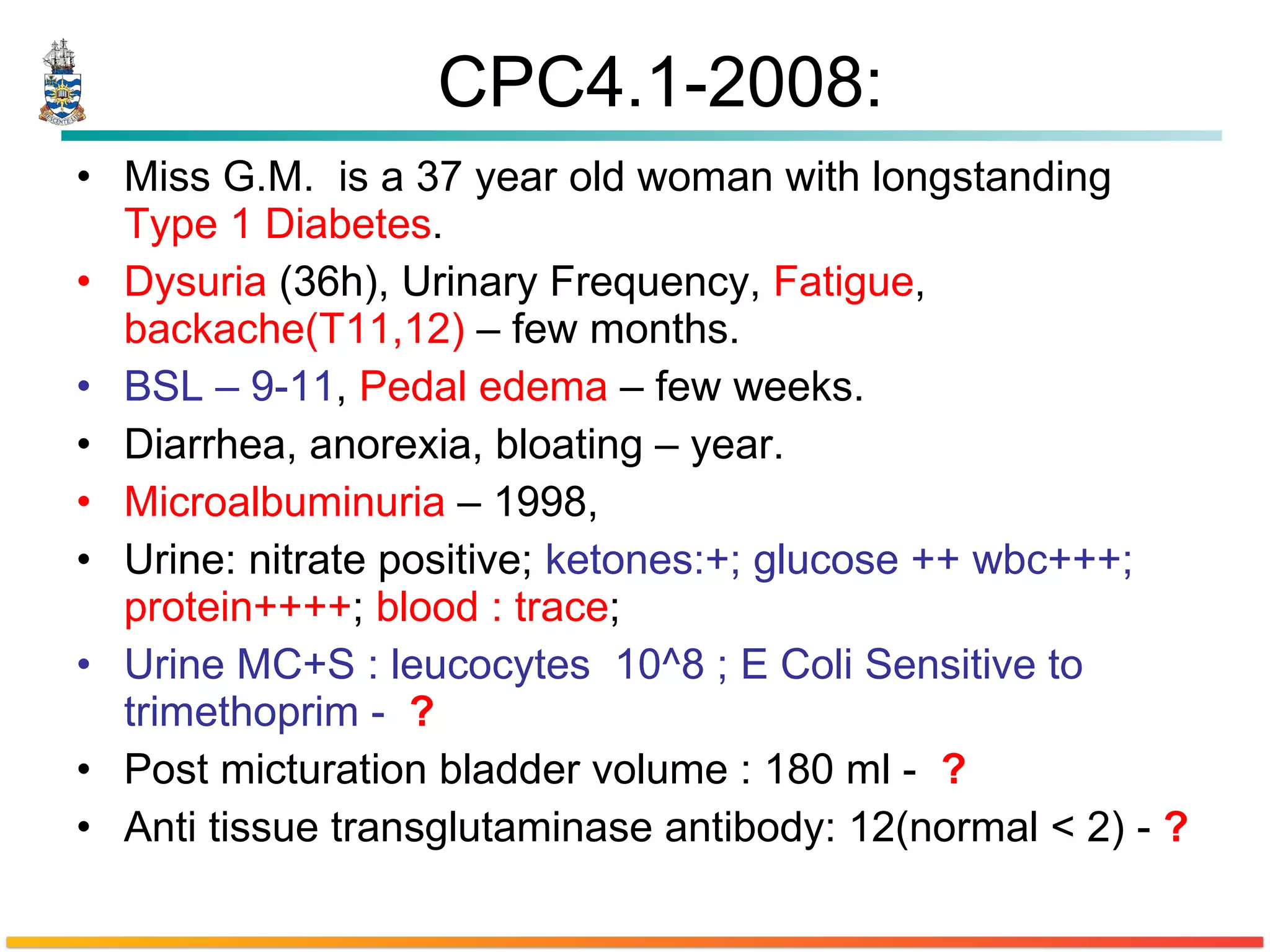
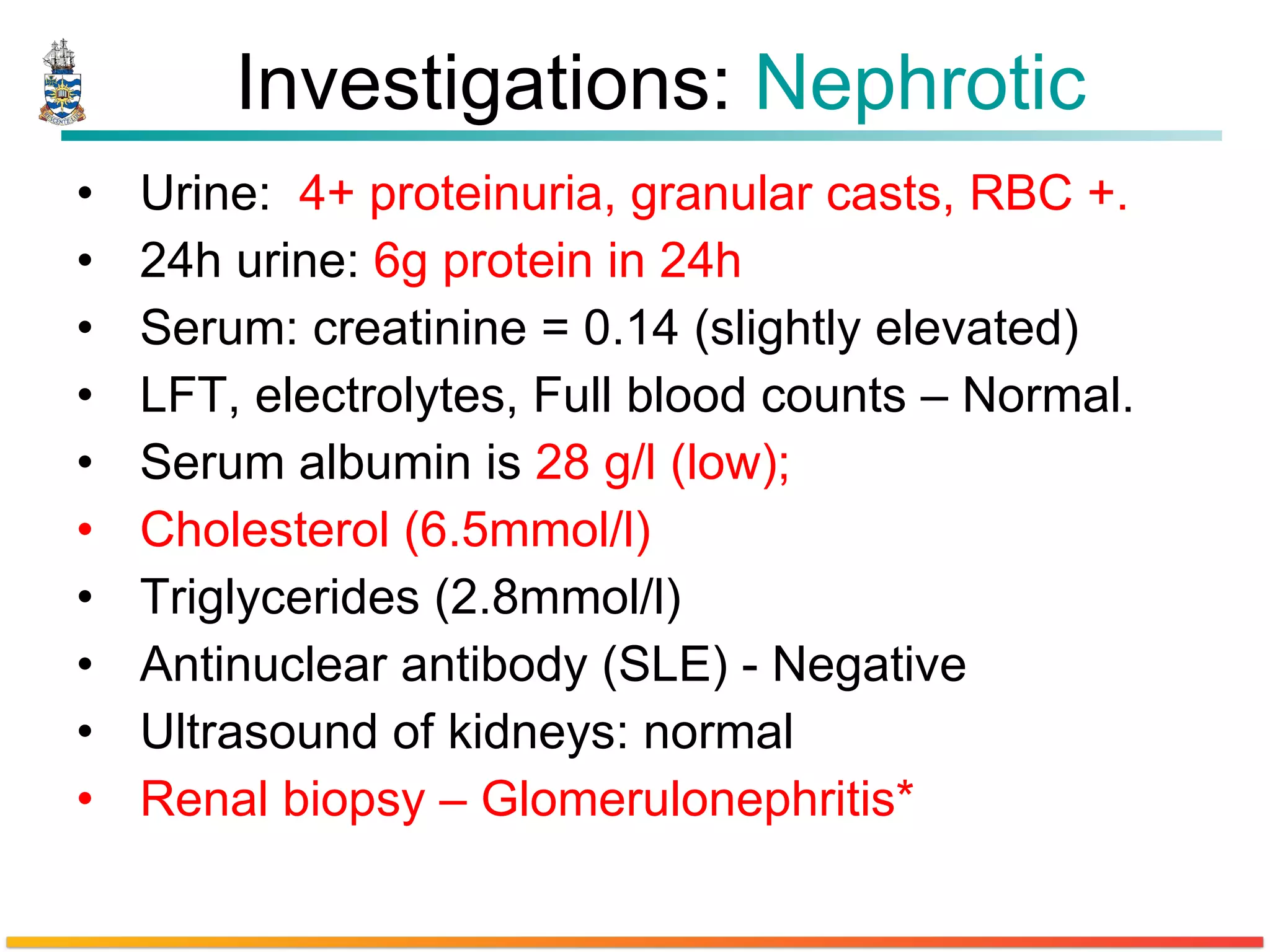
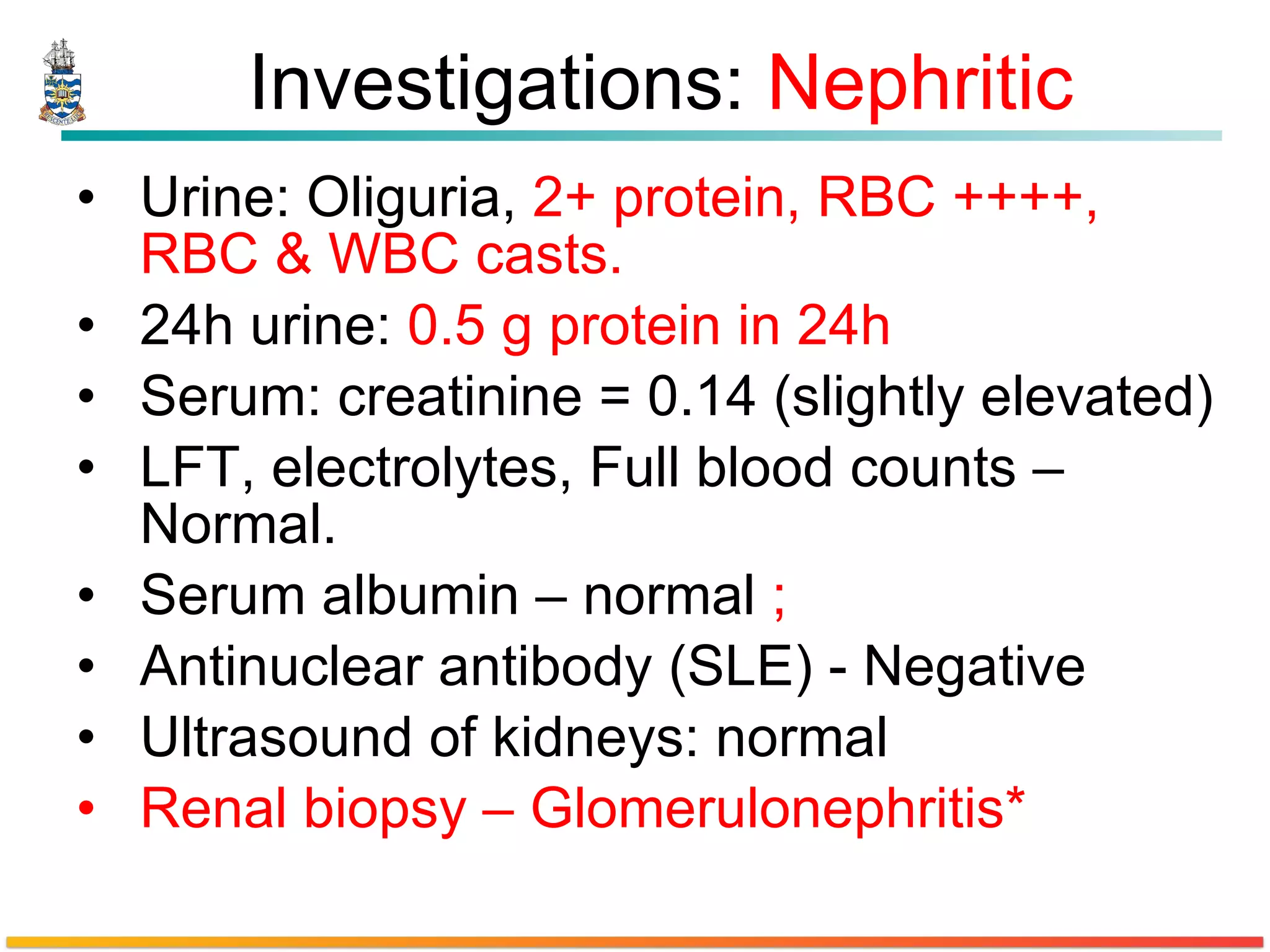
