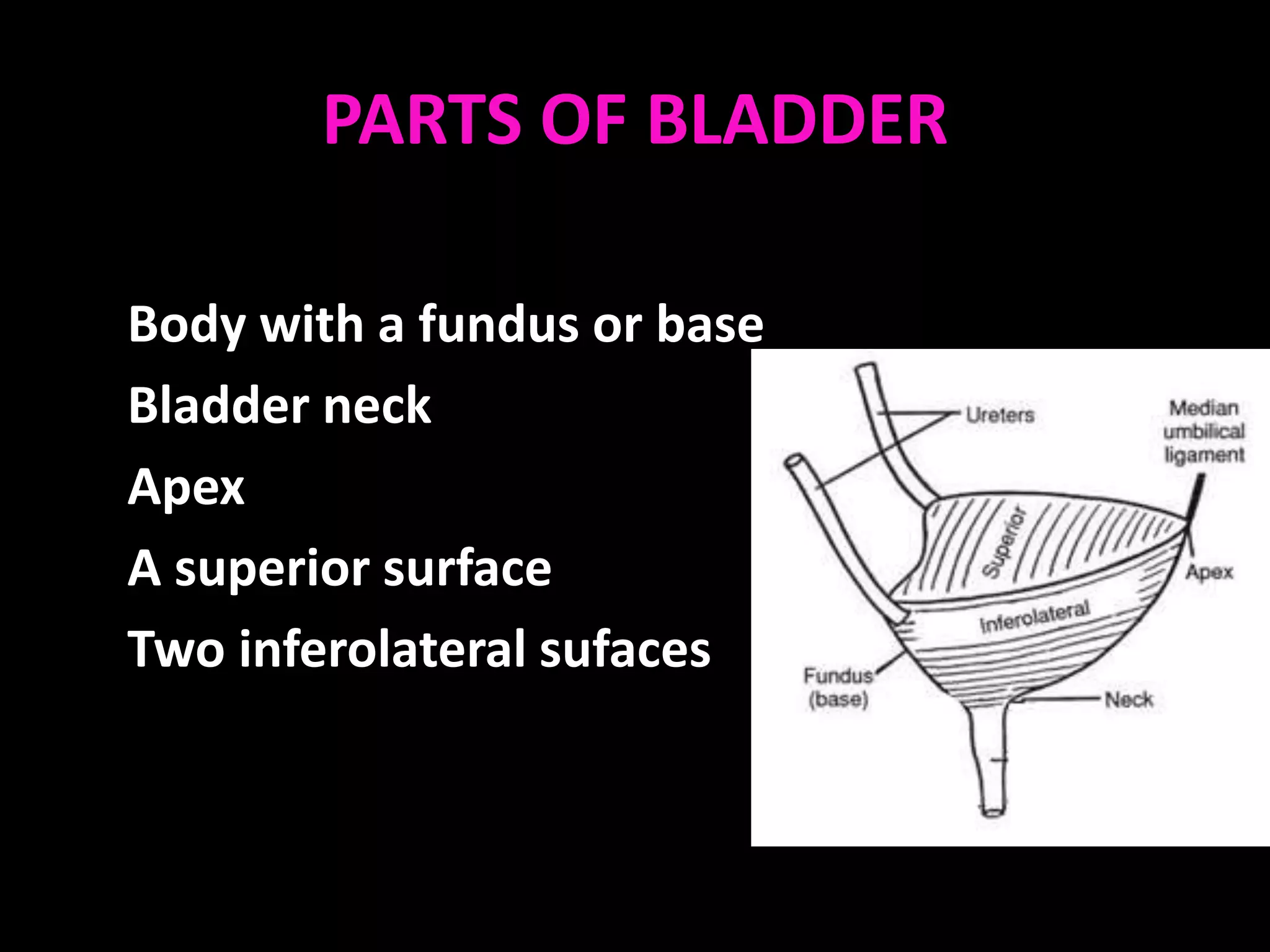
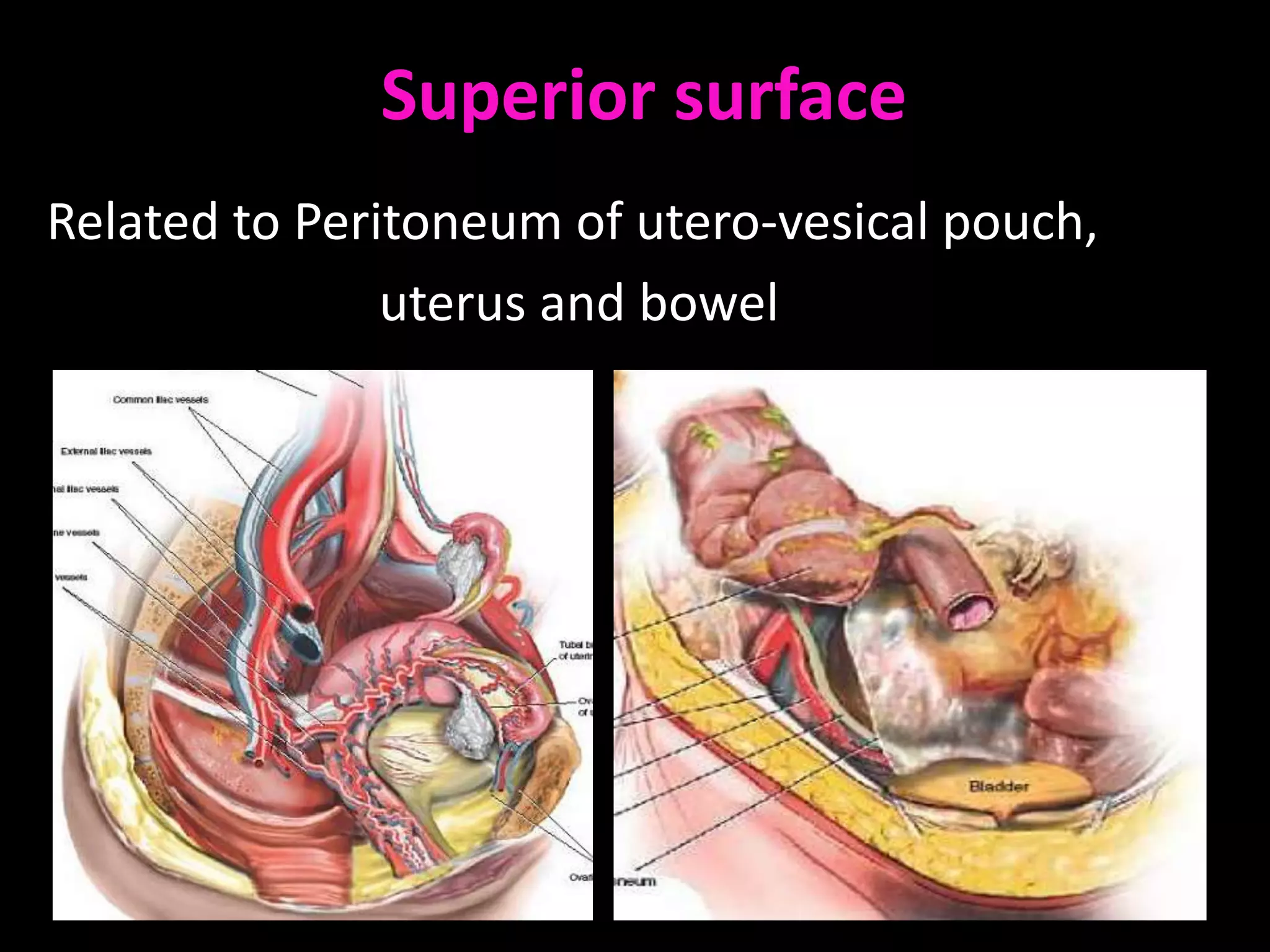
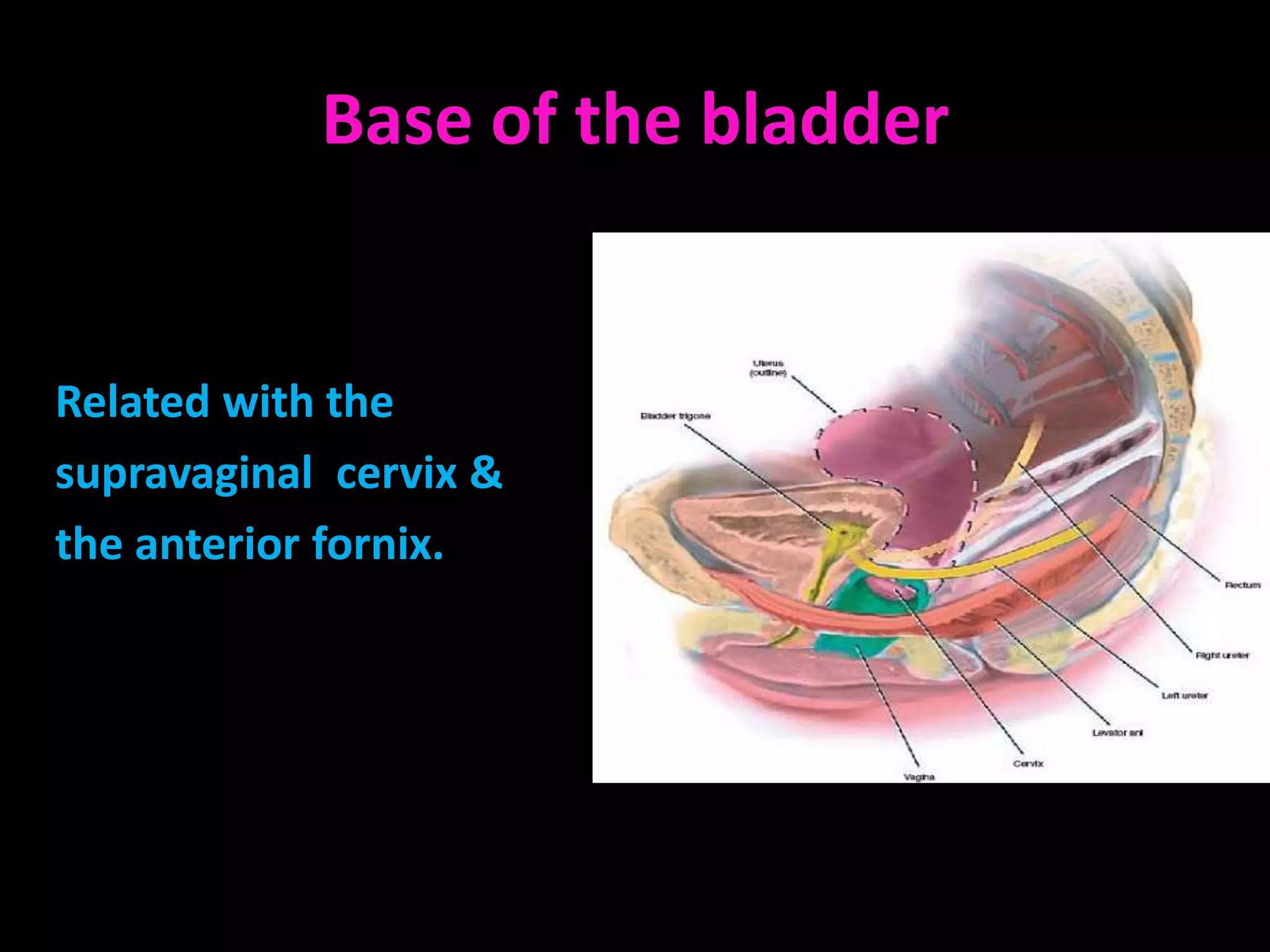
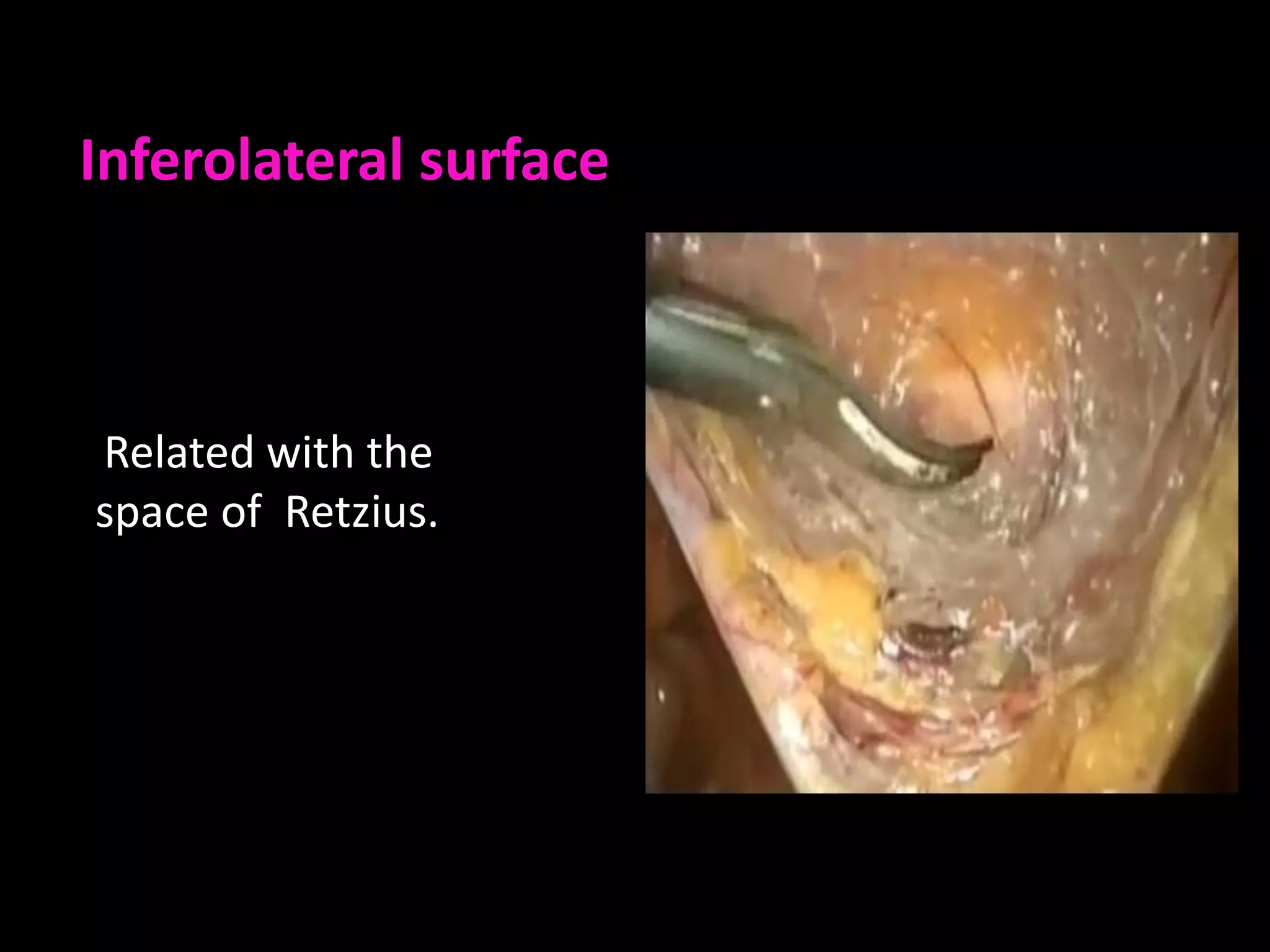
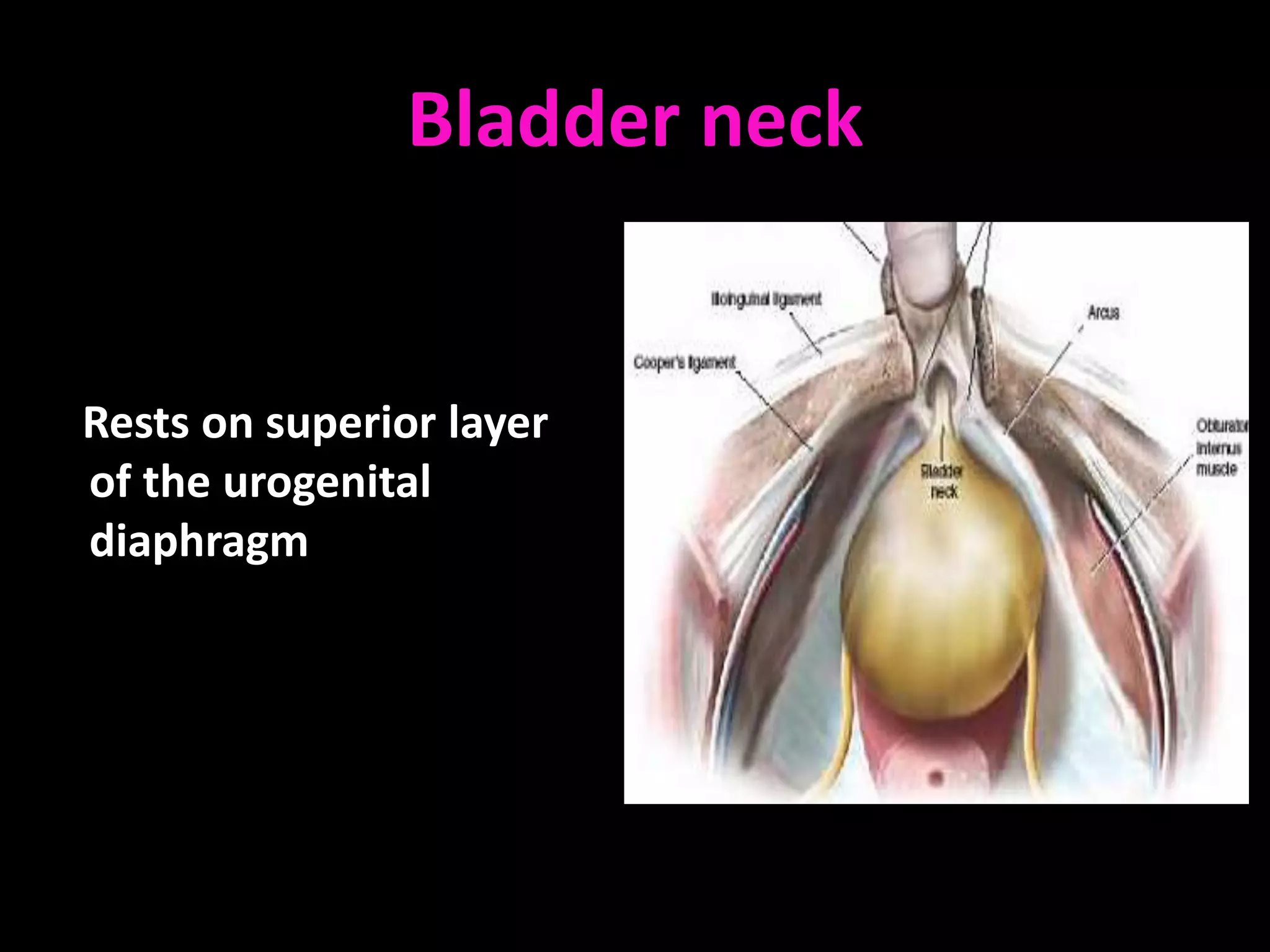
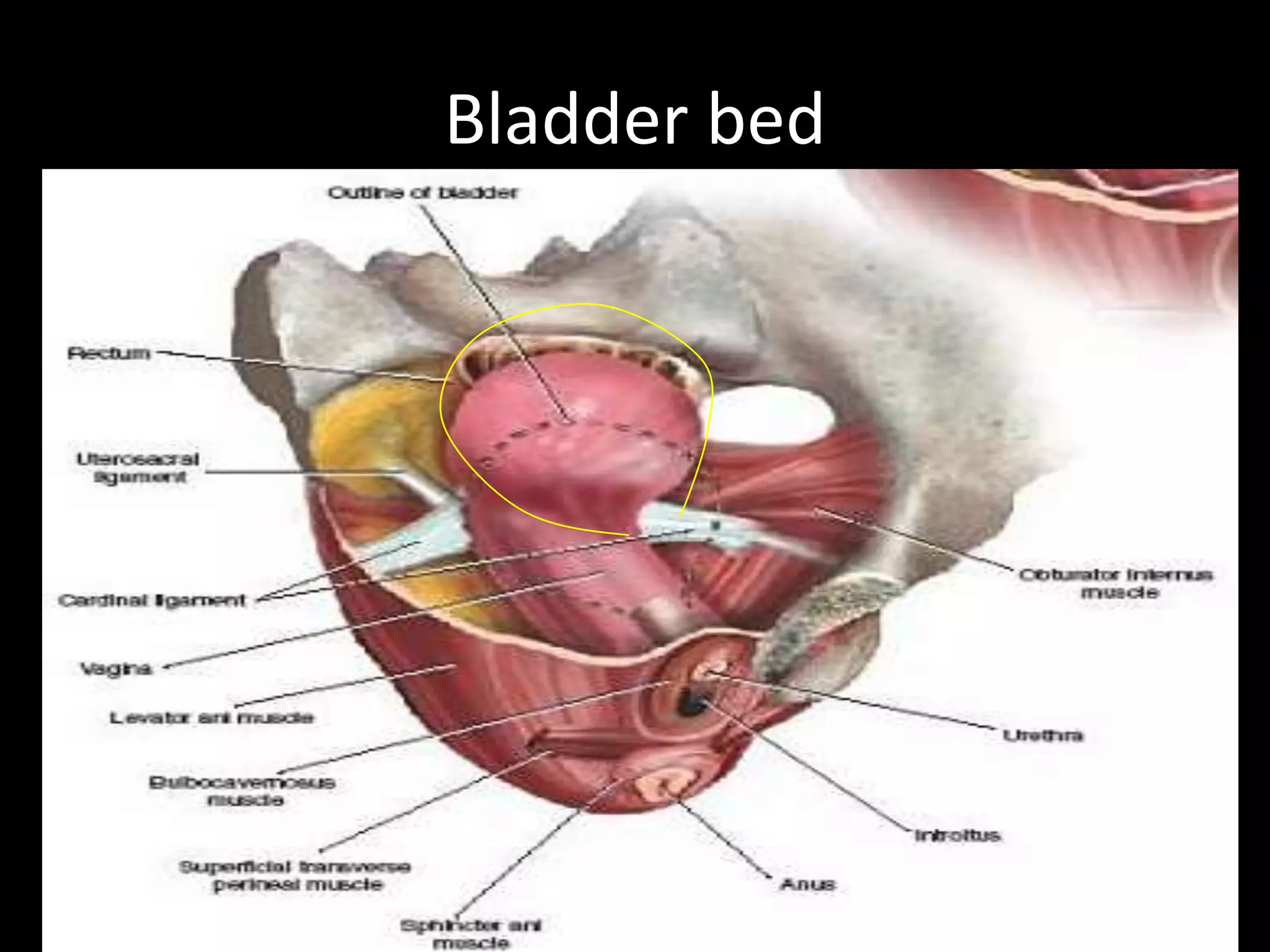
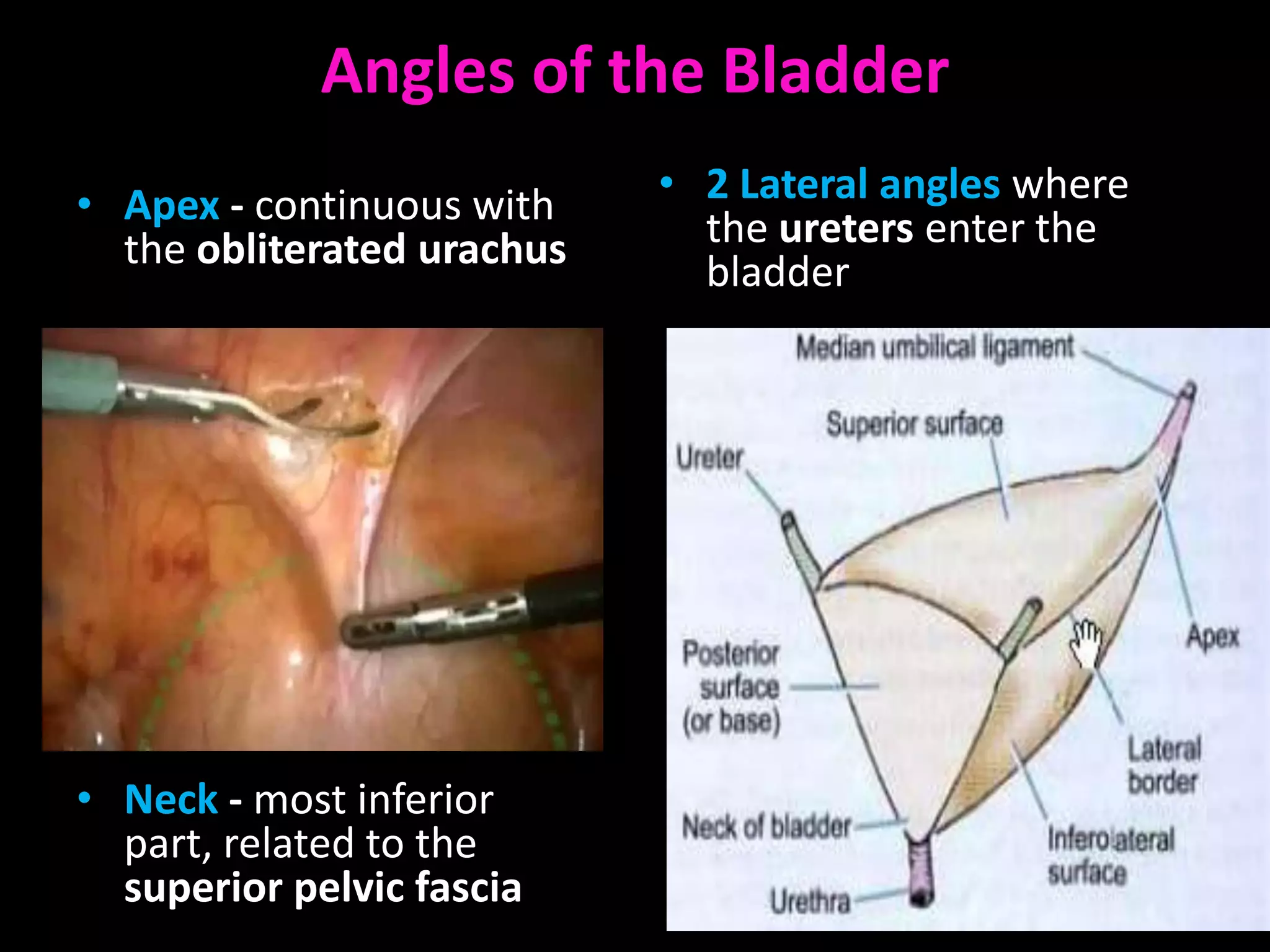
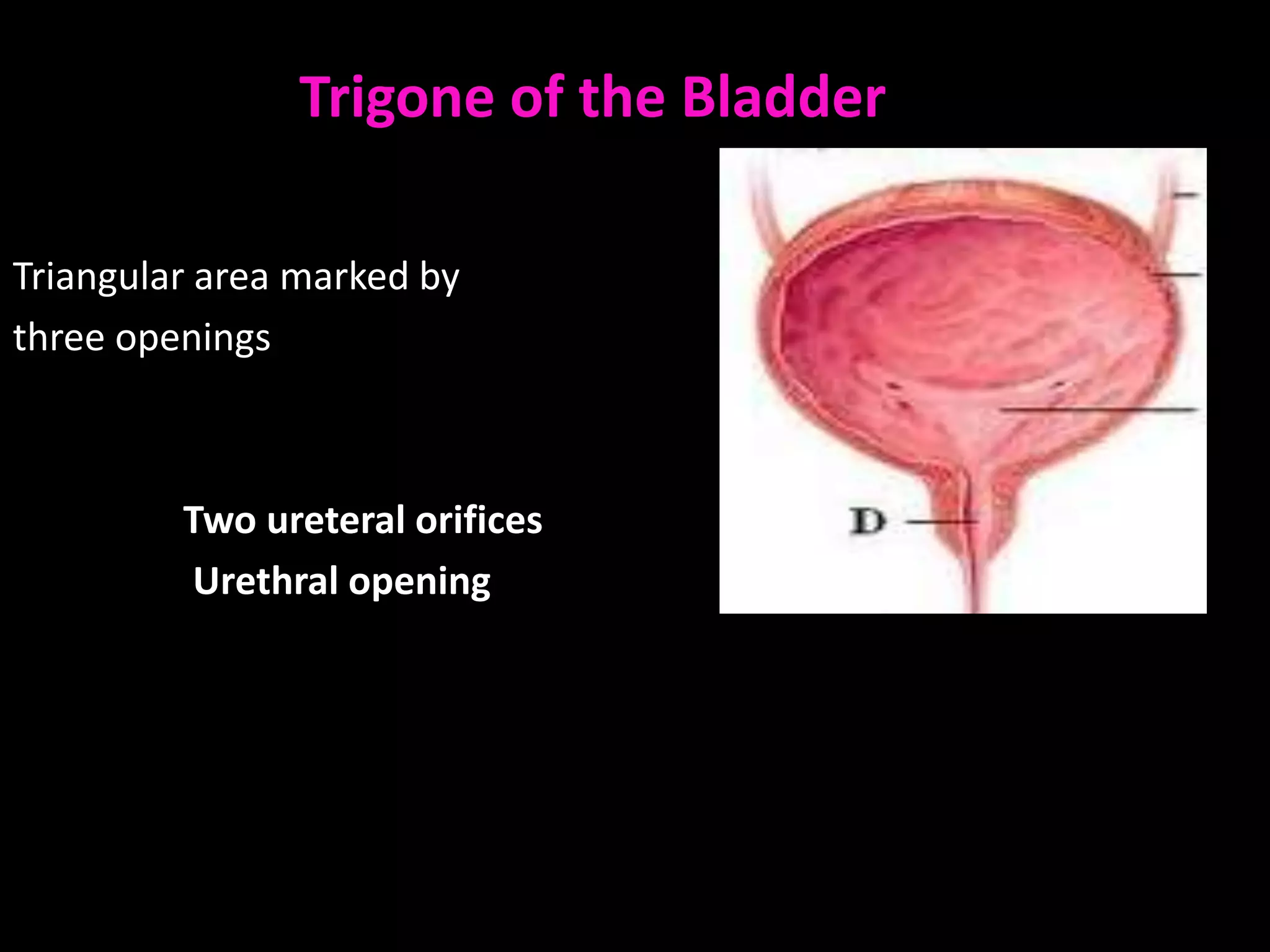
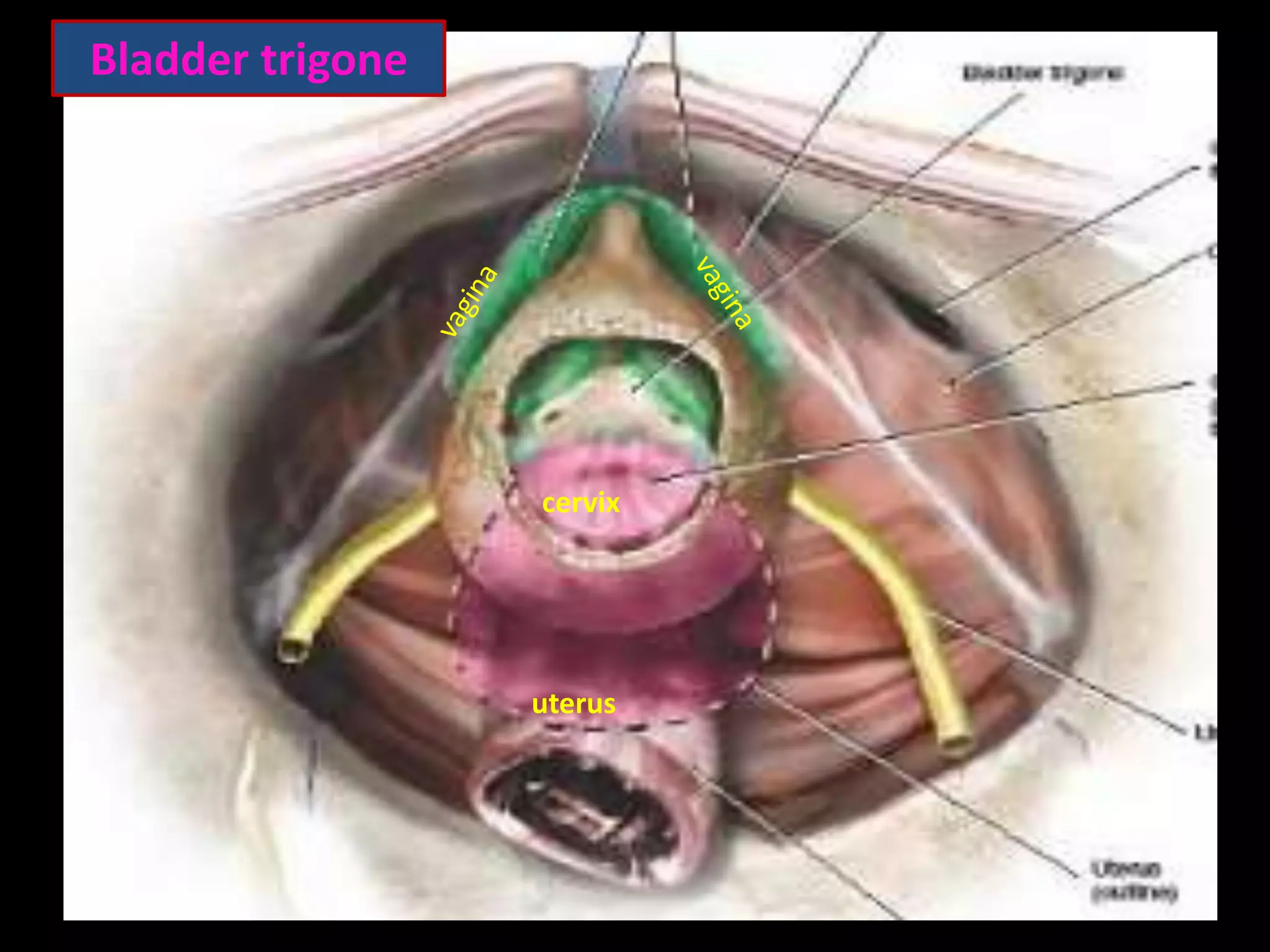
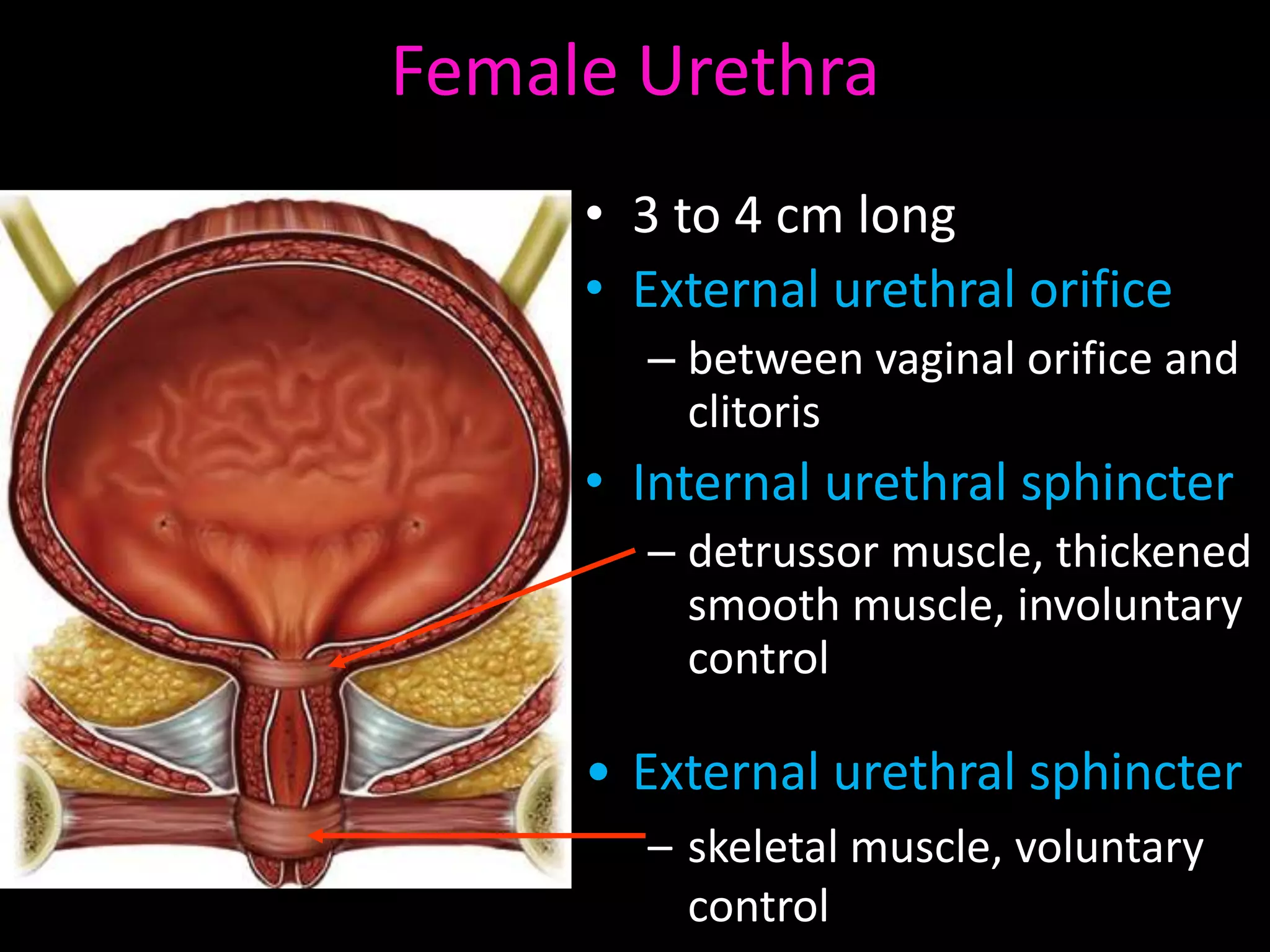
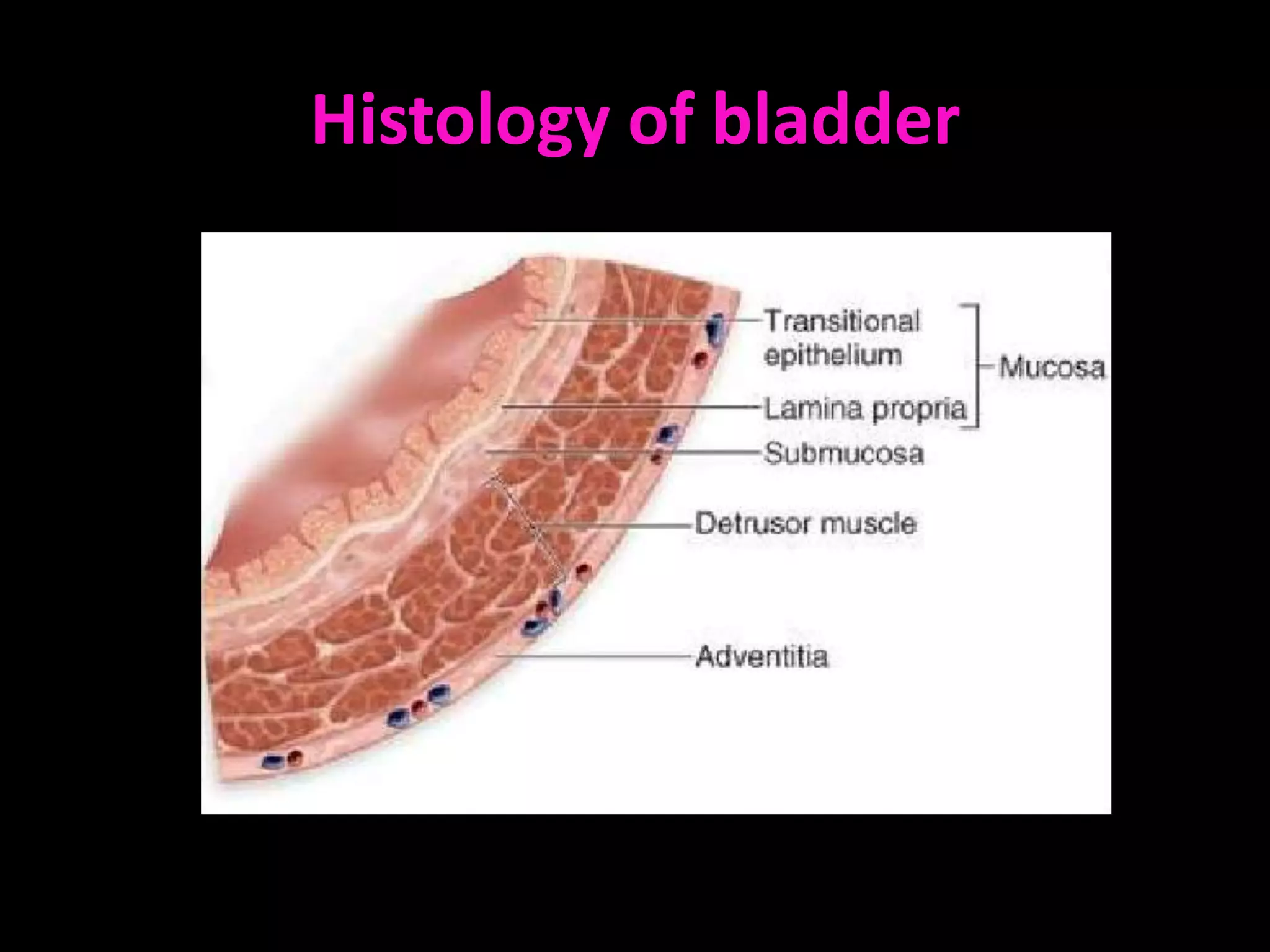
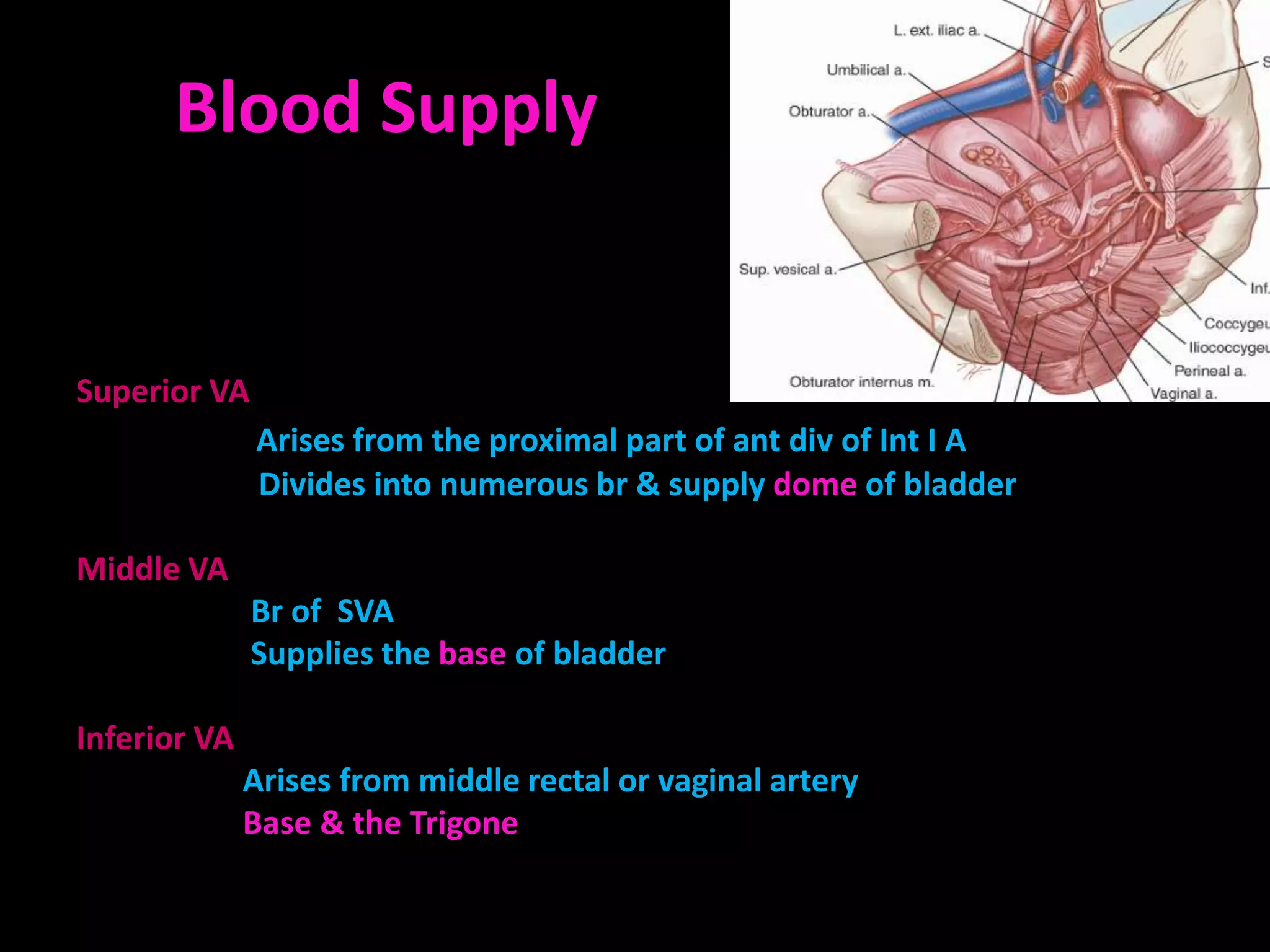