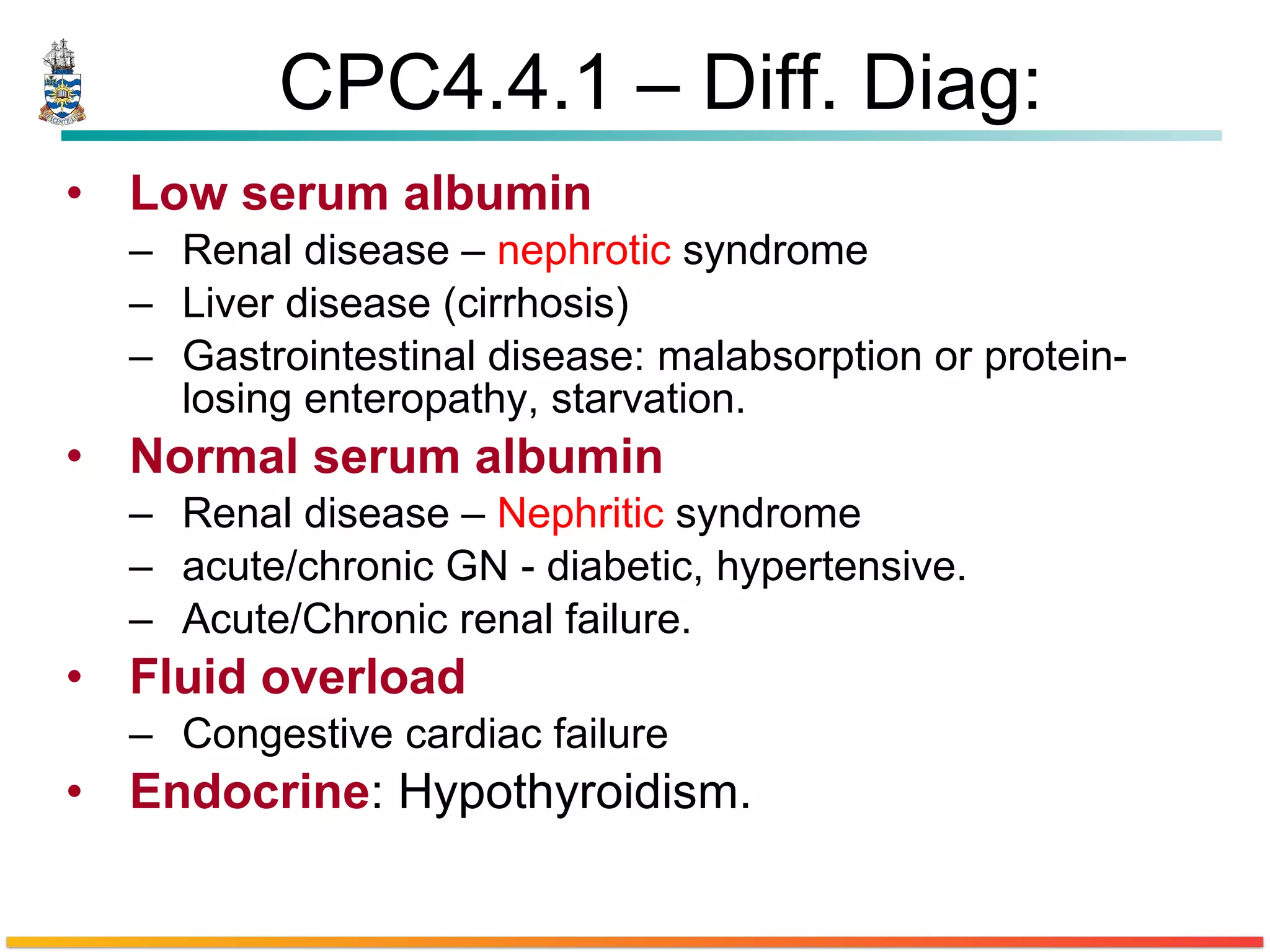
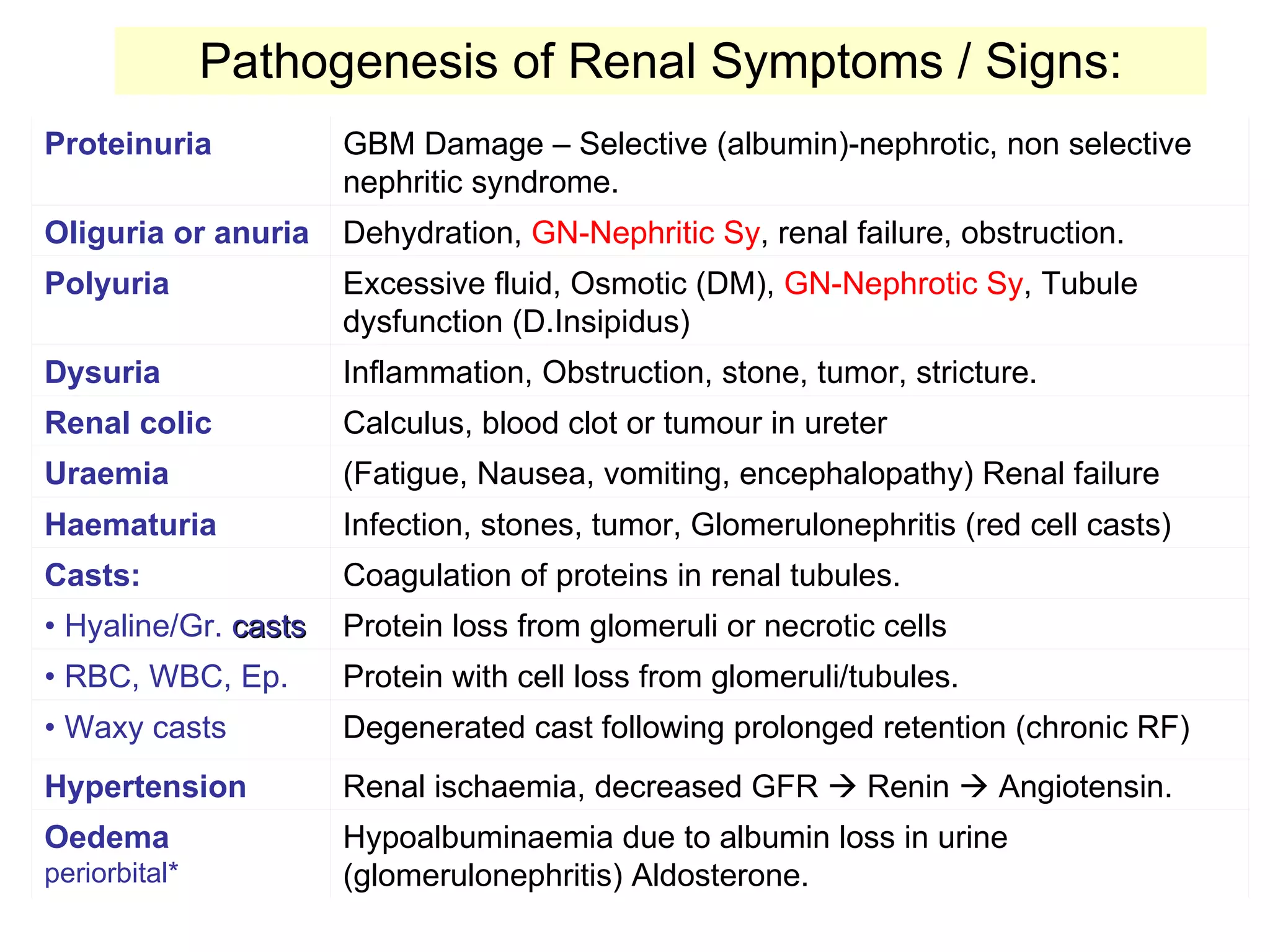
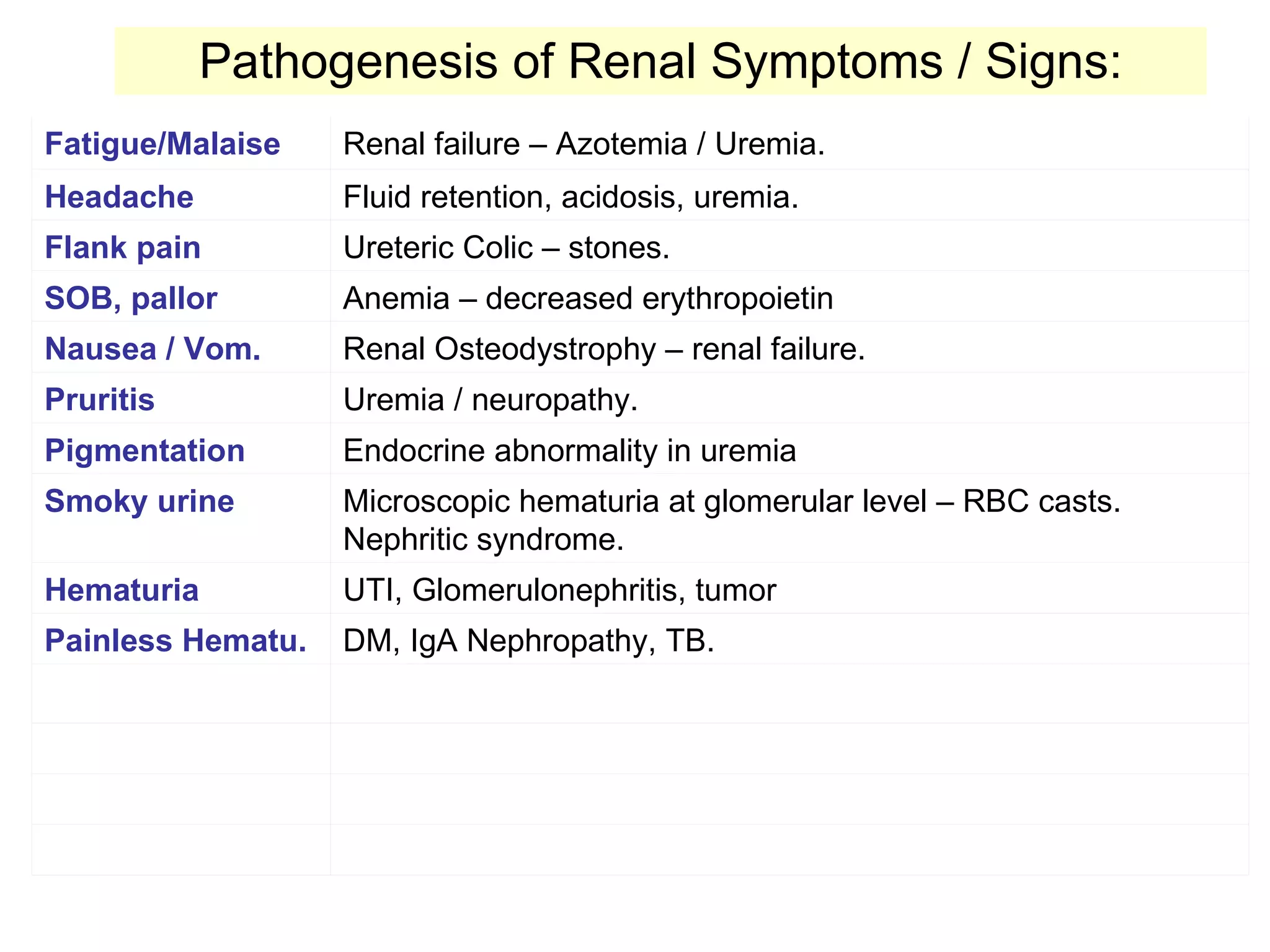
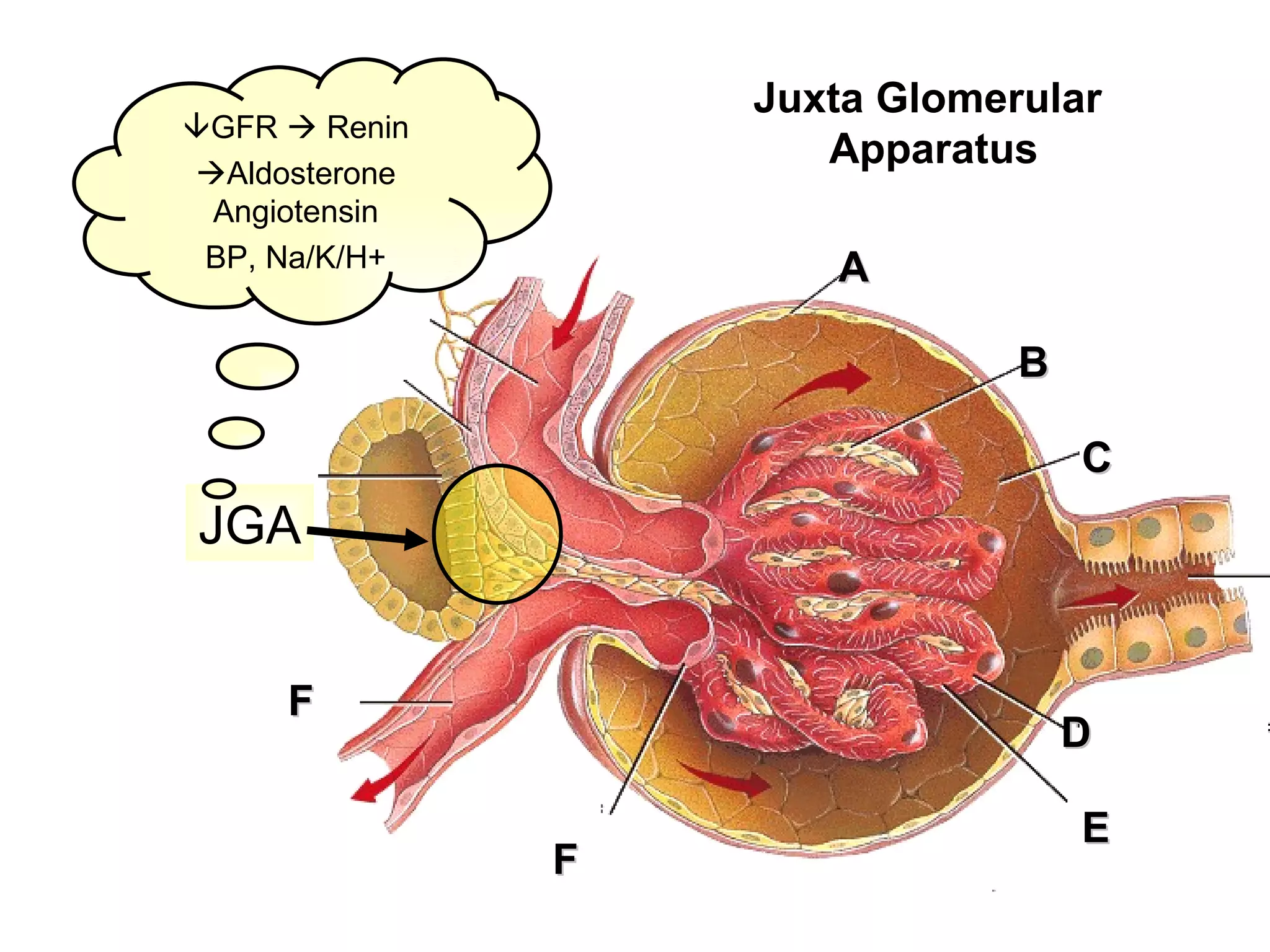
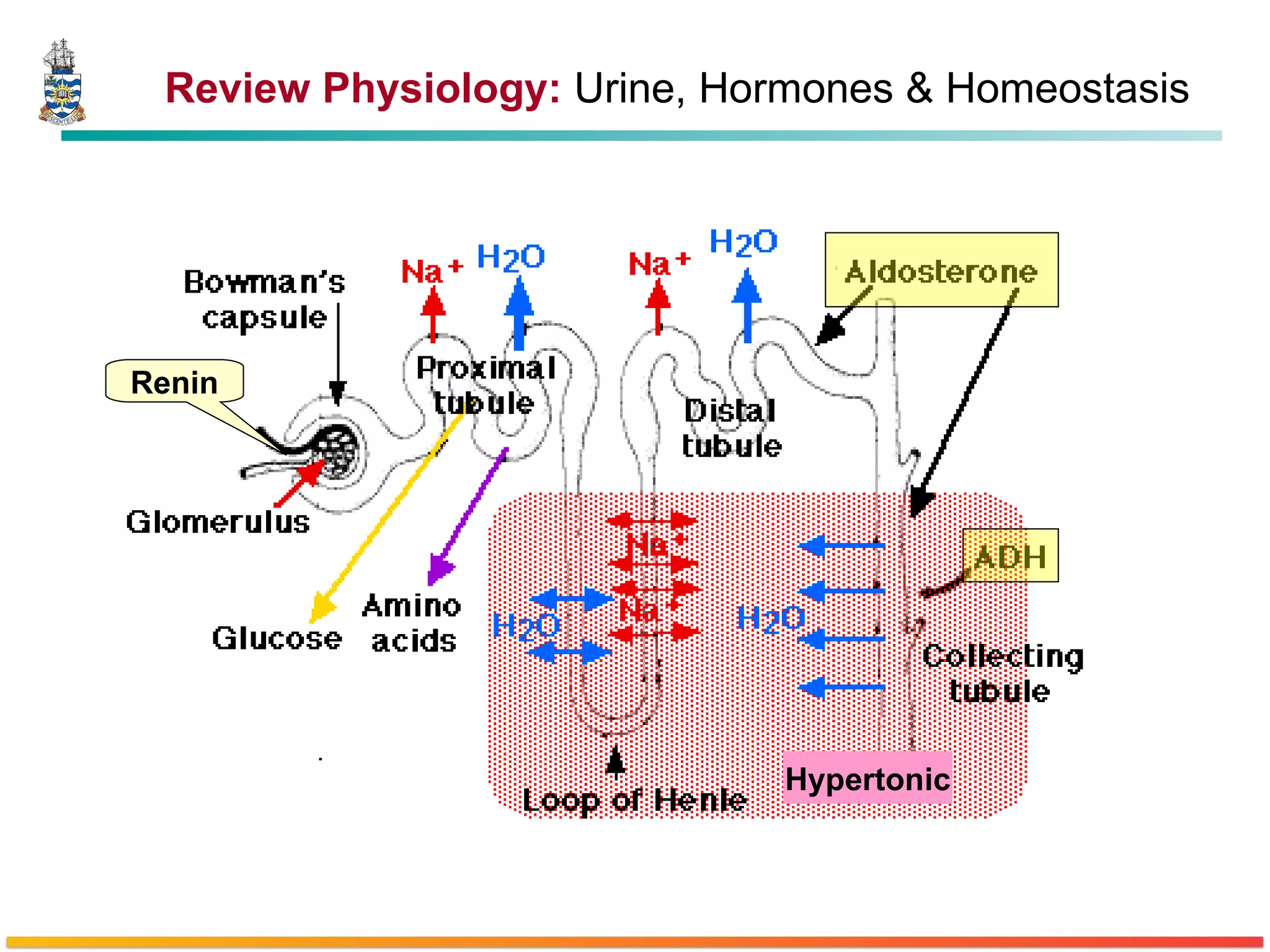
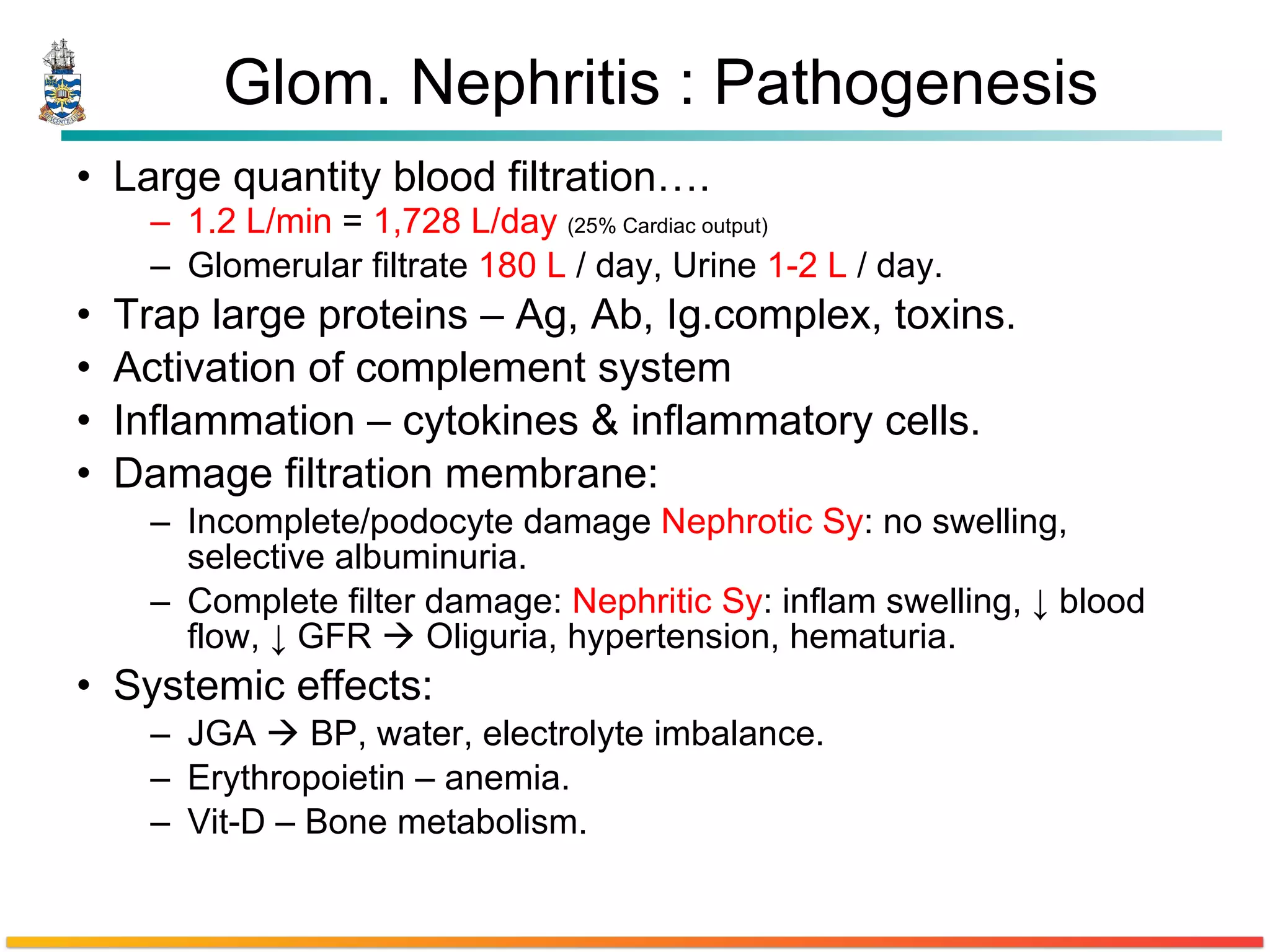
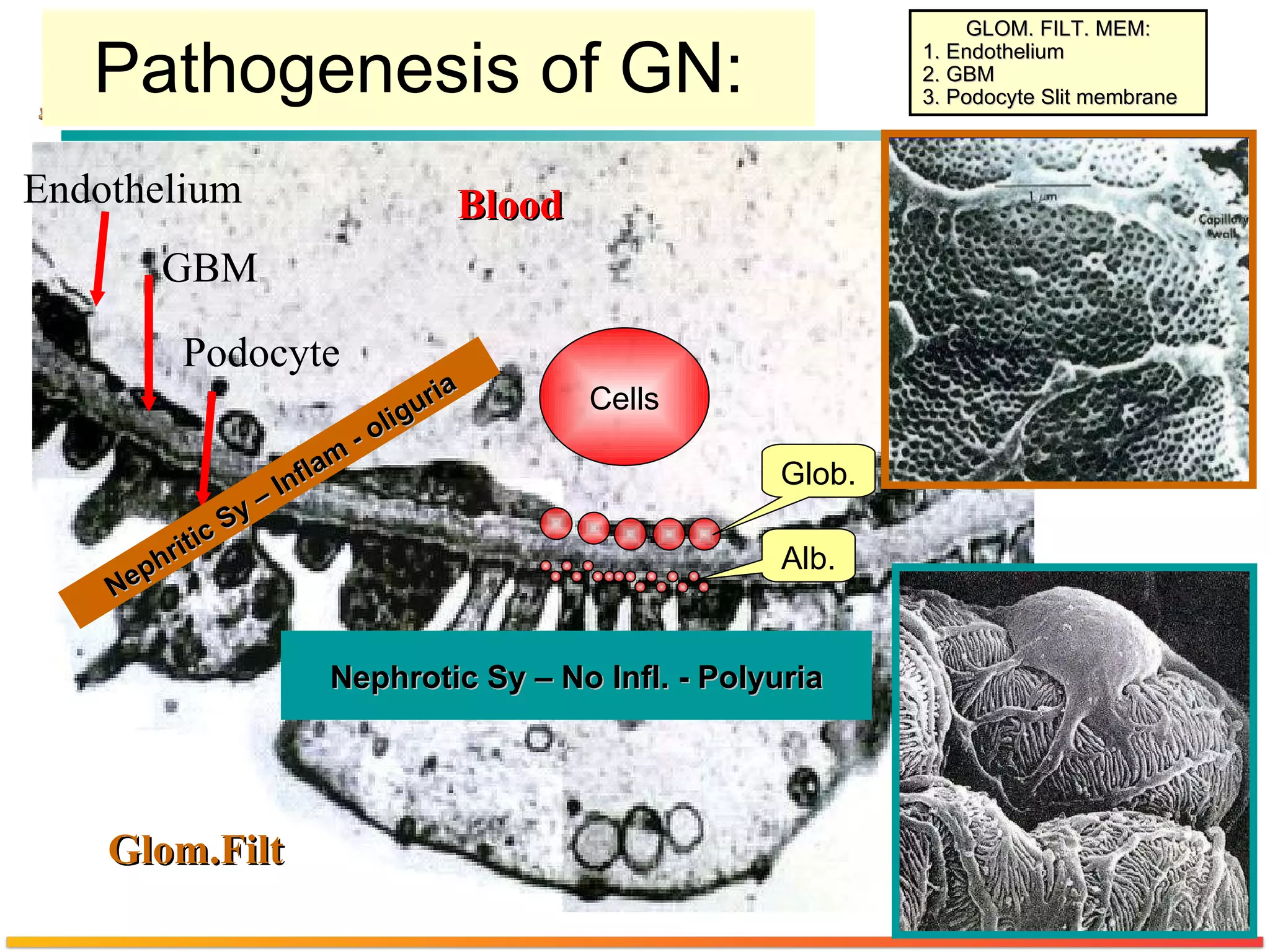