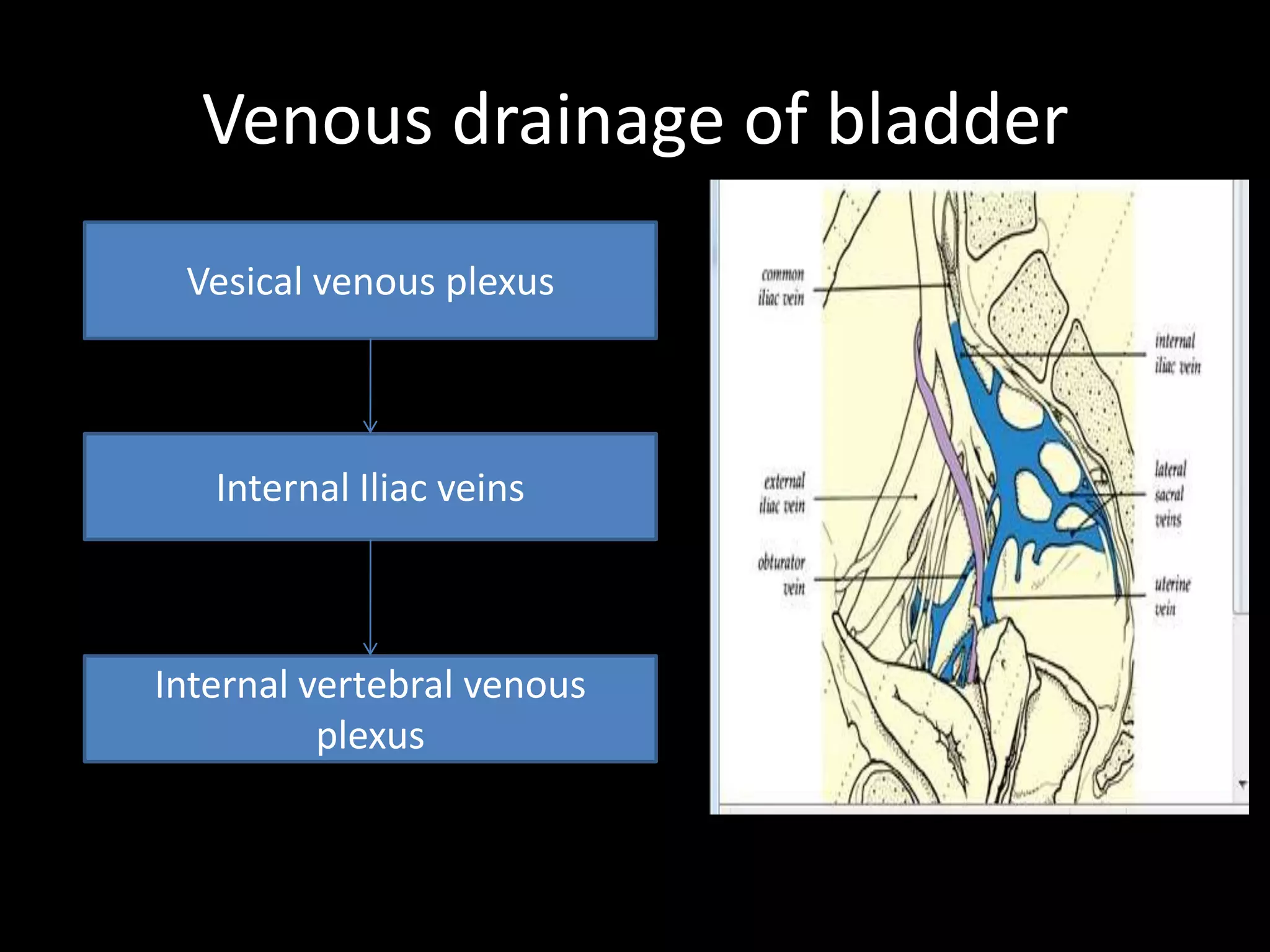
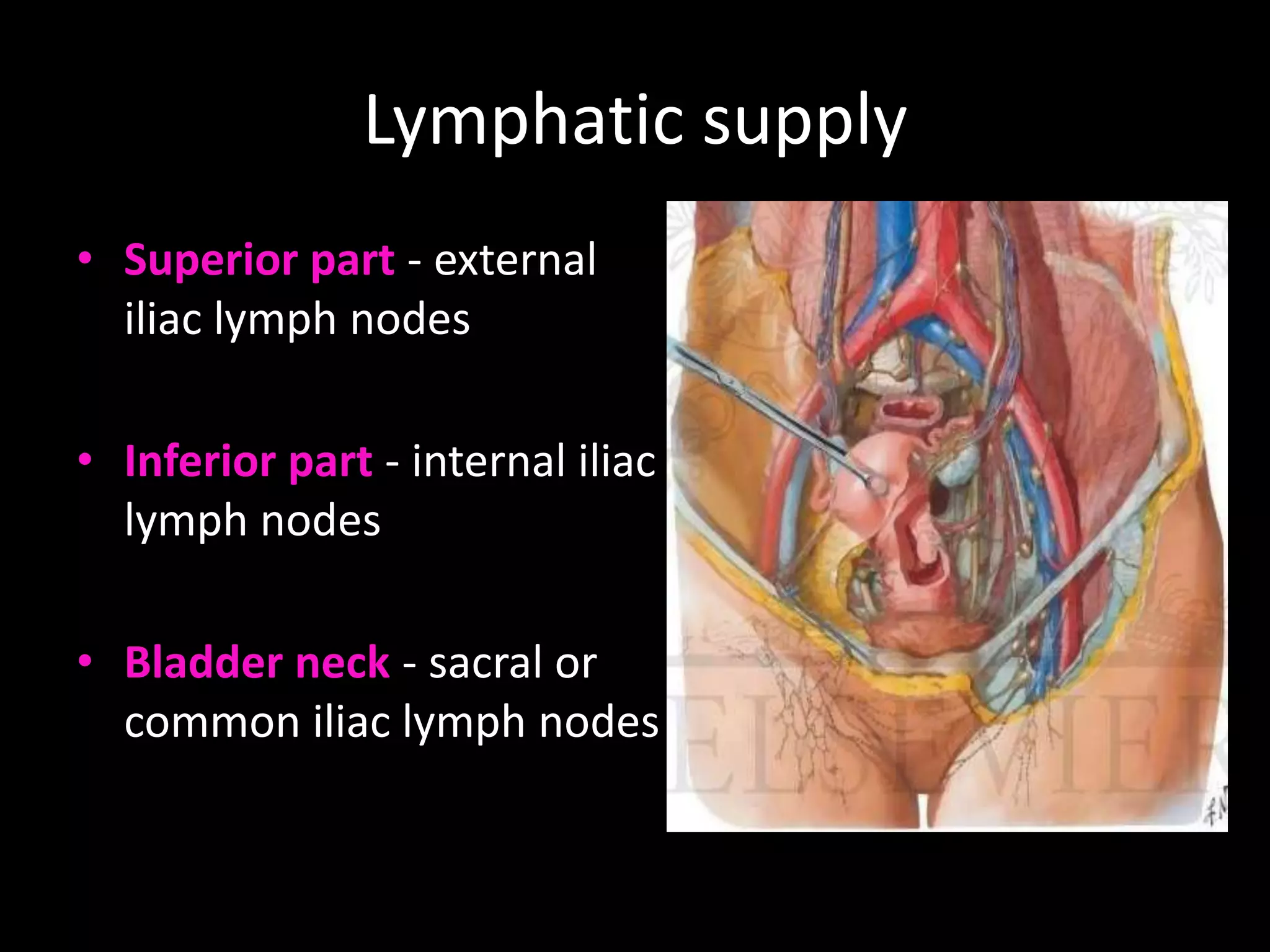
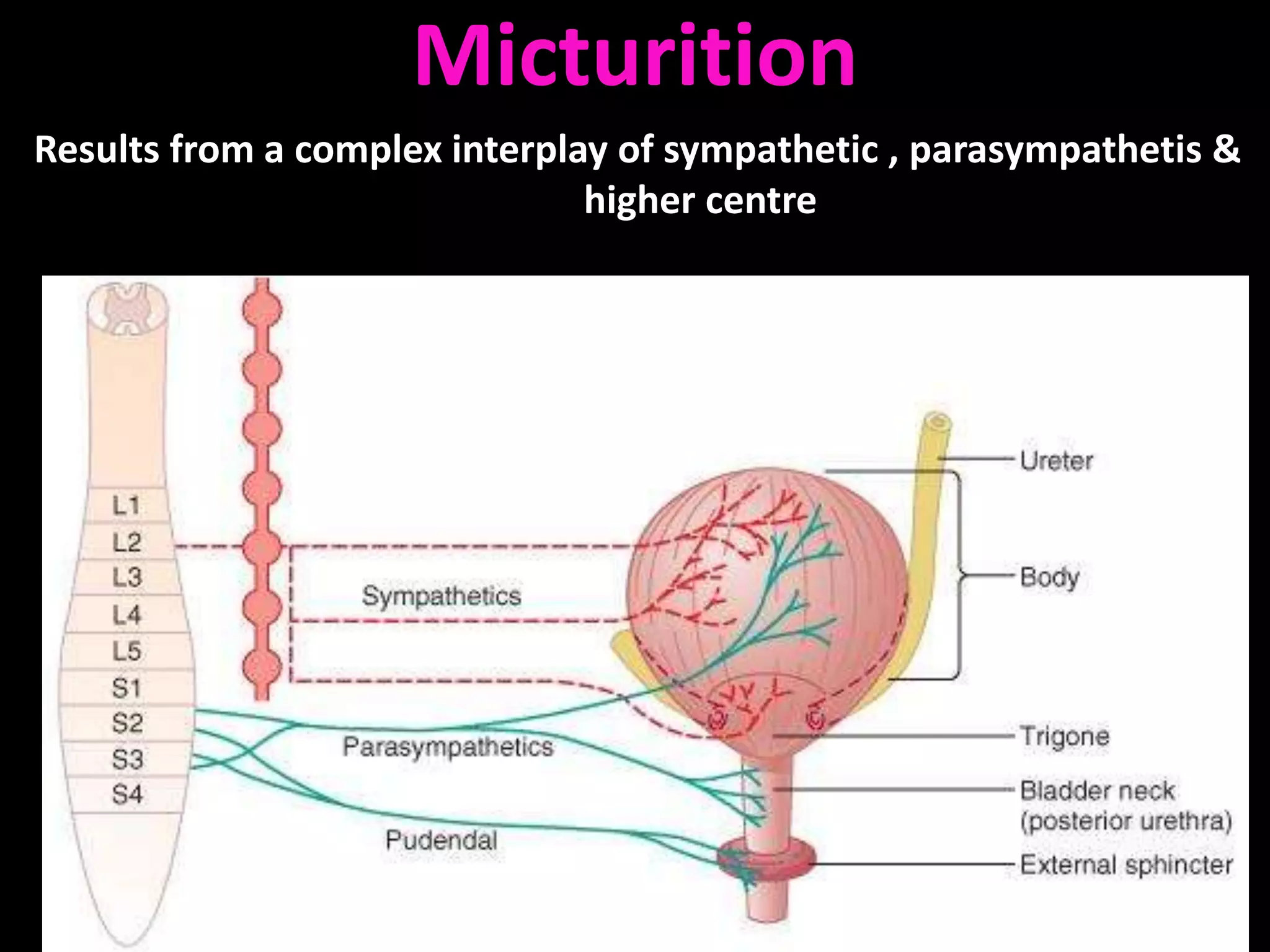
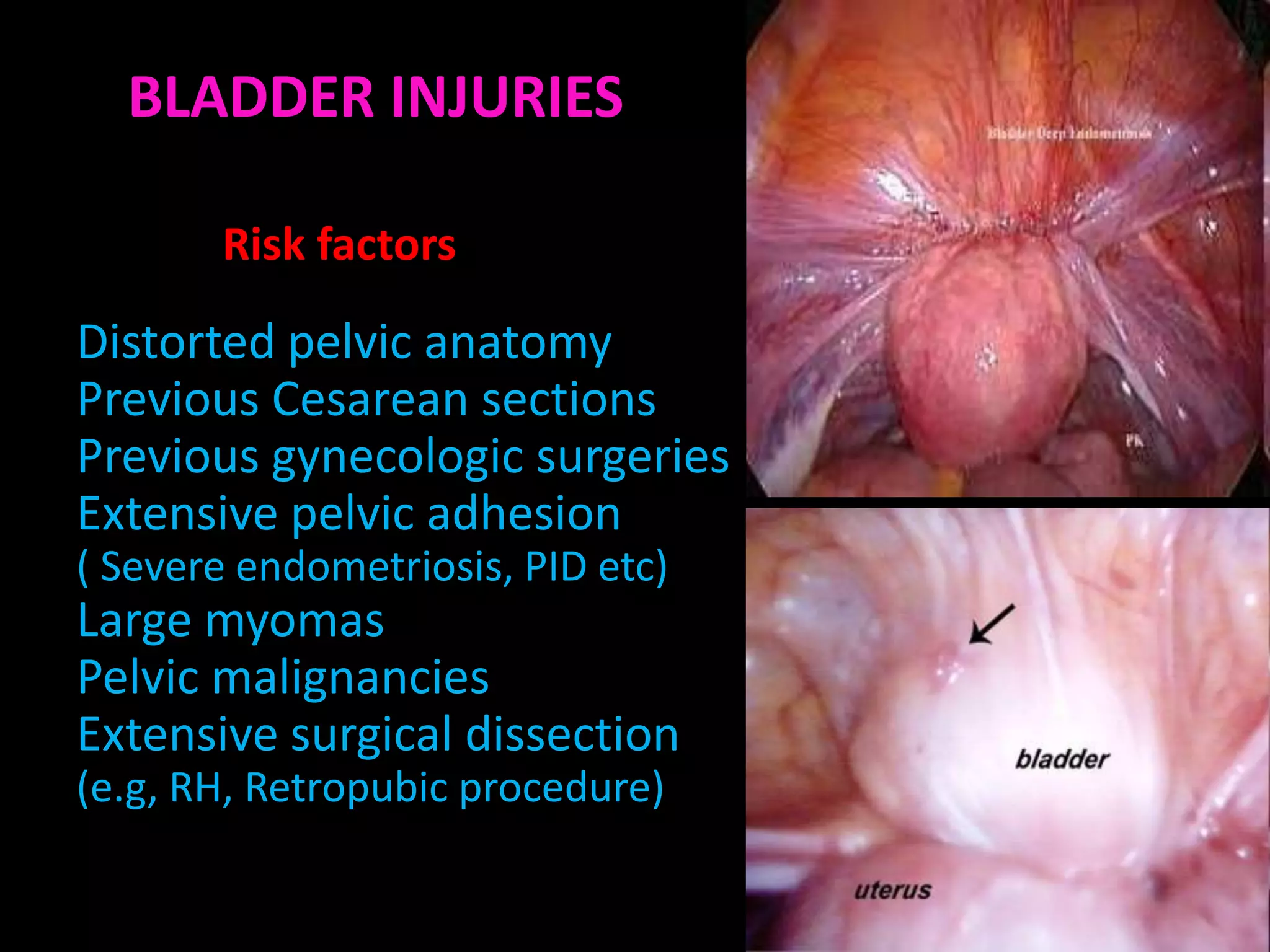
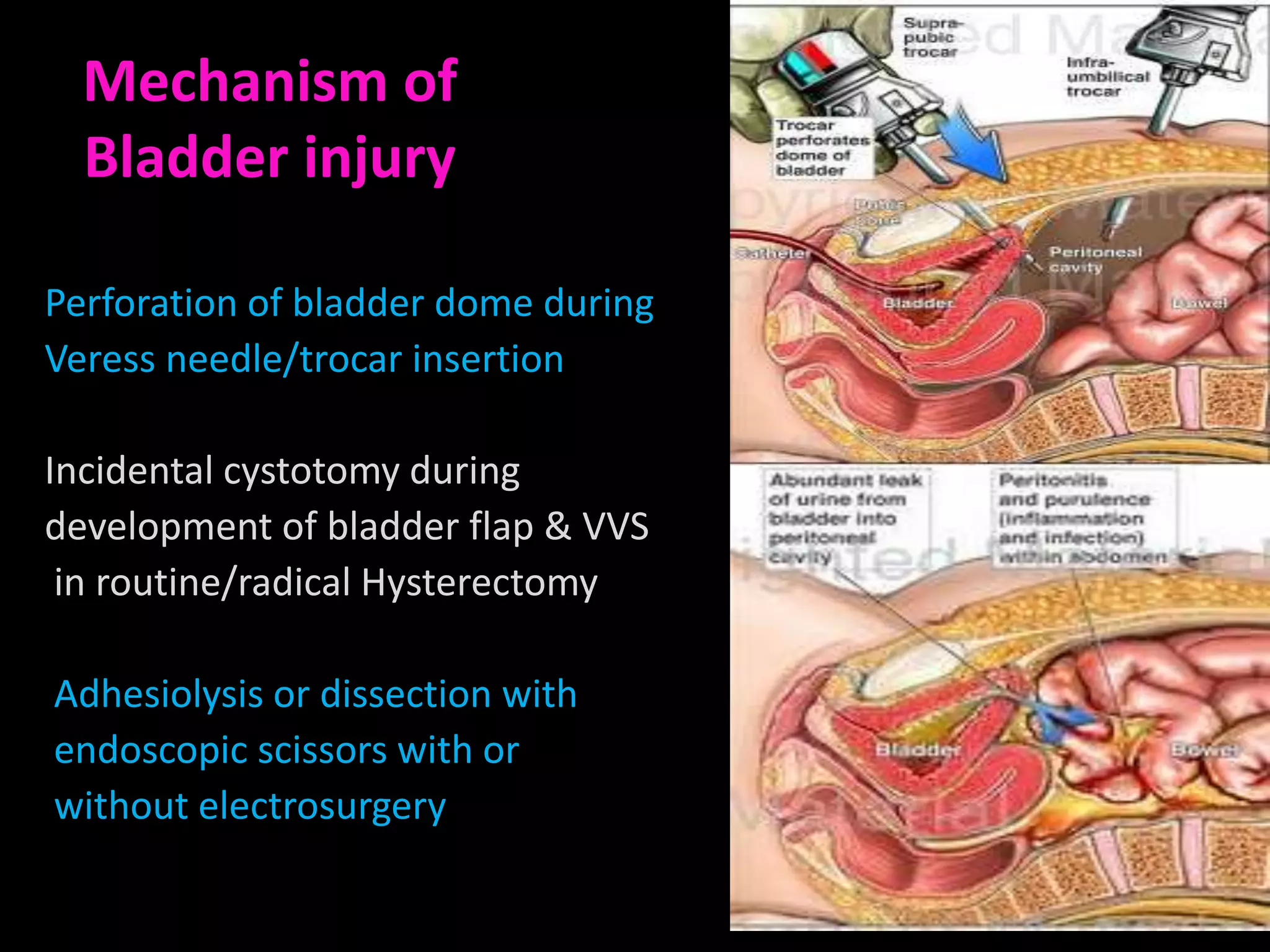
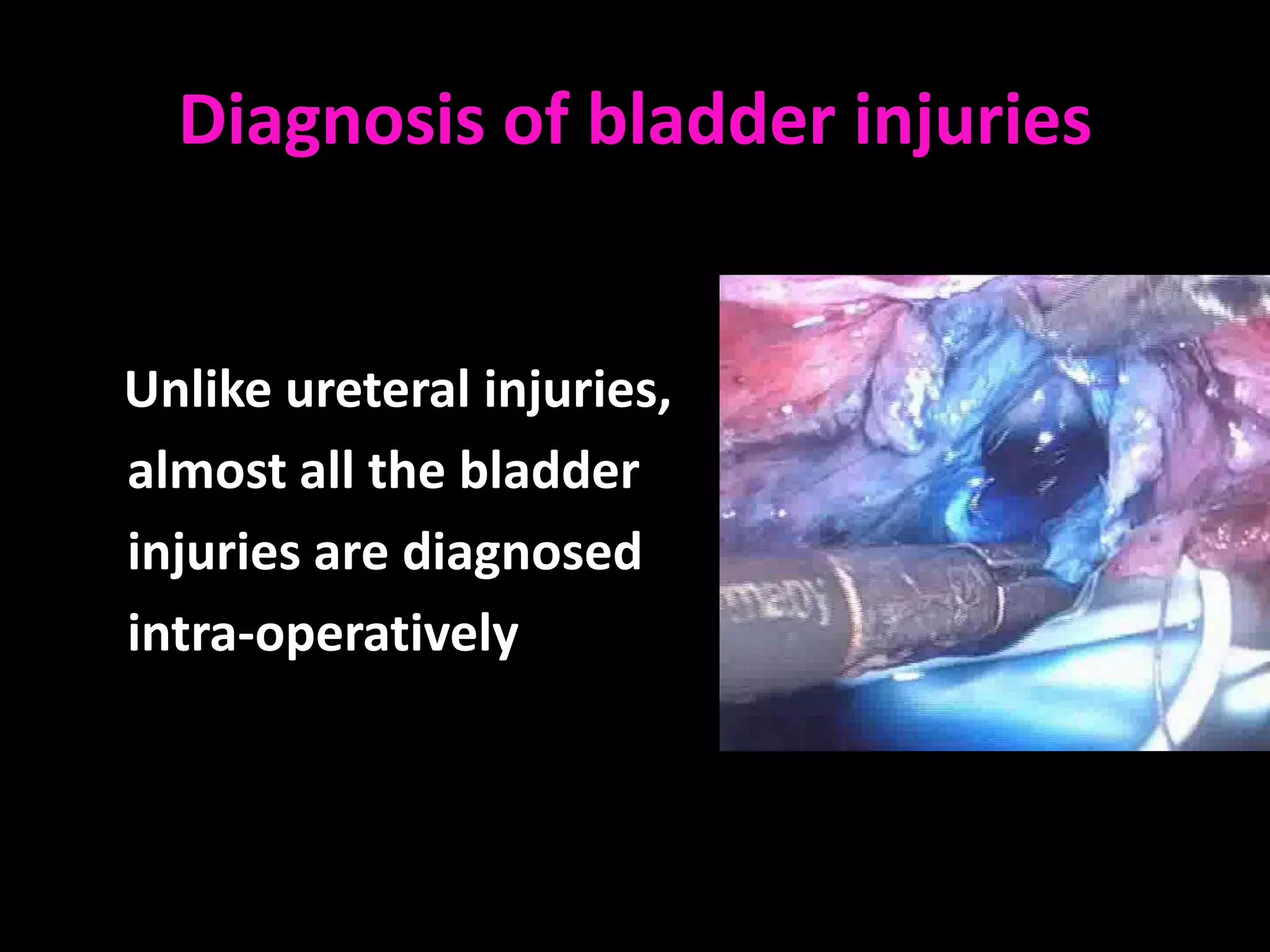
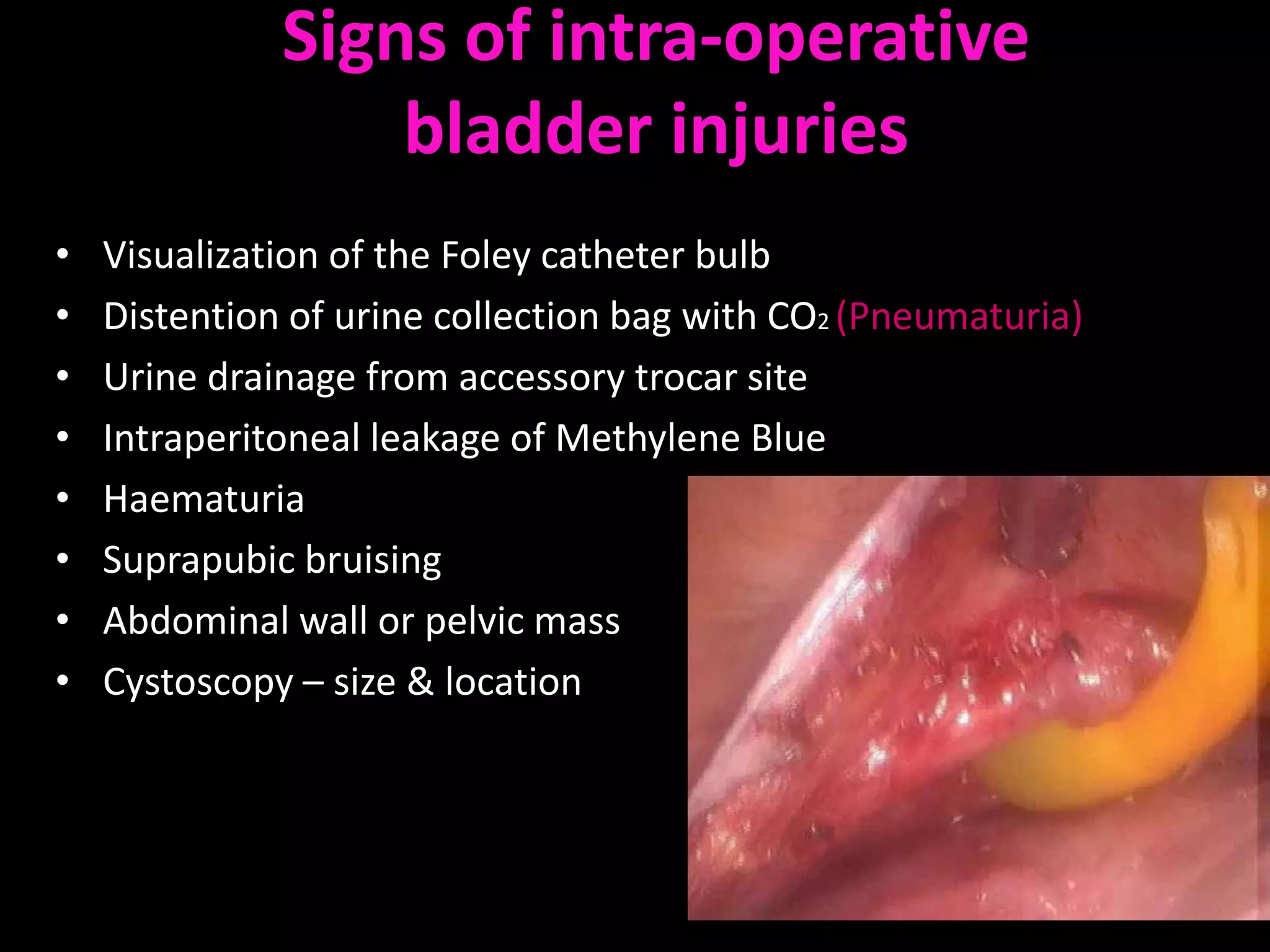
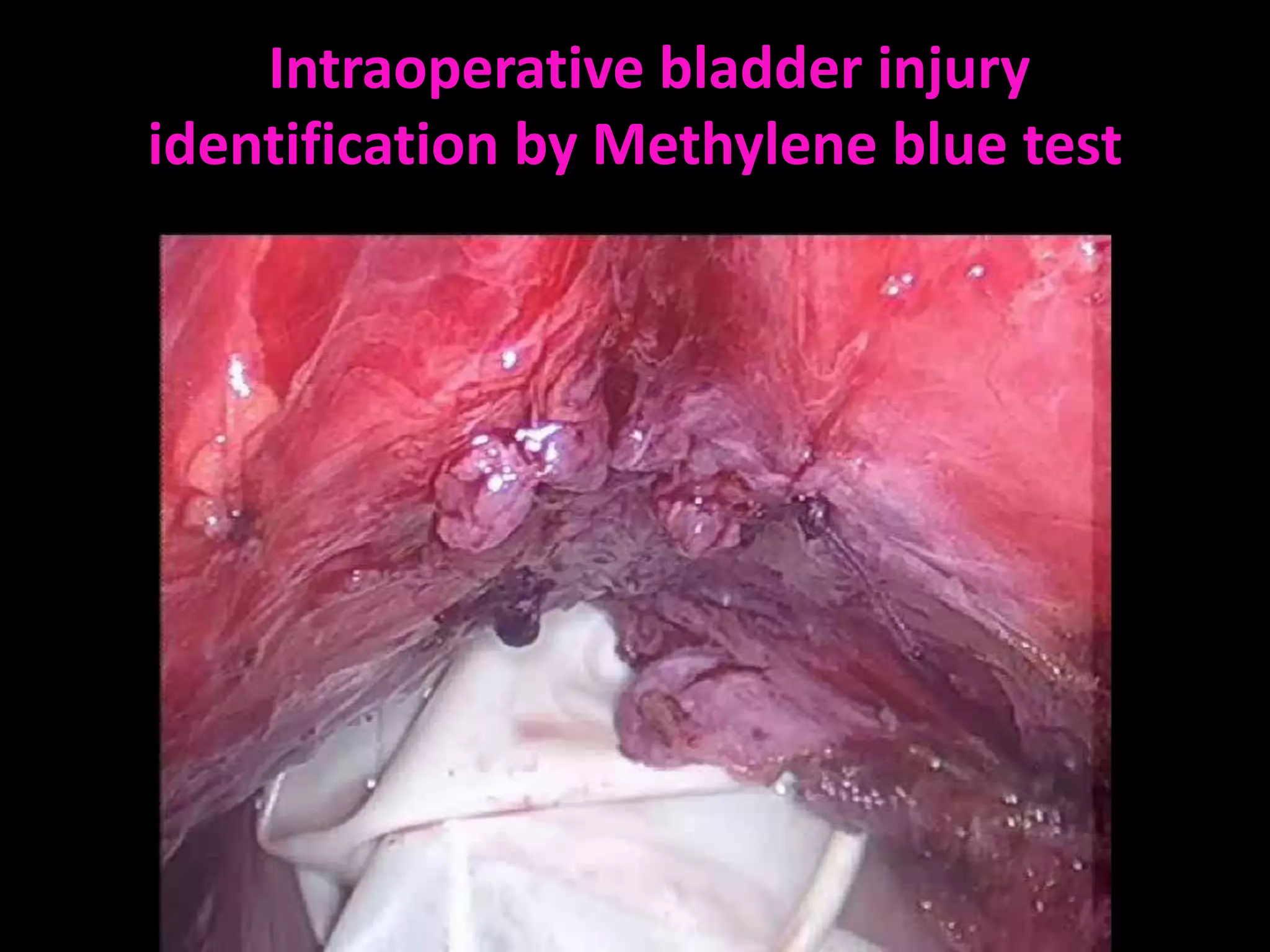
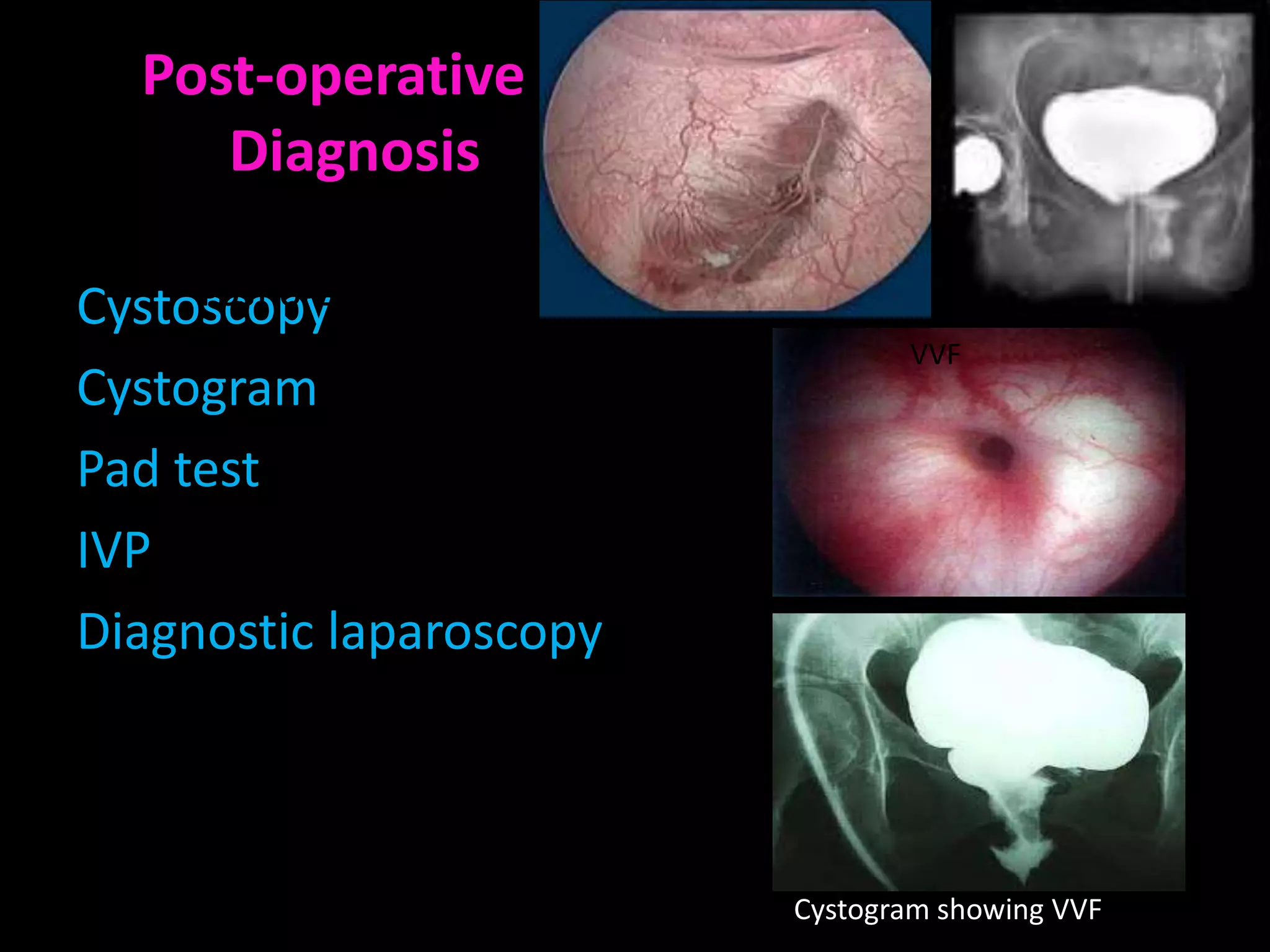
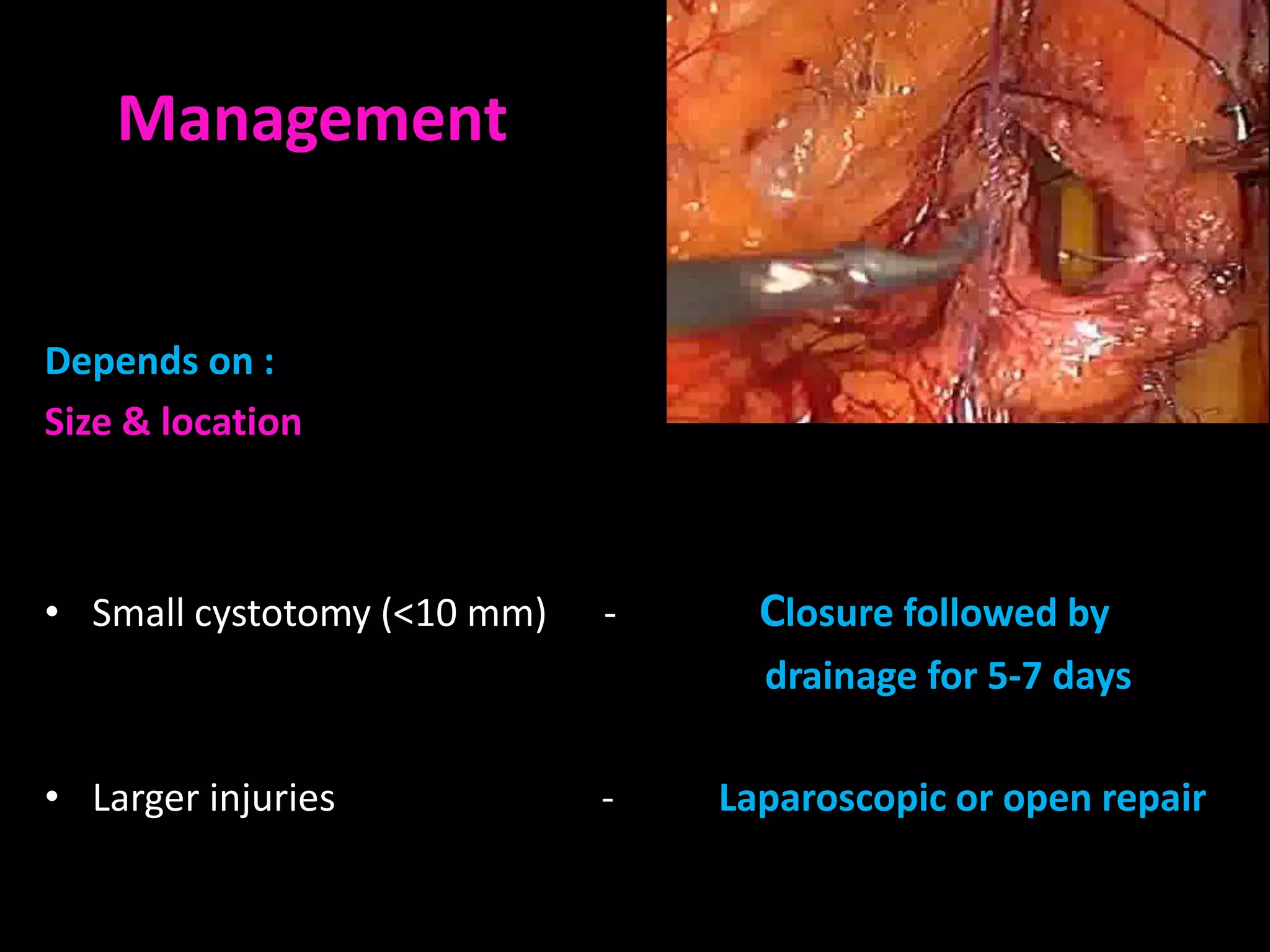
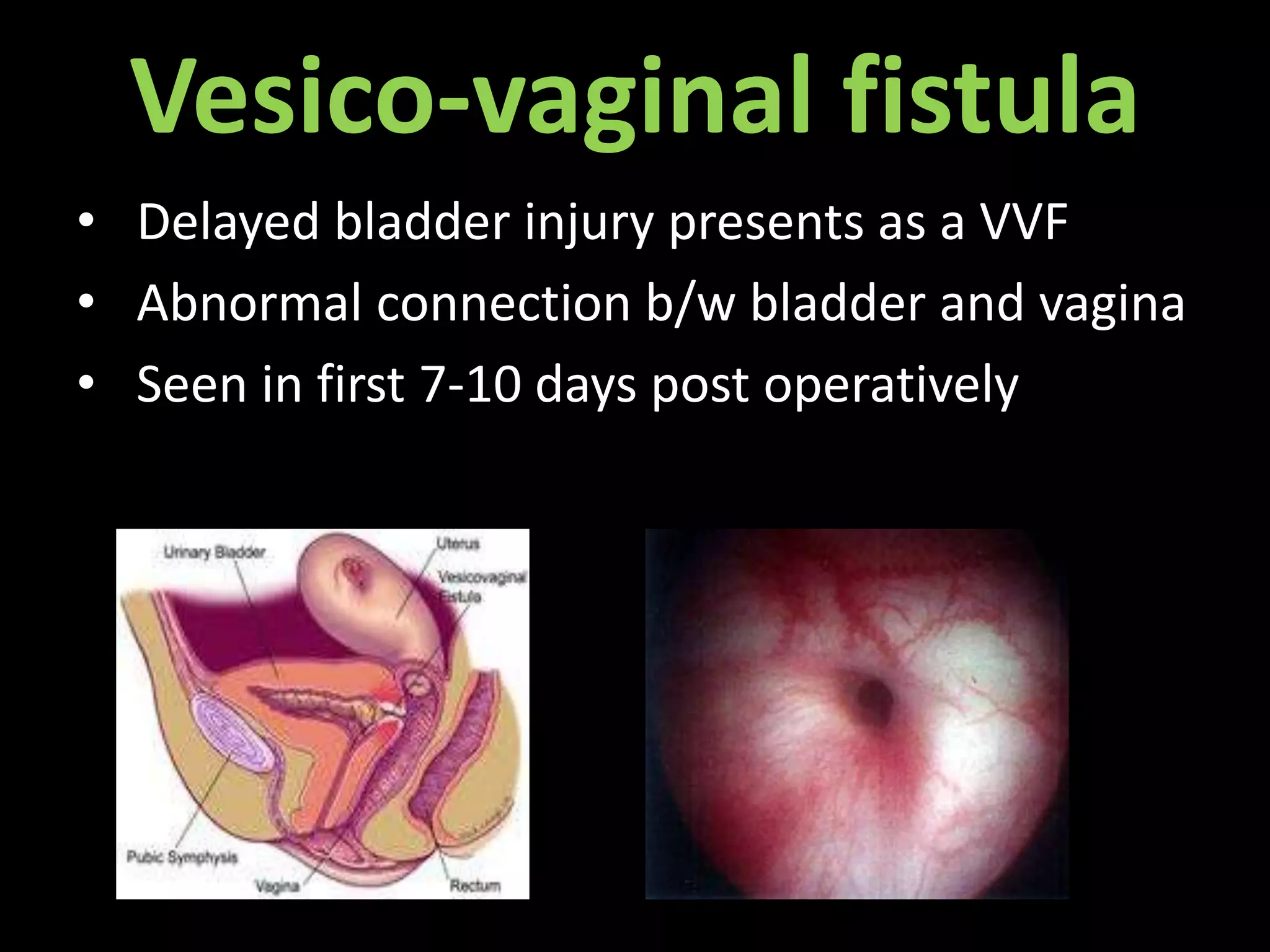