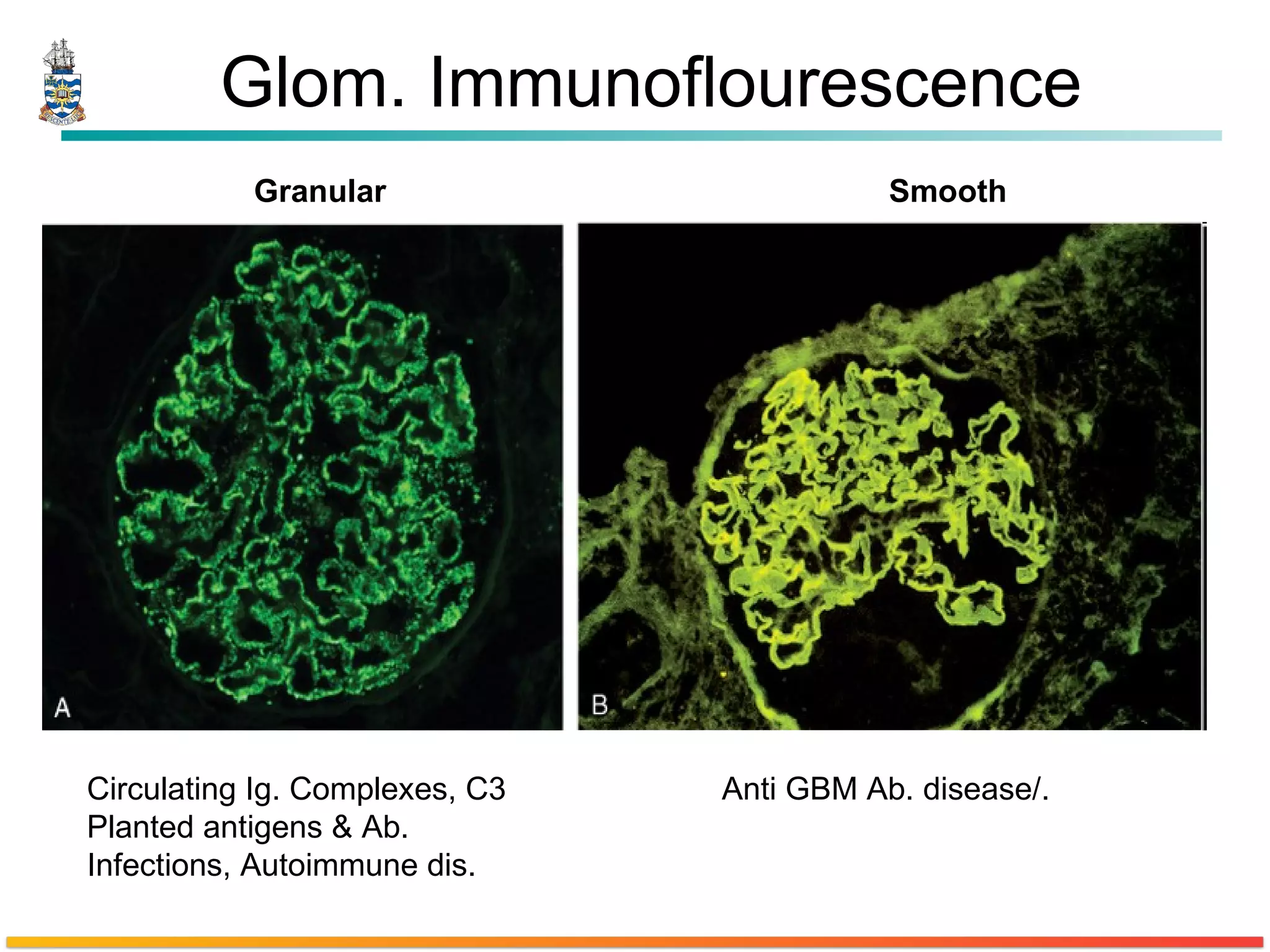
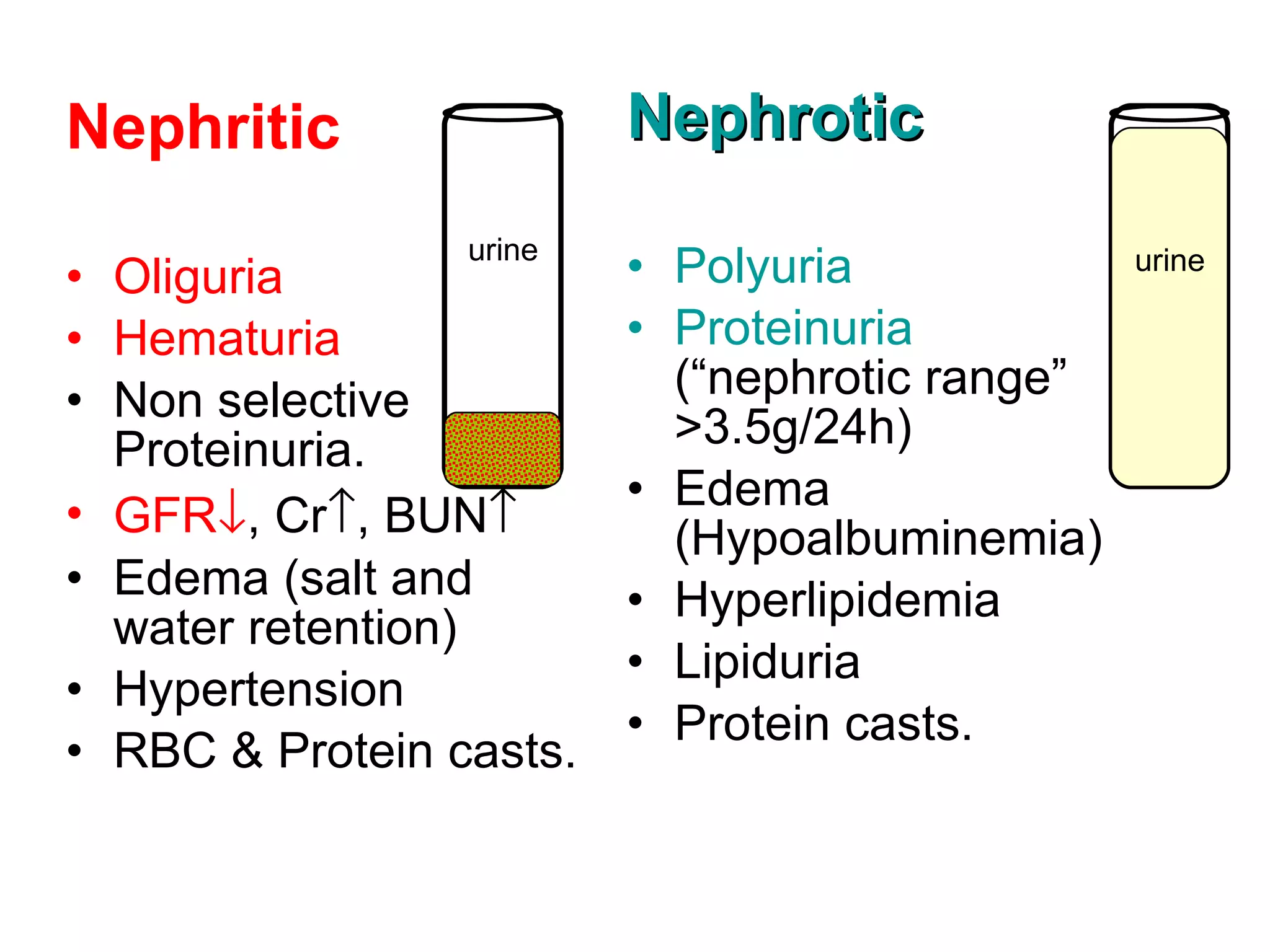
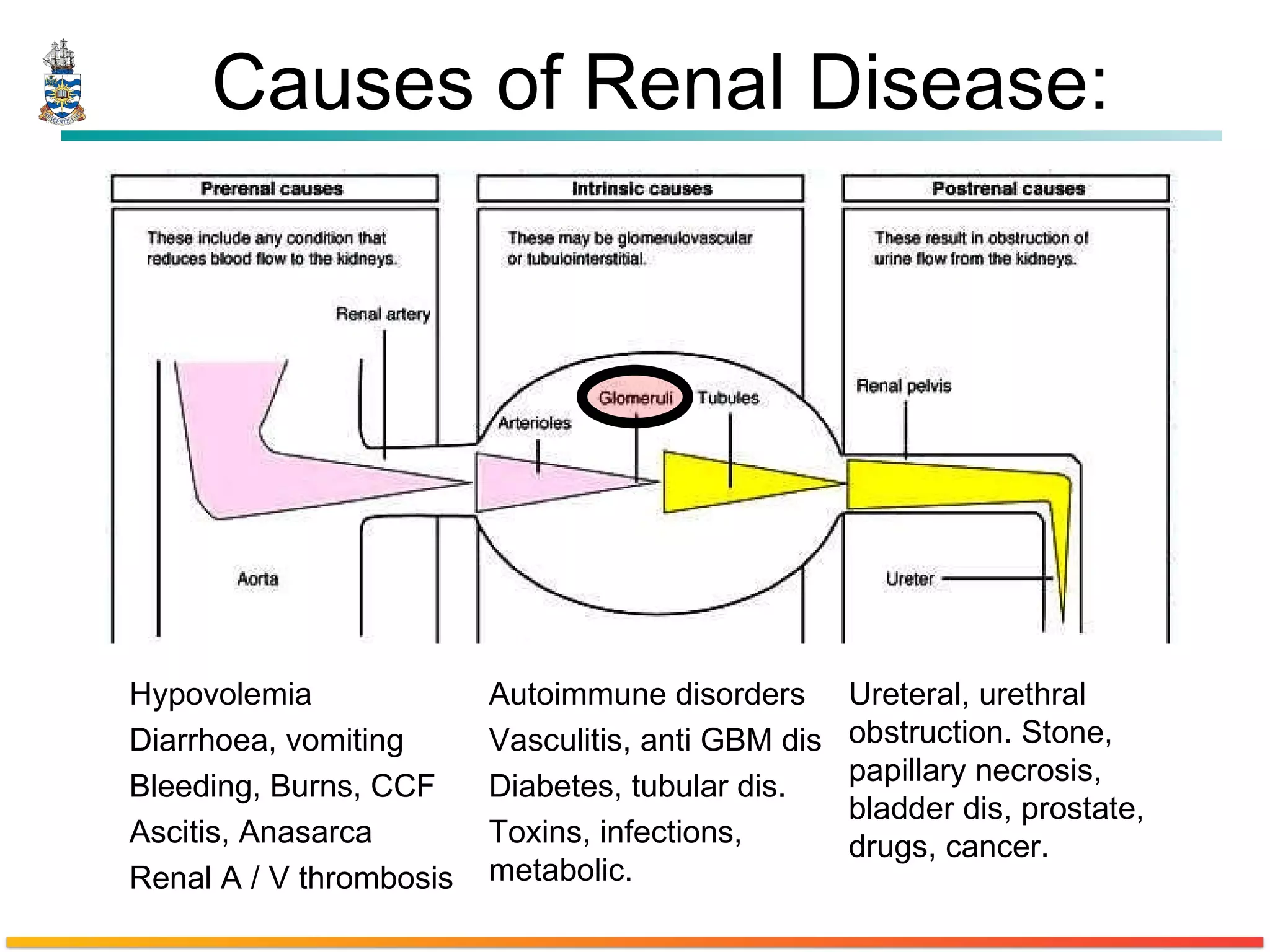
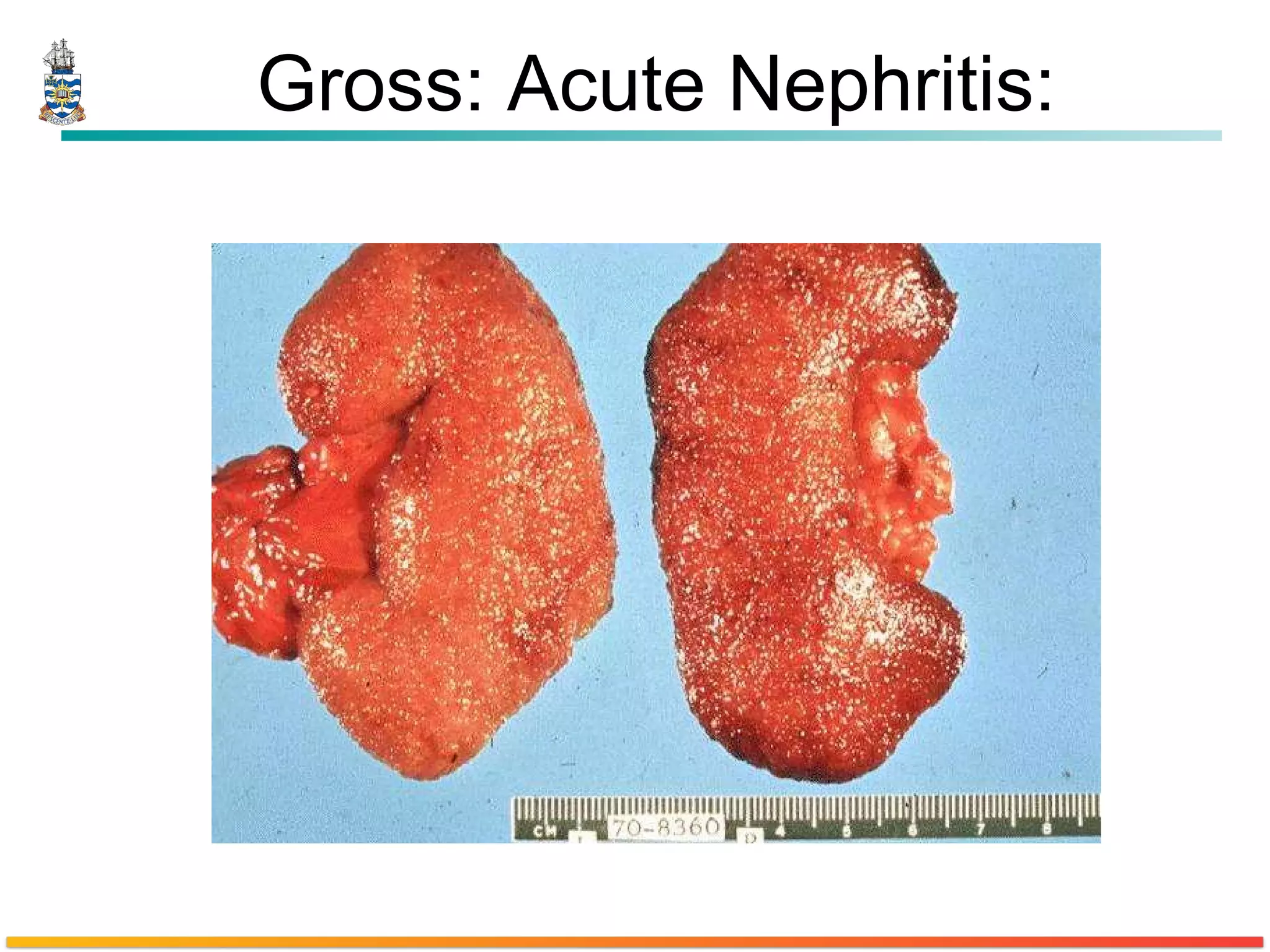
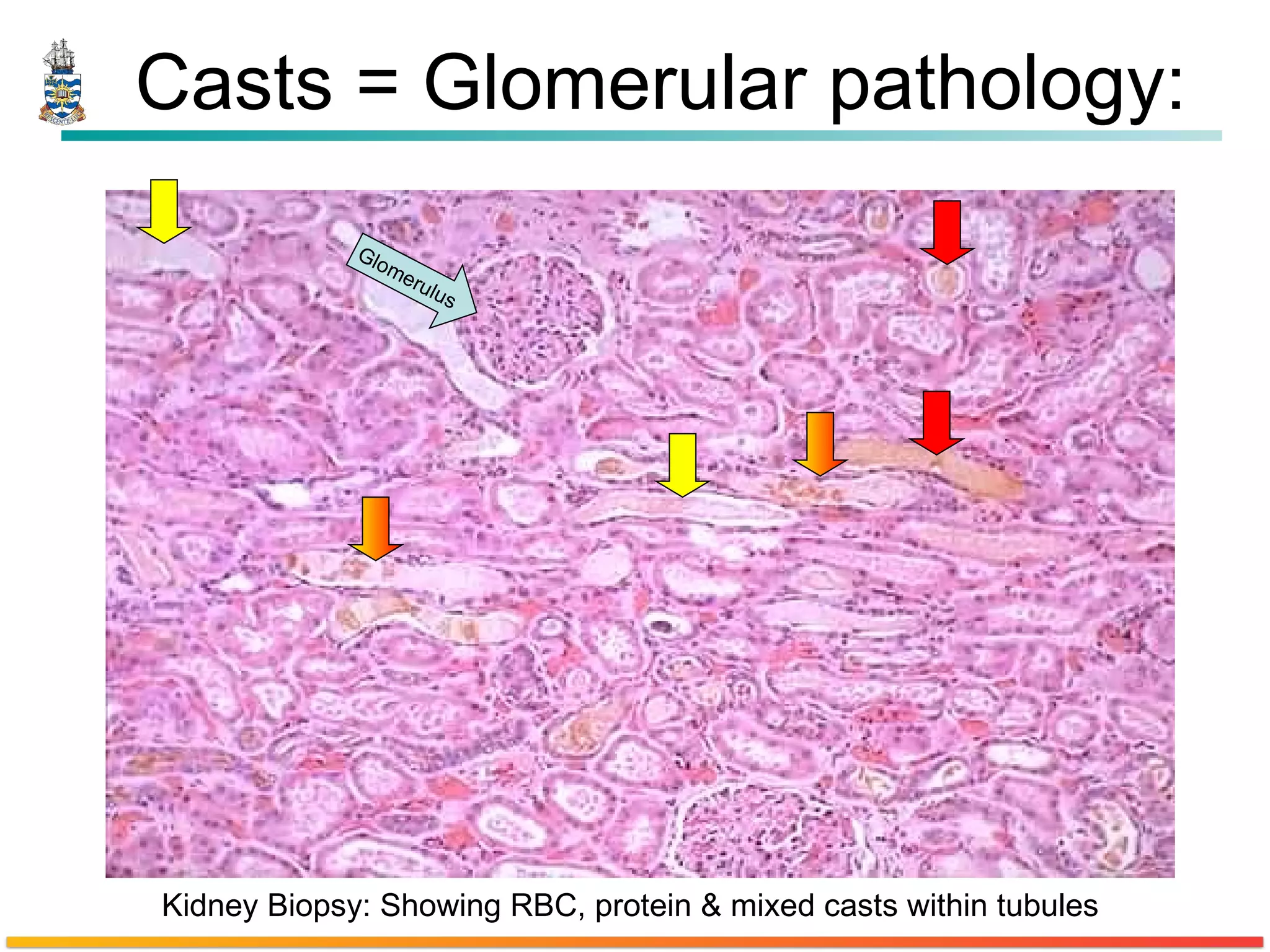
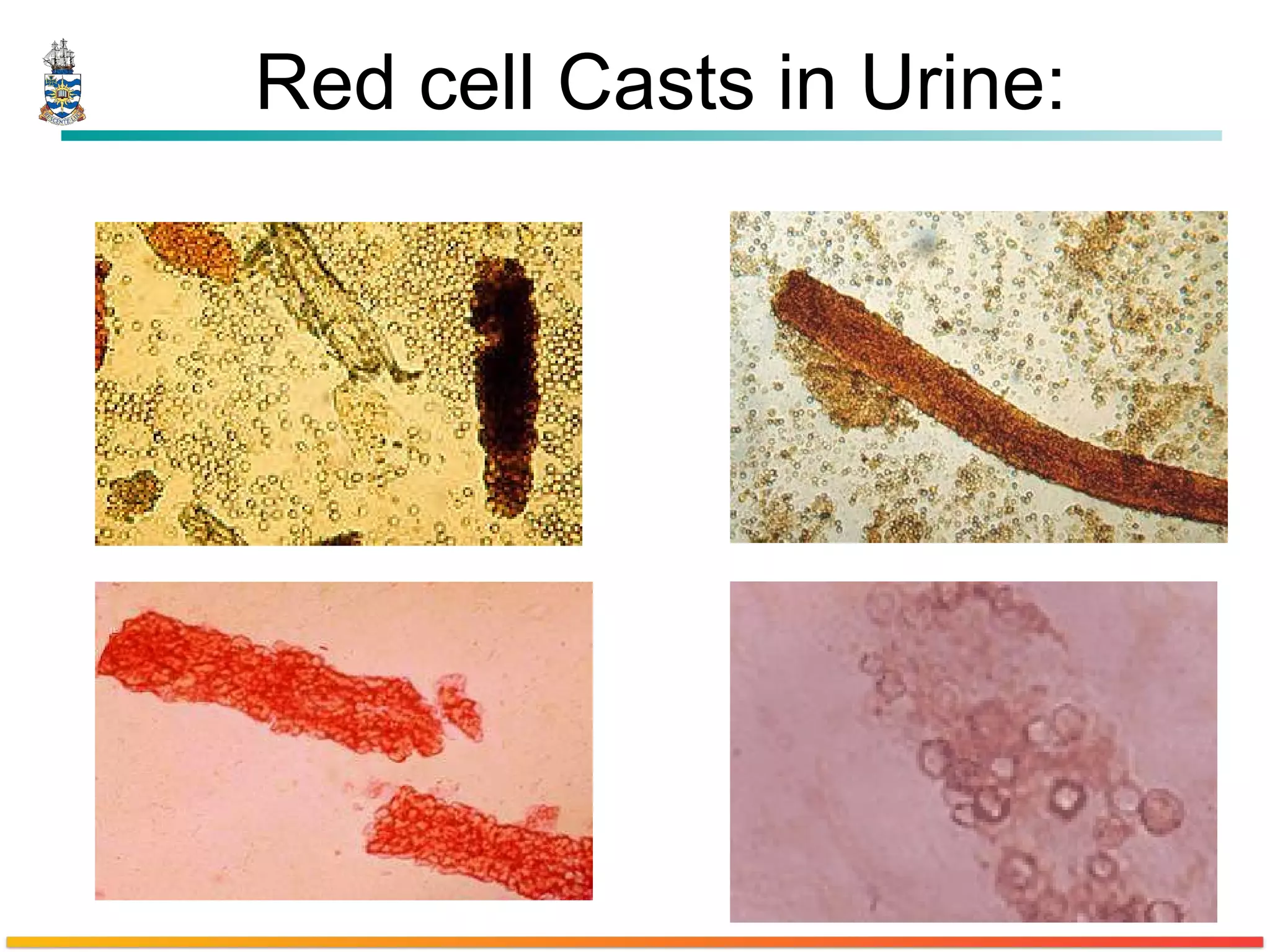