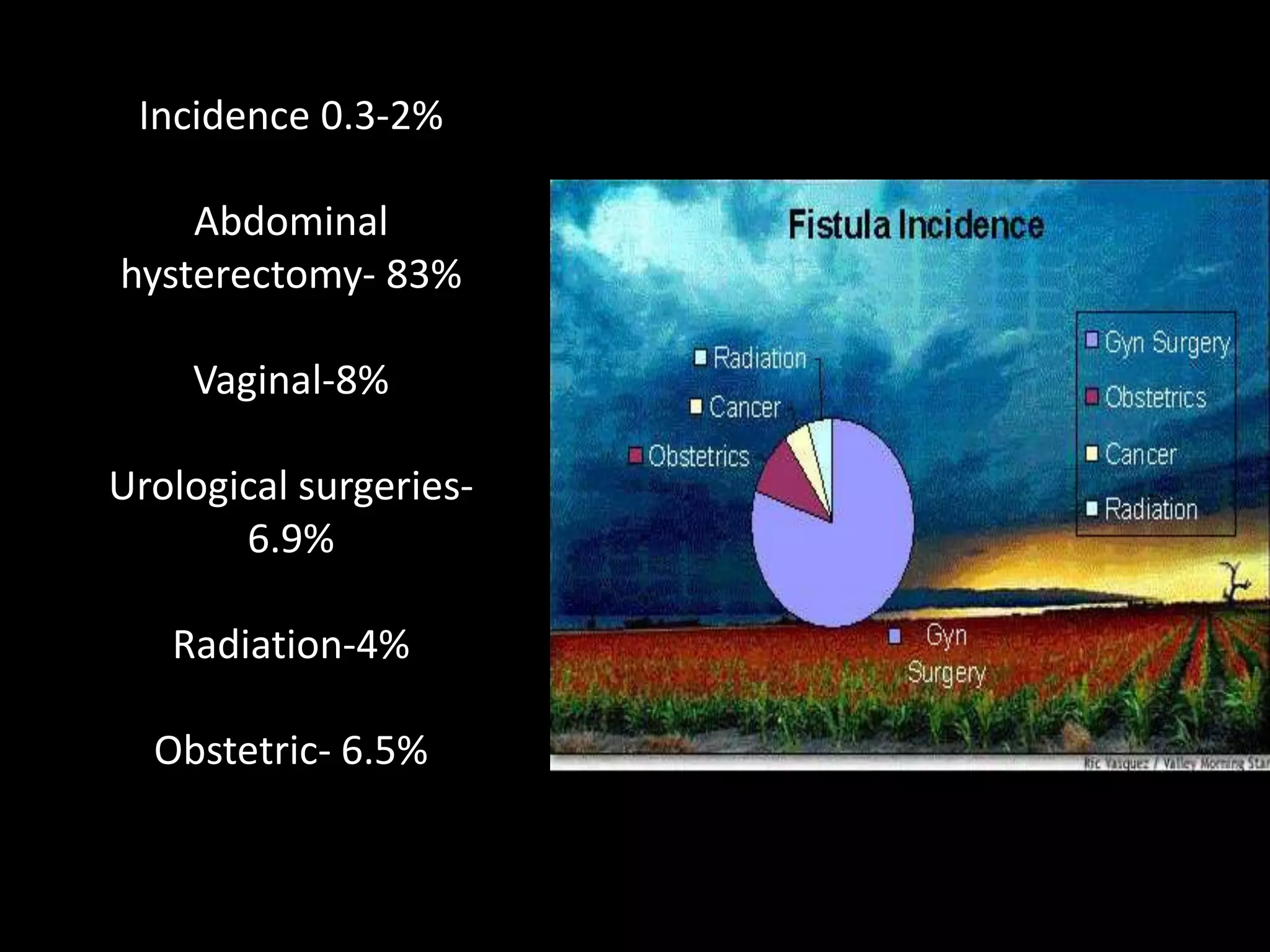
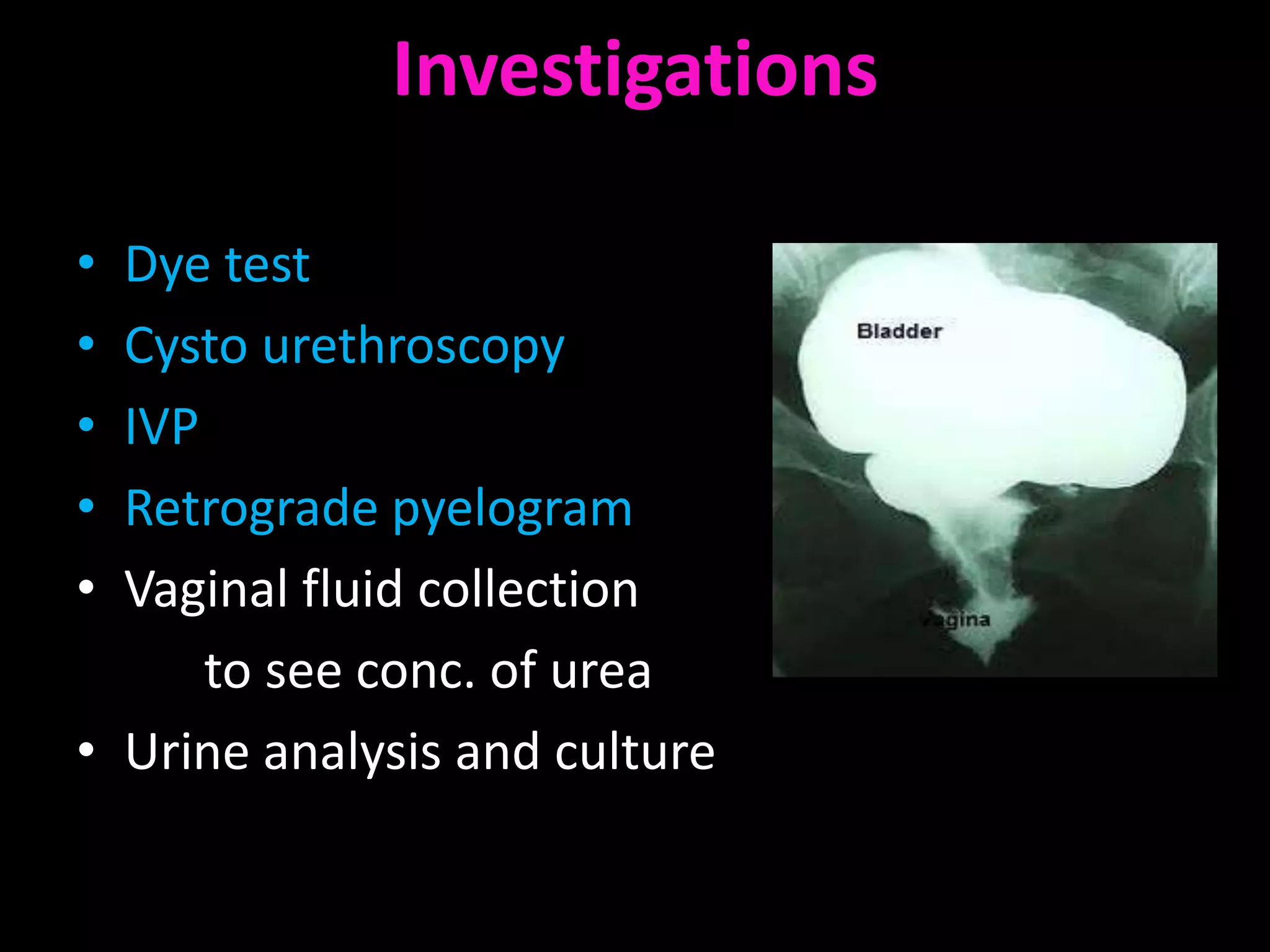
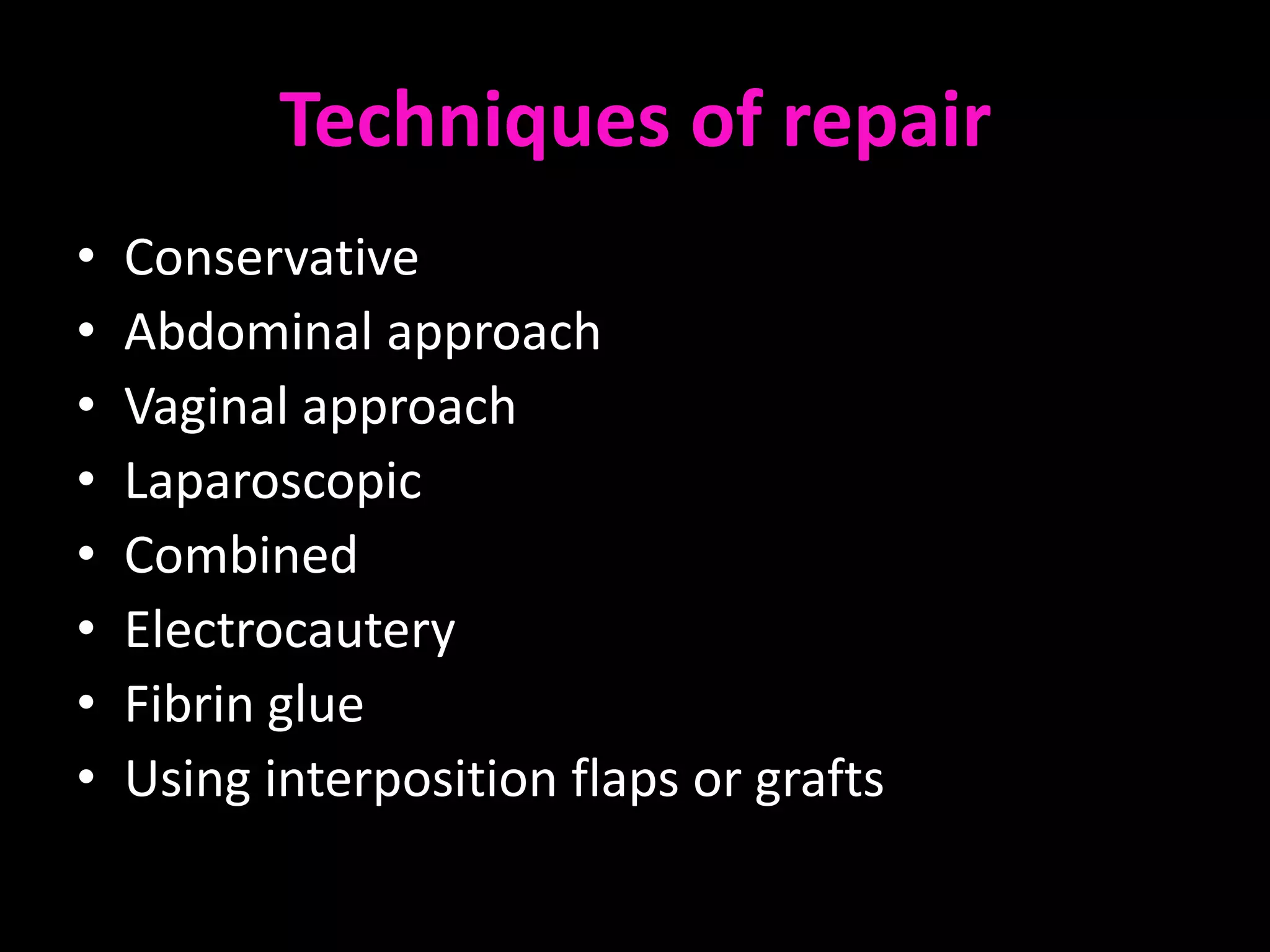
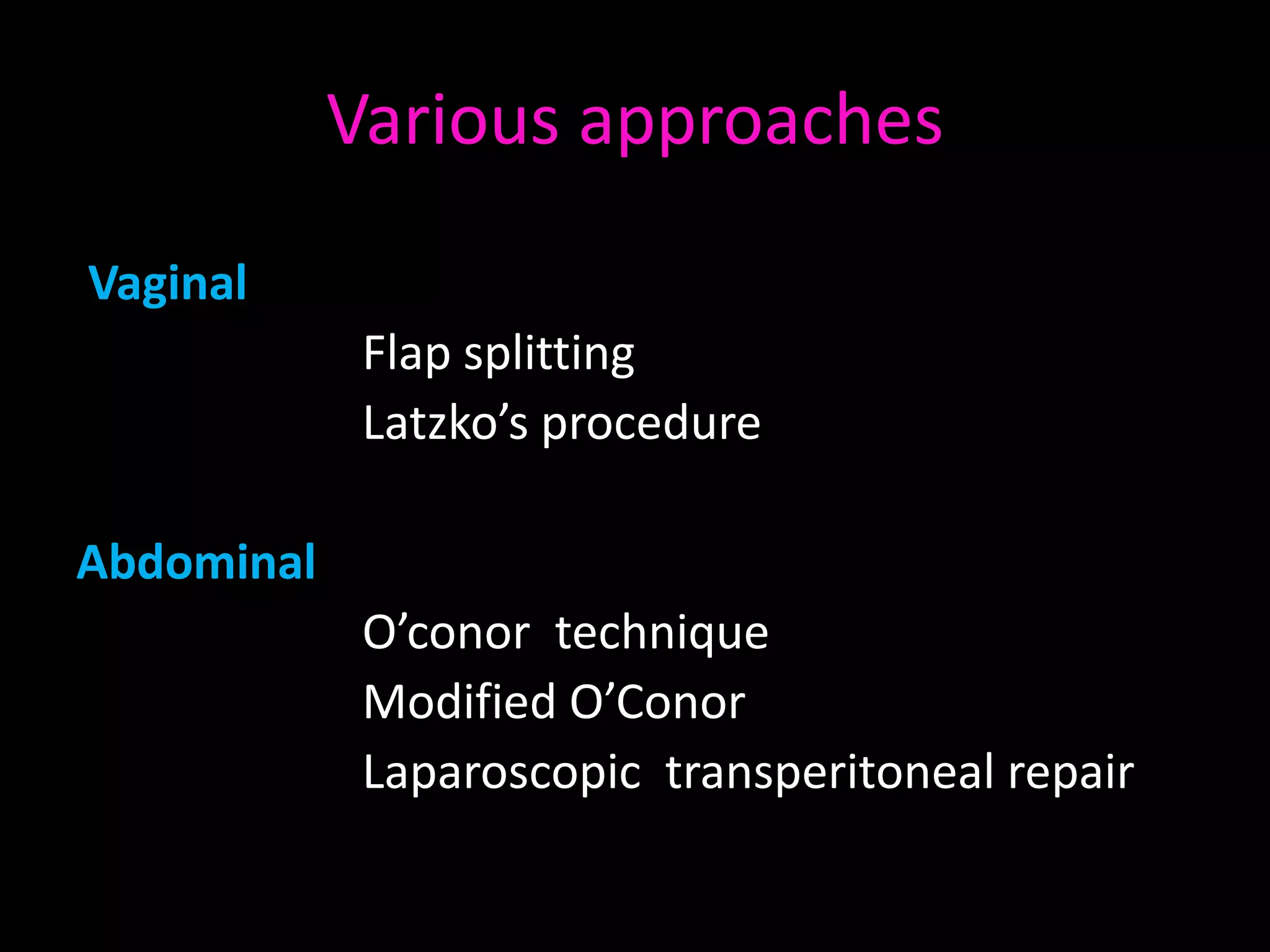
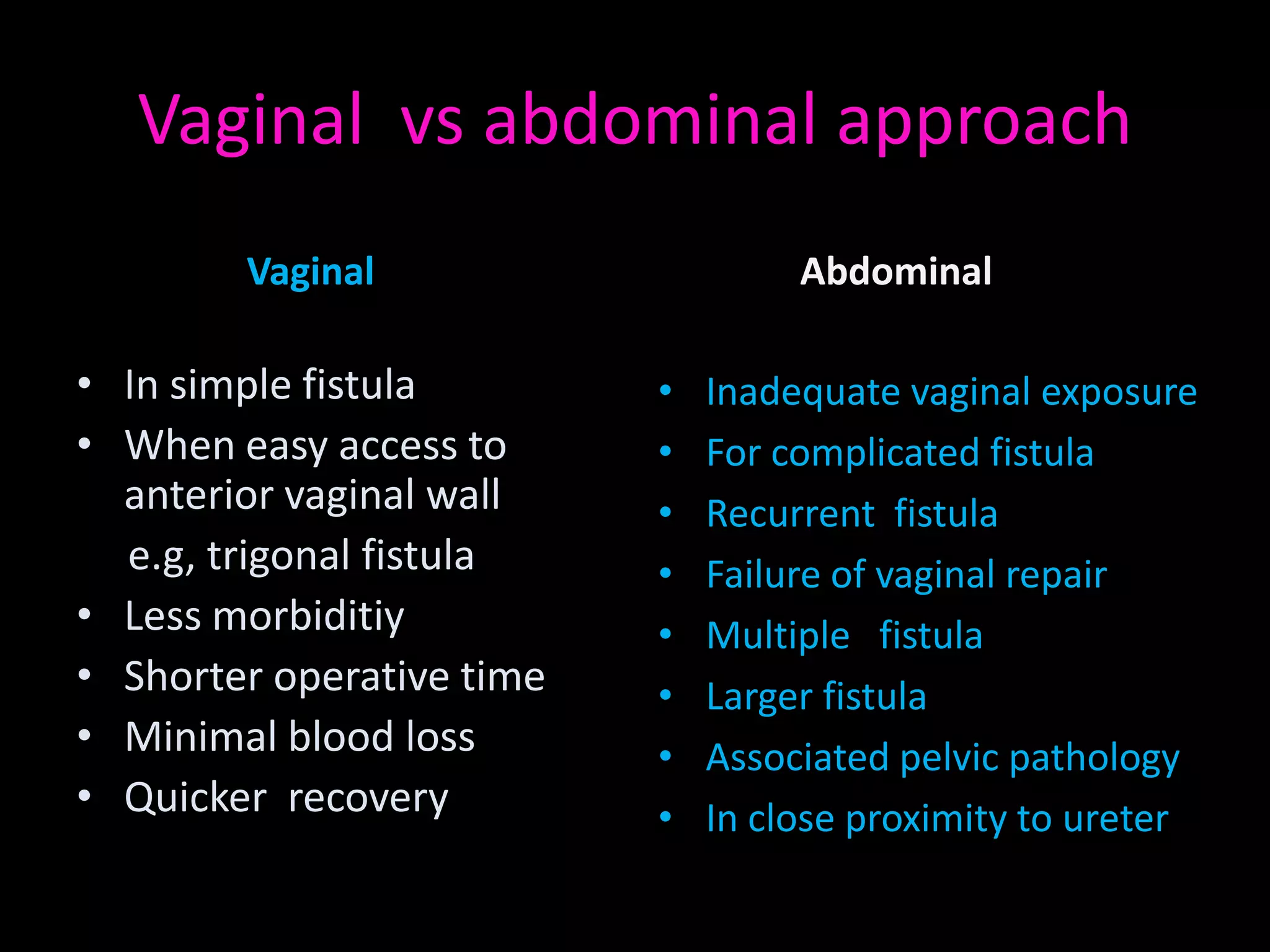
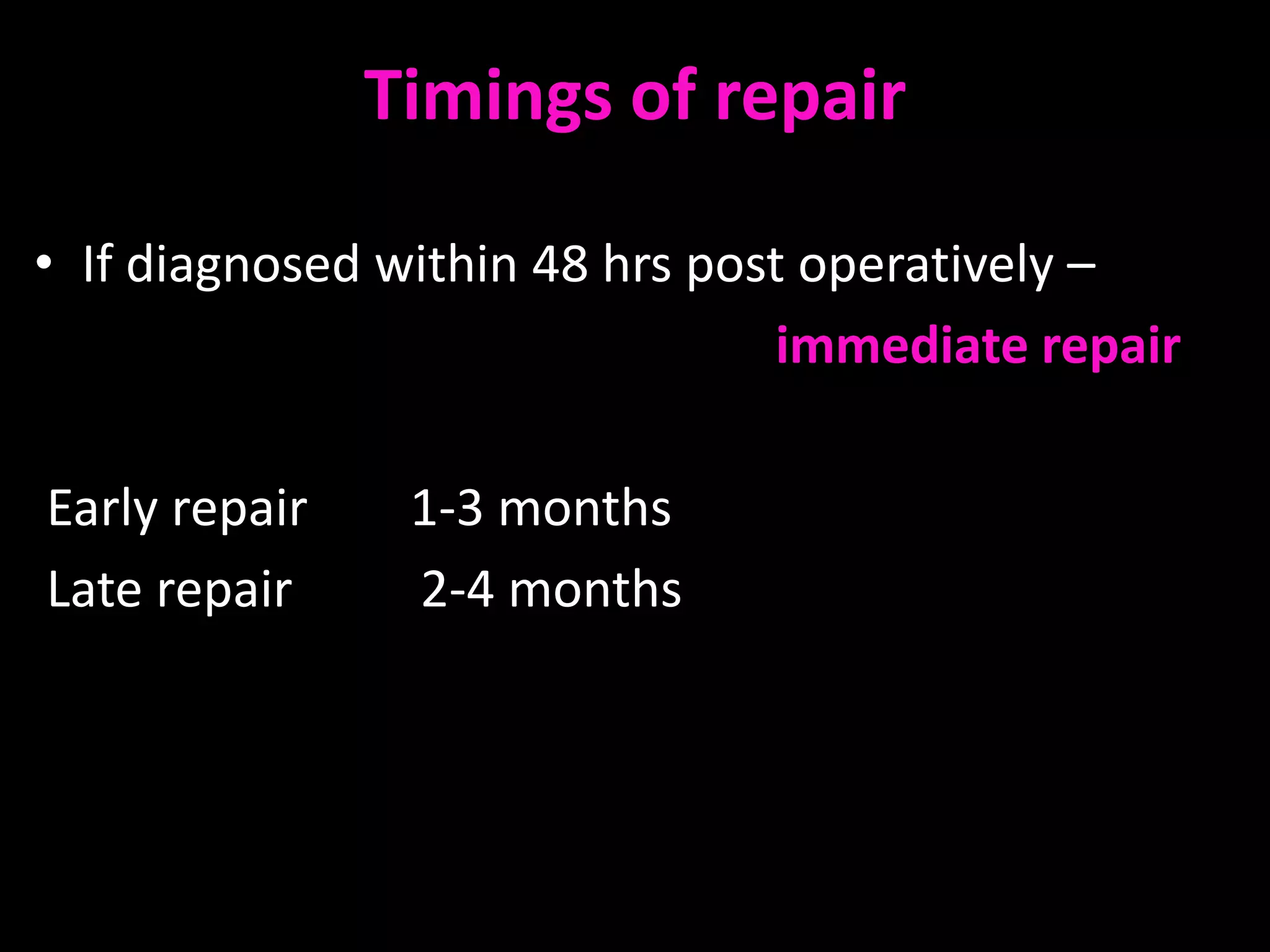