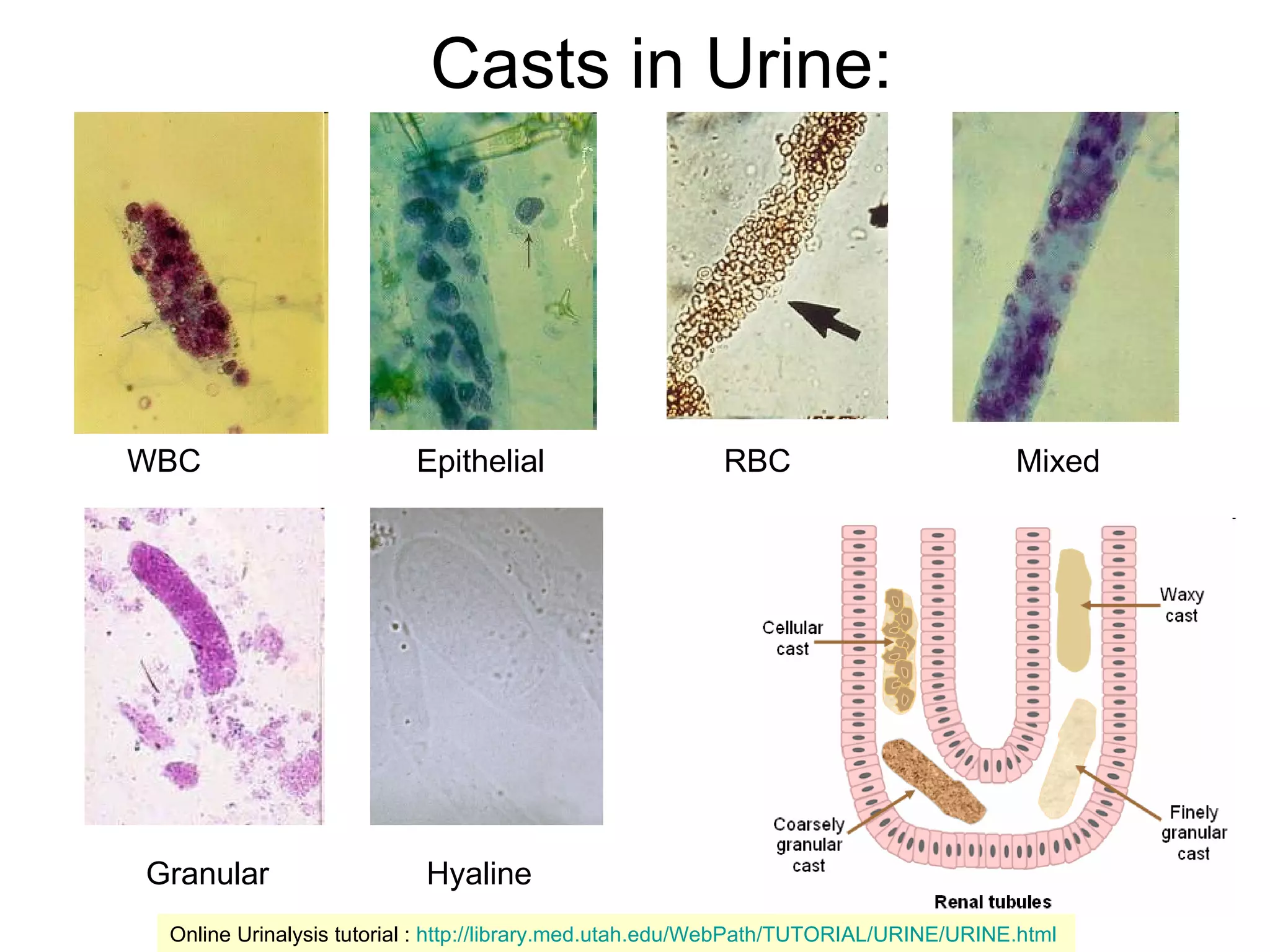
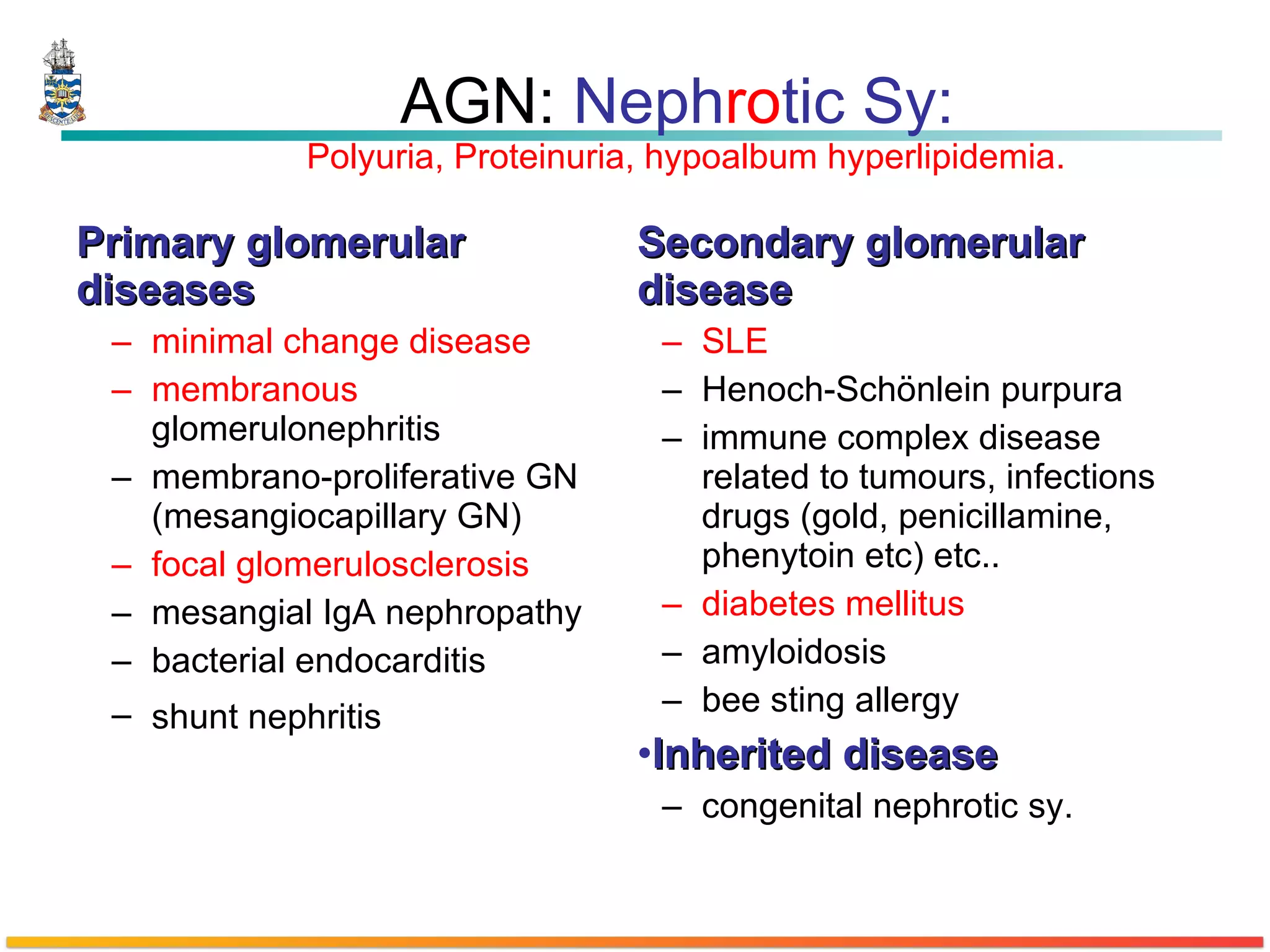
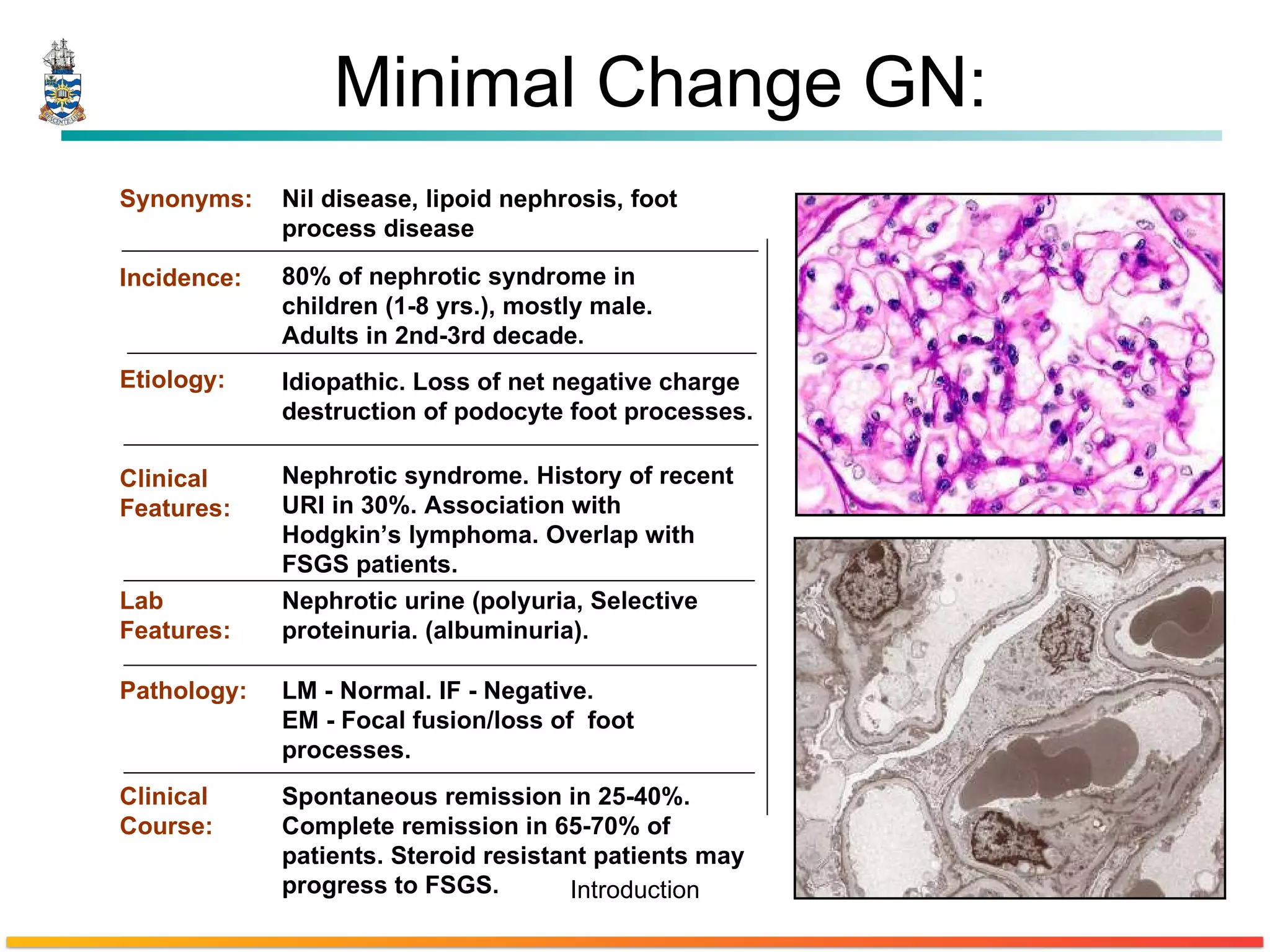
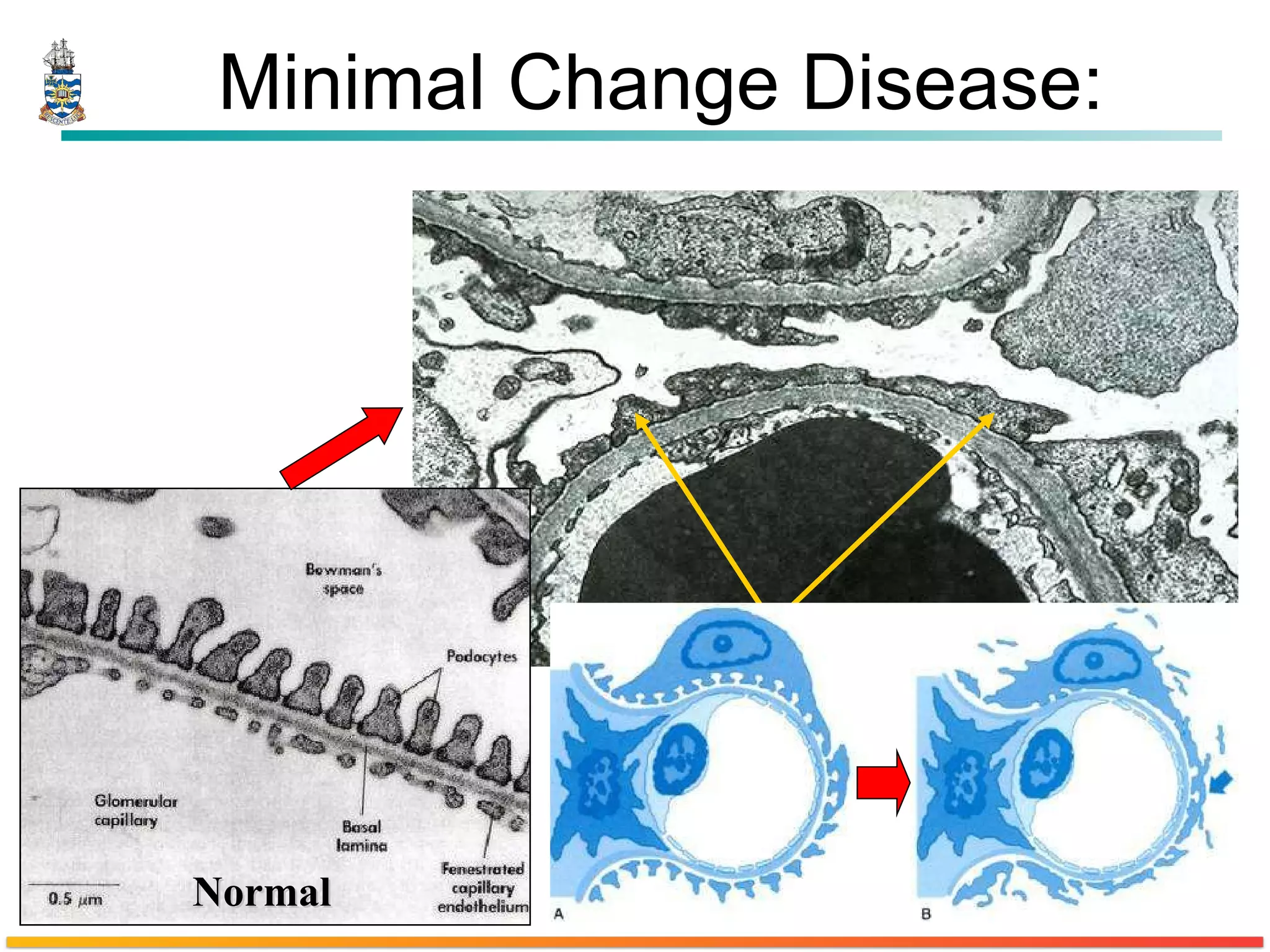