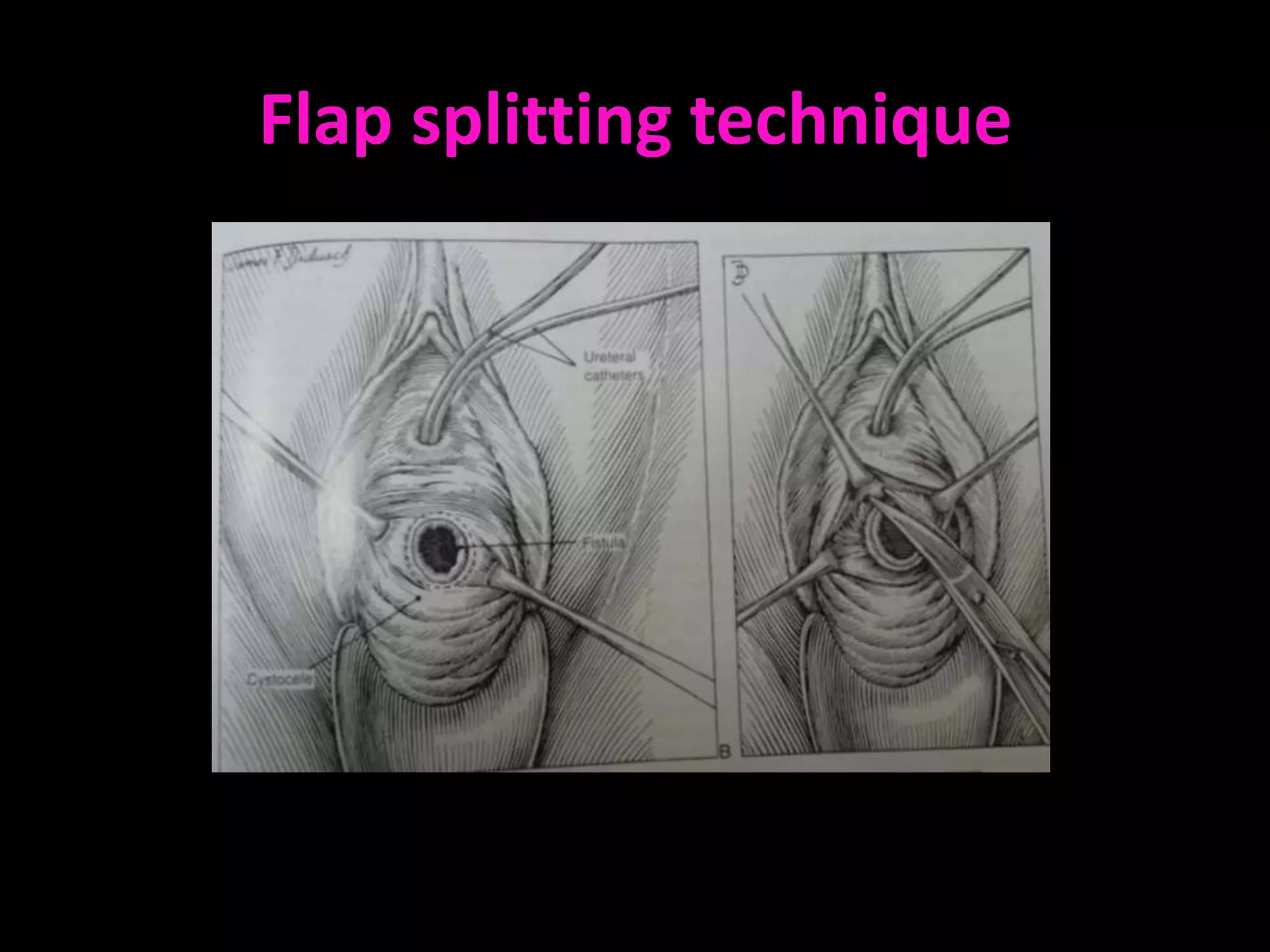
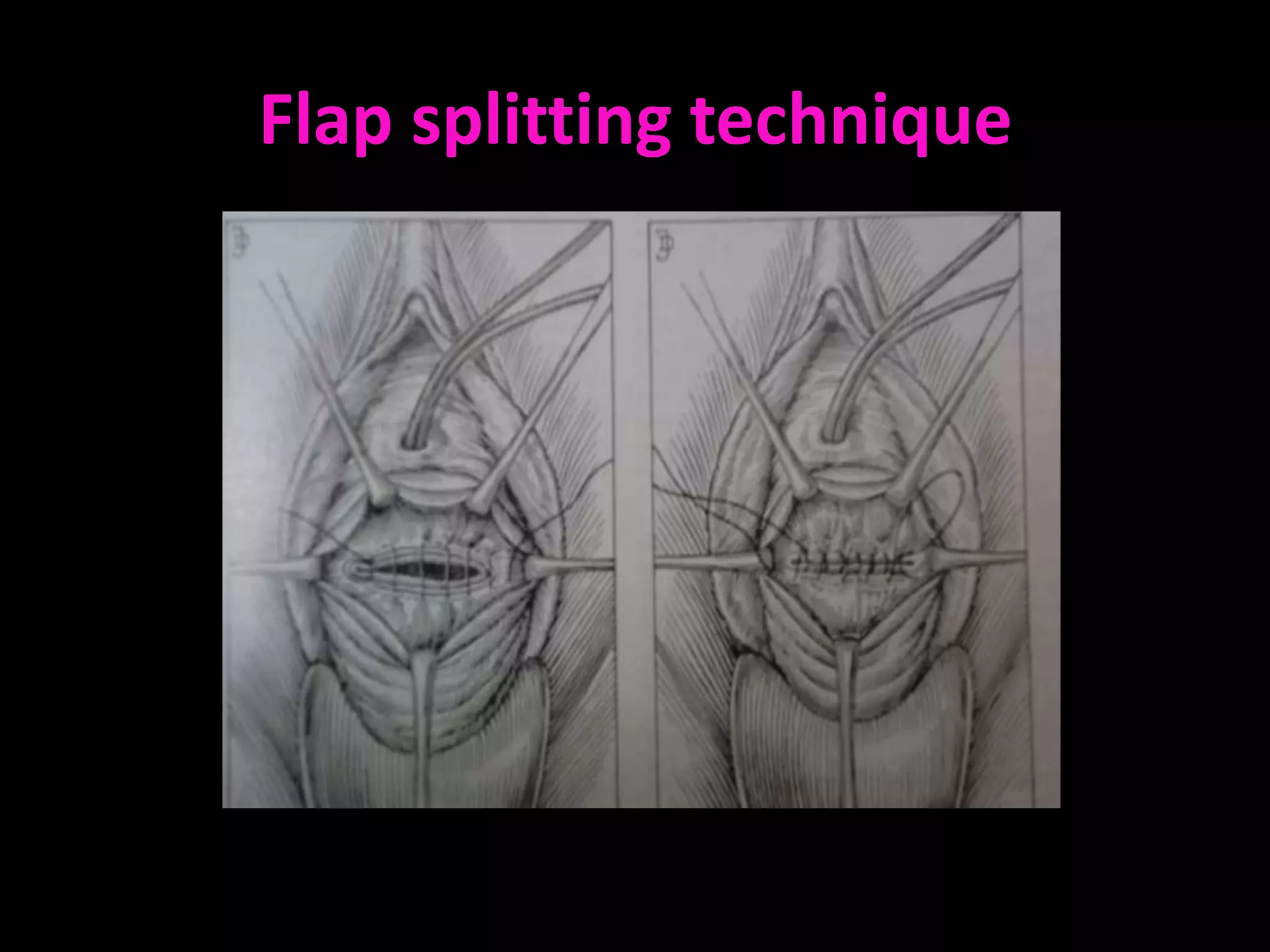
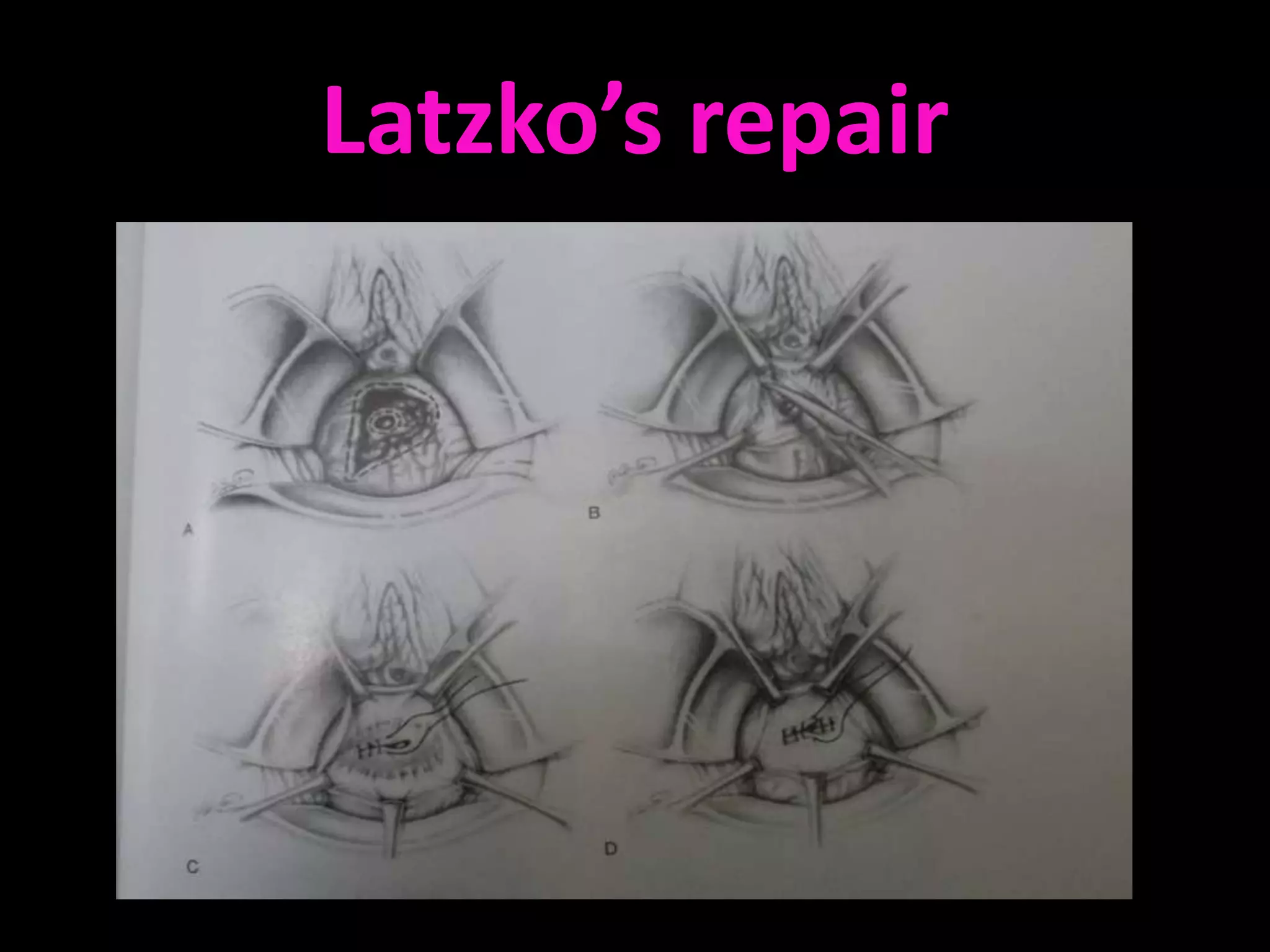
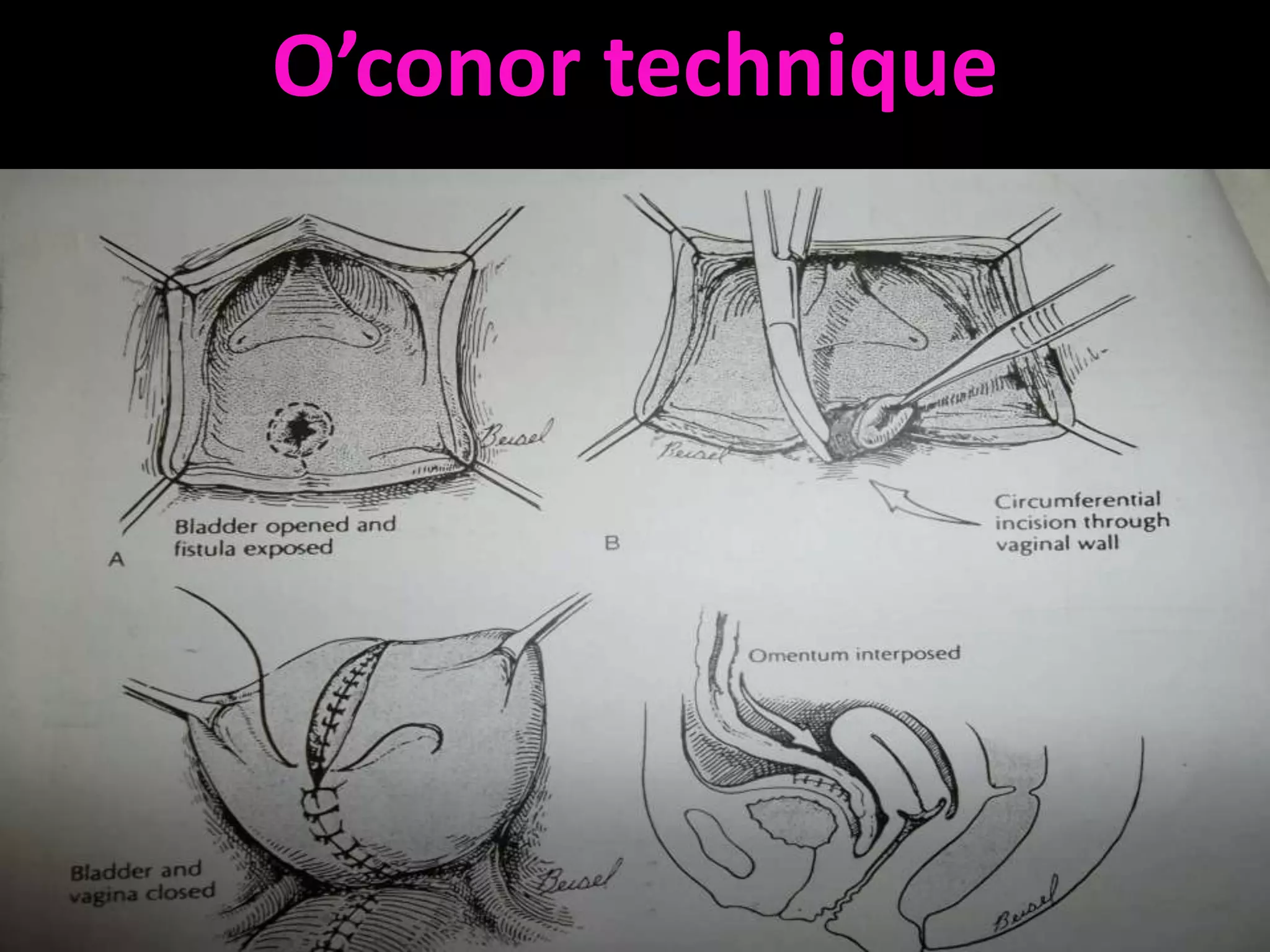
The document provides information about the anatomy, blood supply, innervation and functions of the urinary bladder. It discusses the location of the bladder in the pelvis. It describes the parts of the bladder including the body, fundus, neck, apex and surfaces. It explains micturition and various factors involved in bladder filling and emptying. The document also discusses bladder injuries including risk factors, signs, management and repair techniques. It provides details about vesicovaginal fistula including causes, types, presentations and approaches to repair.