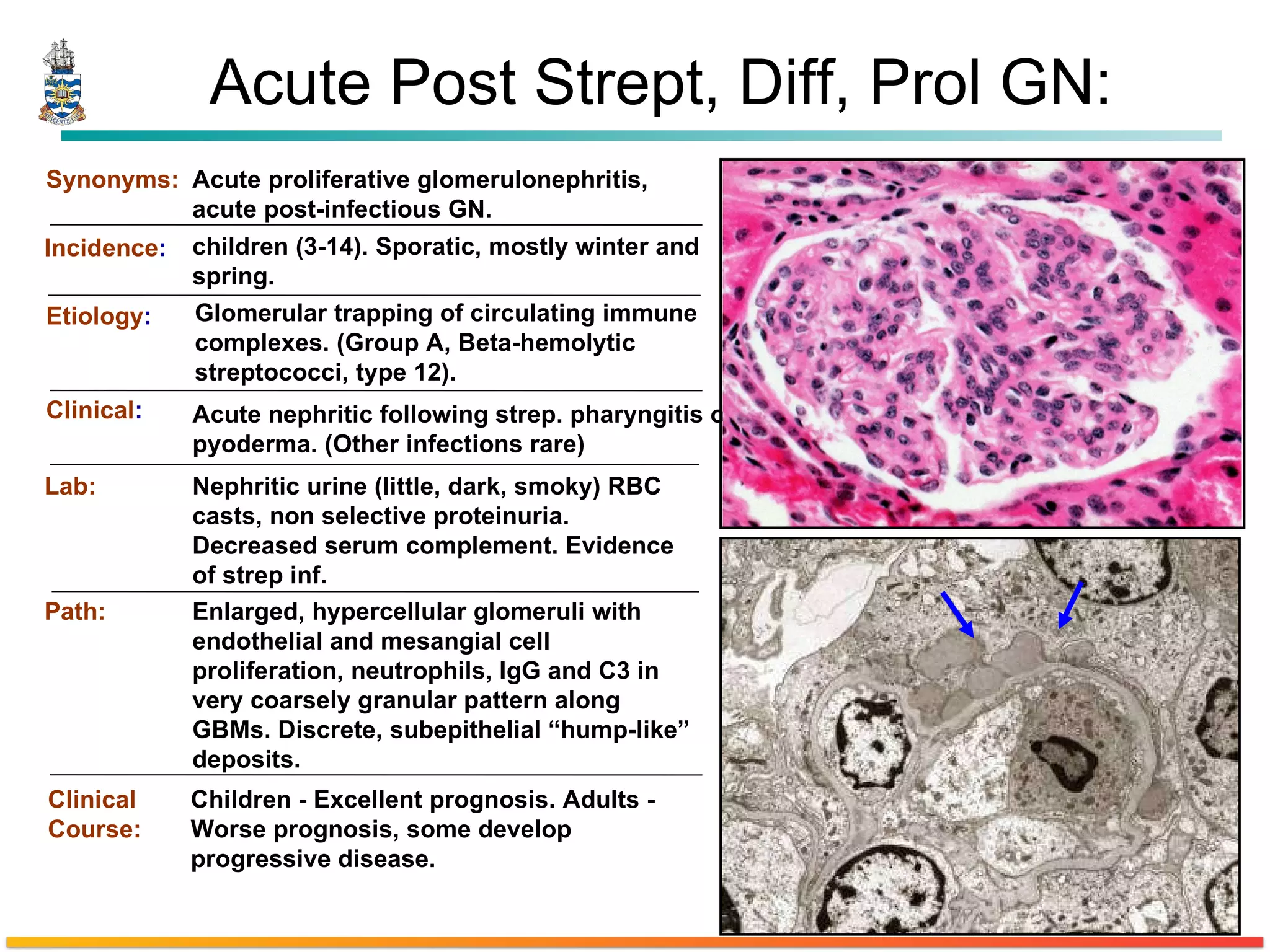
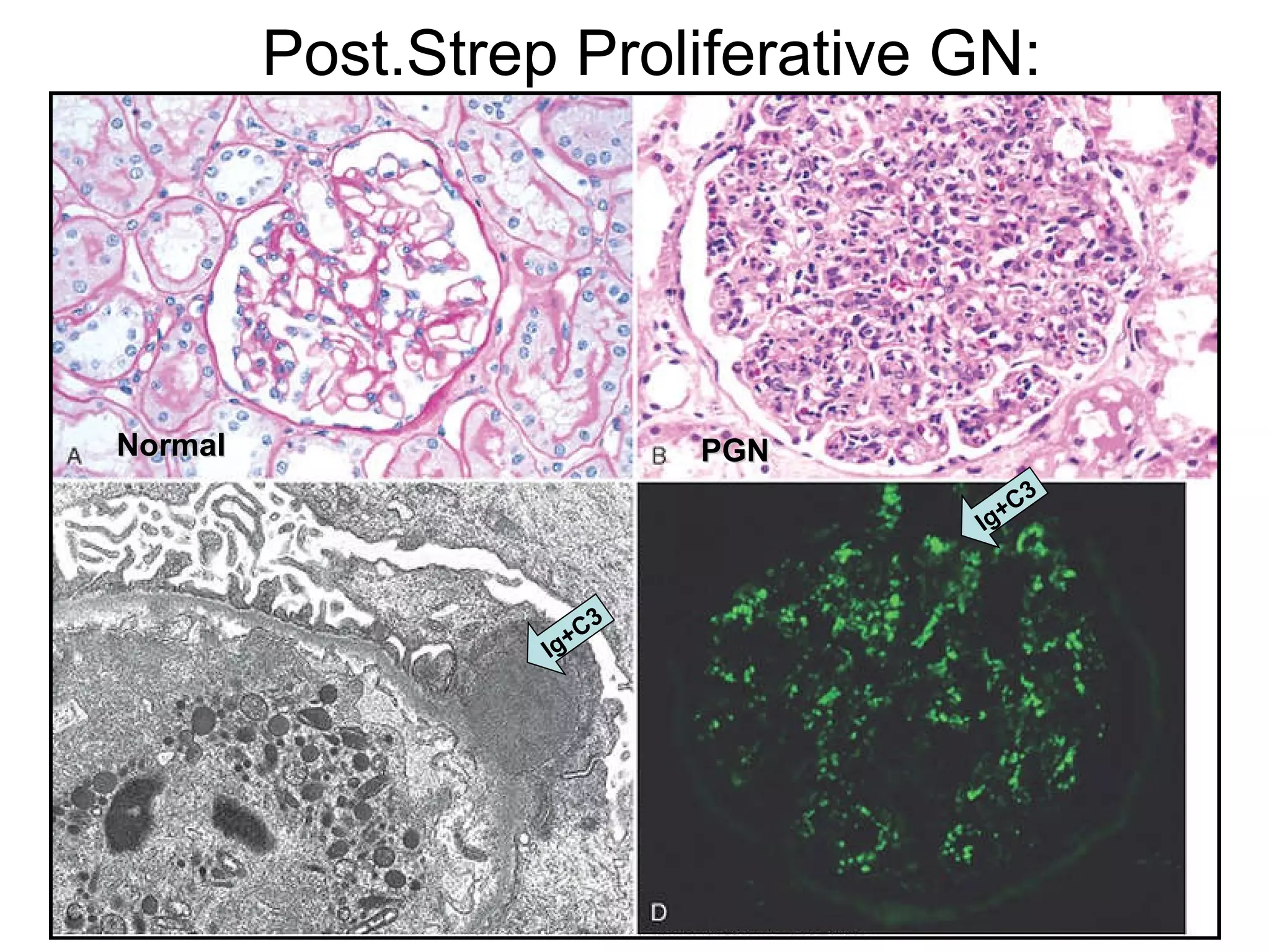
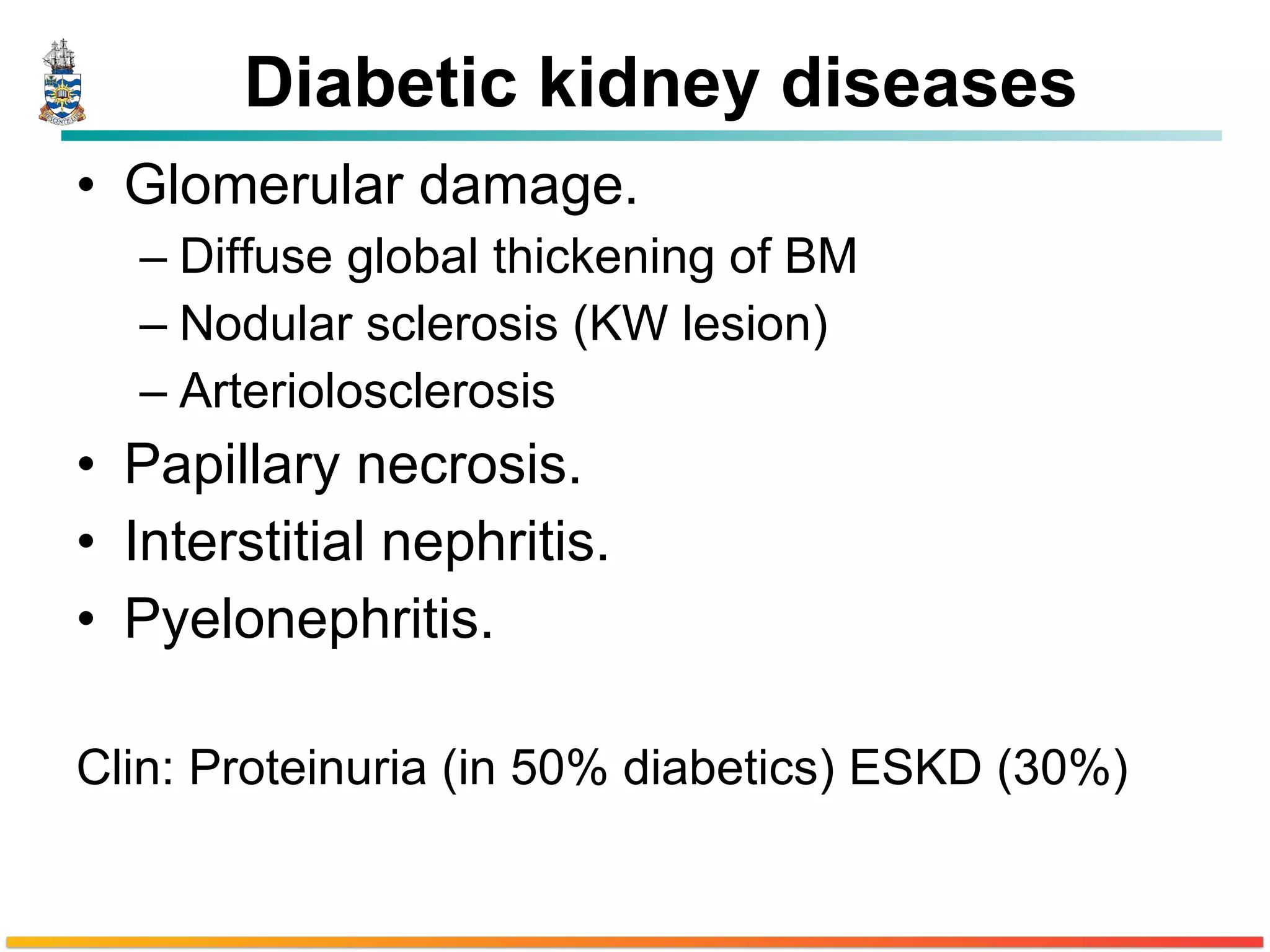
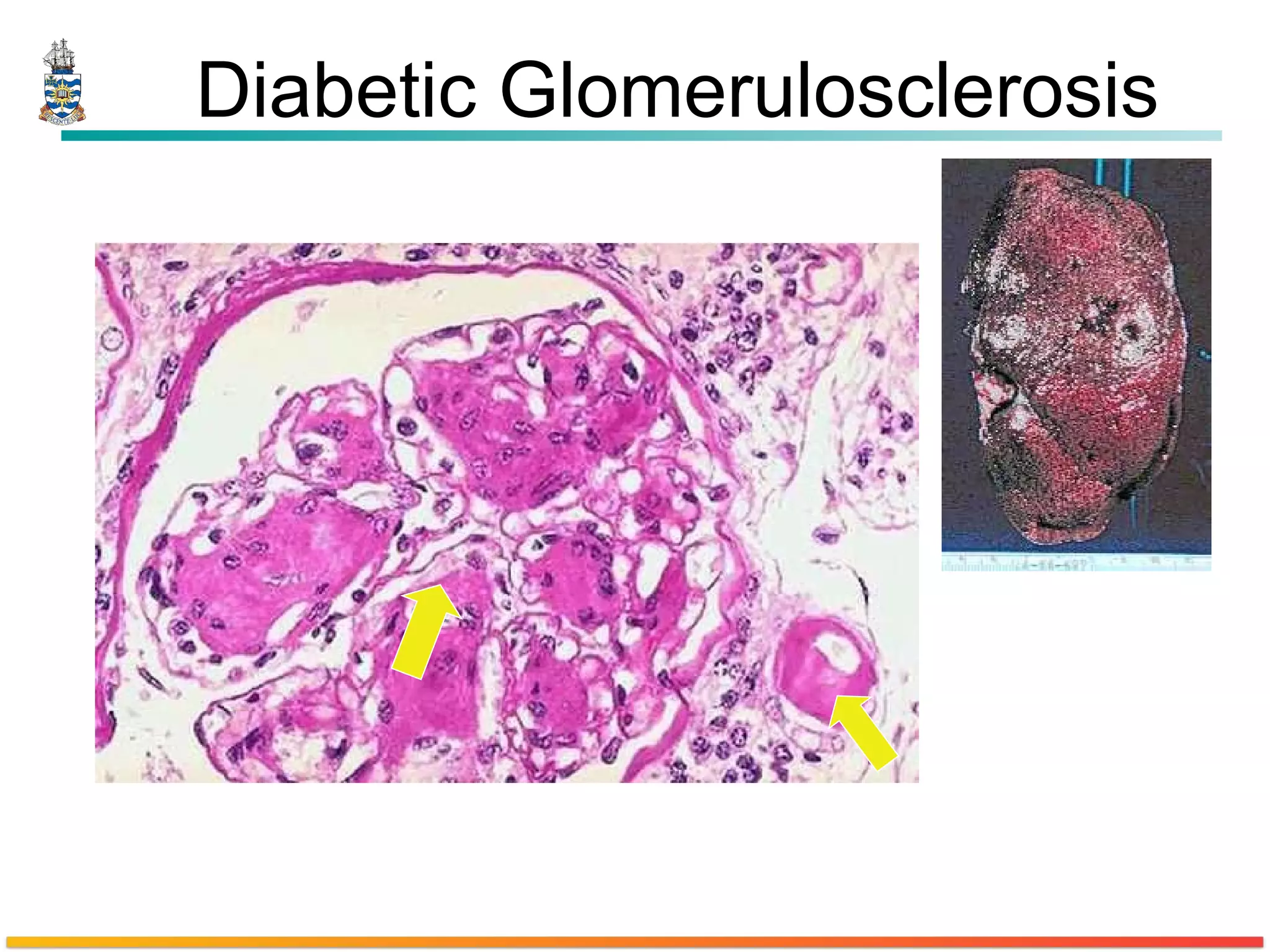
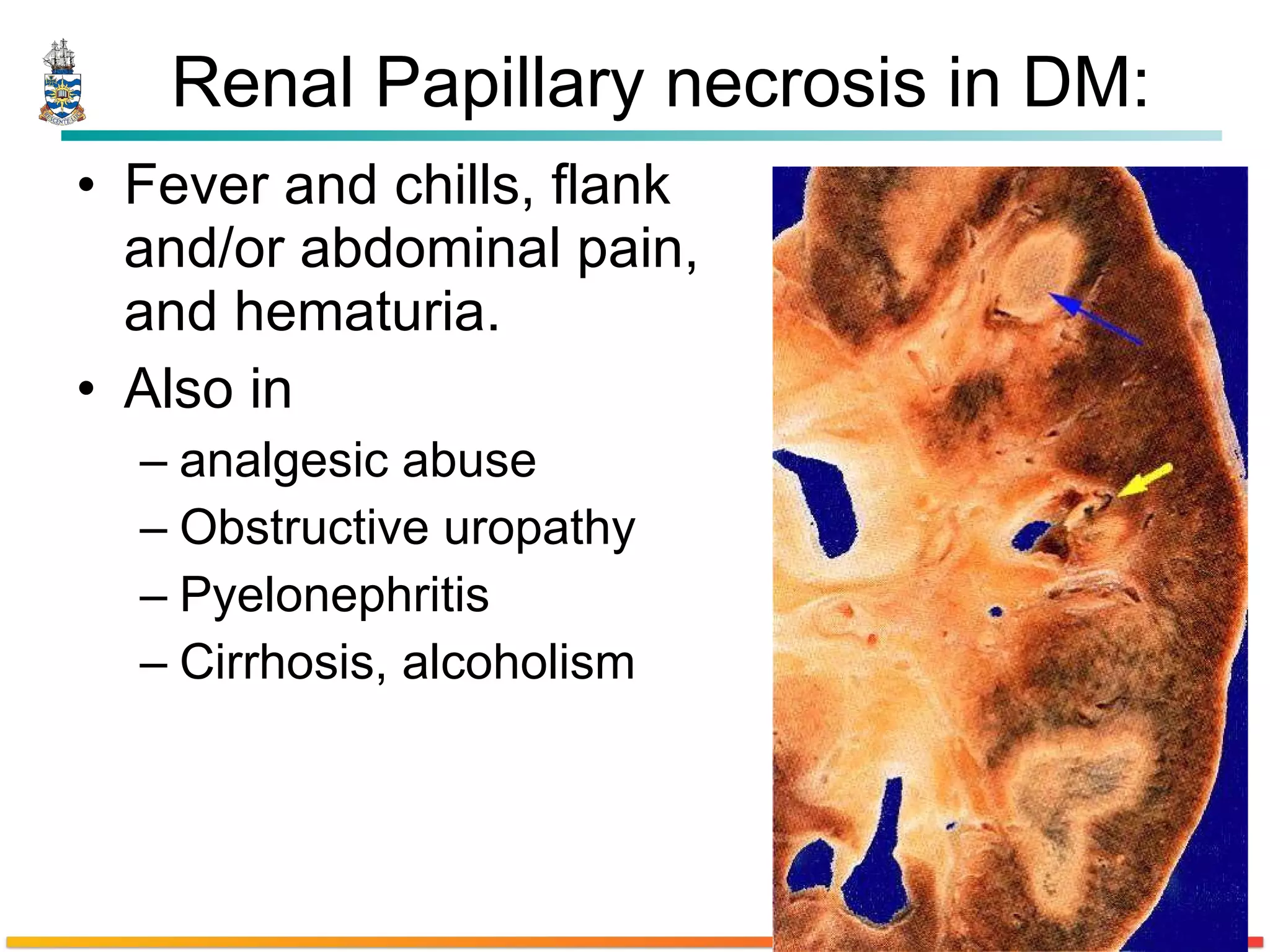
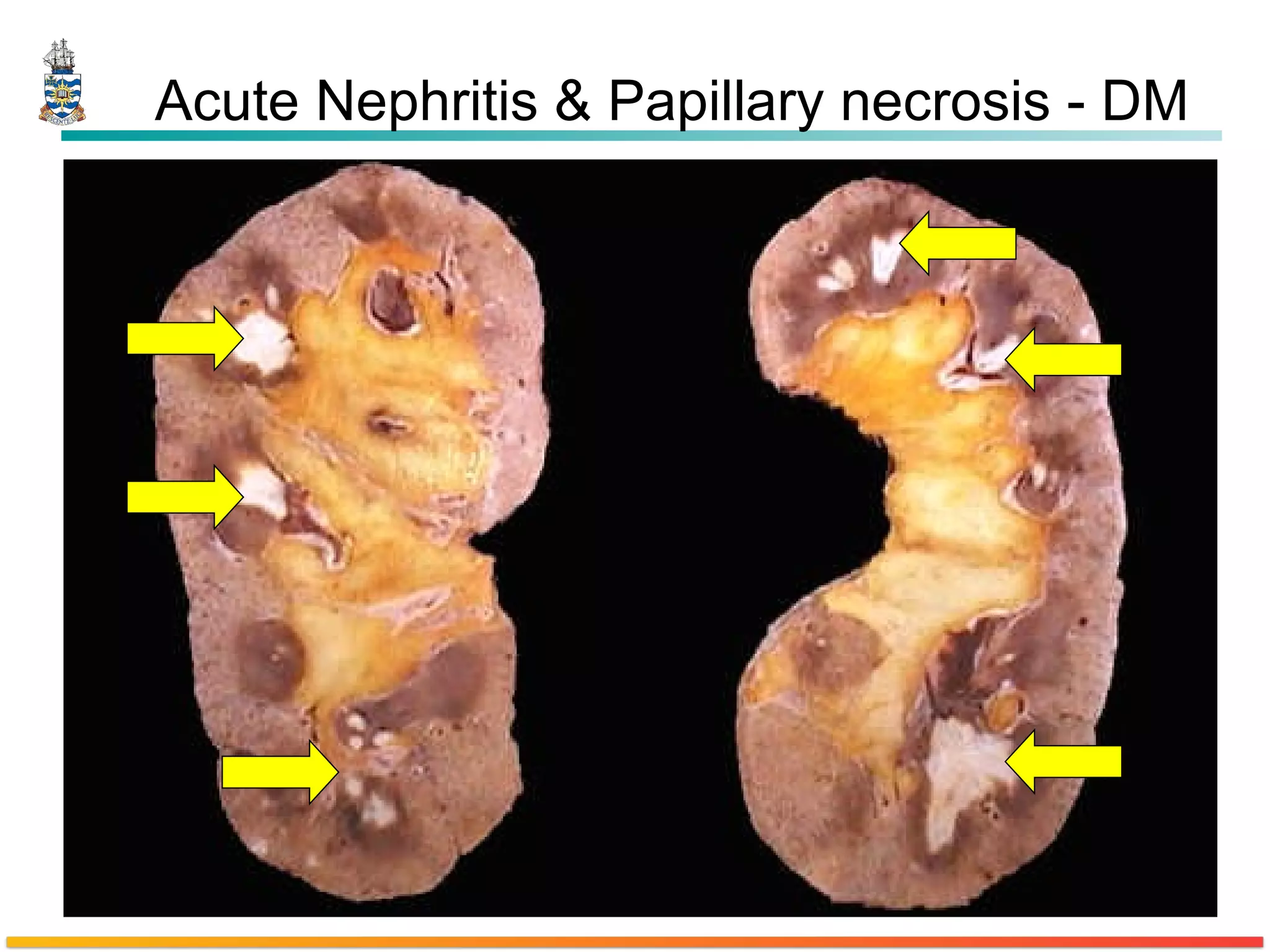
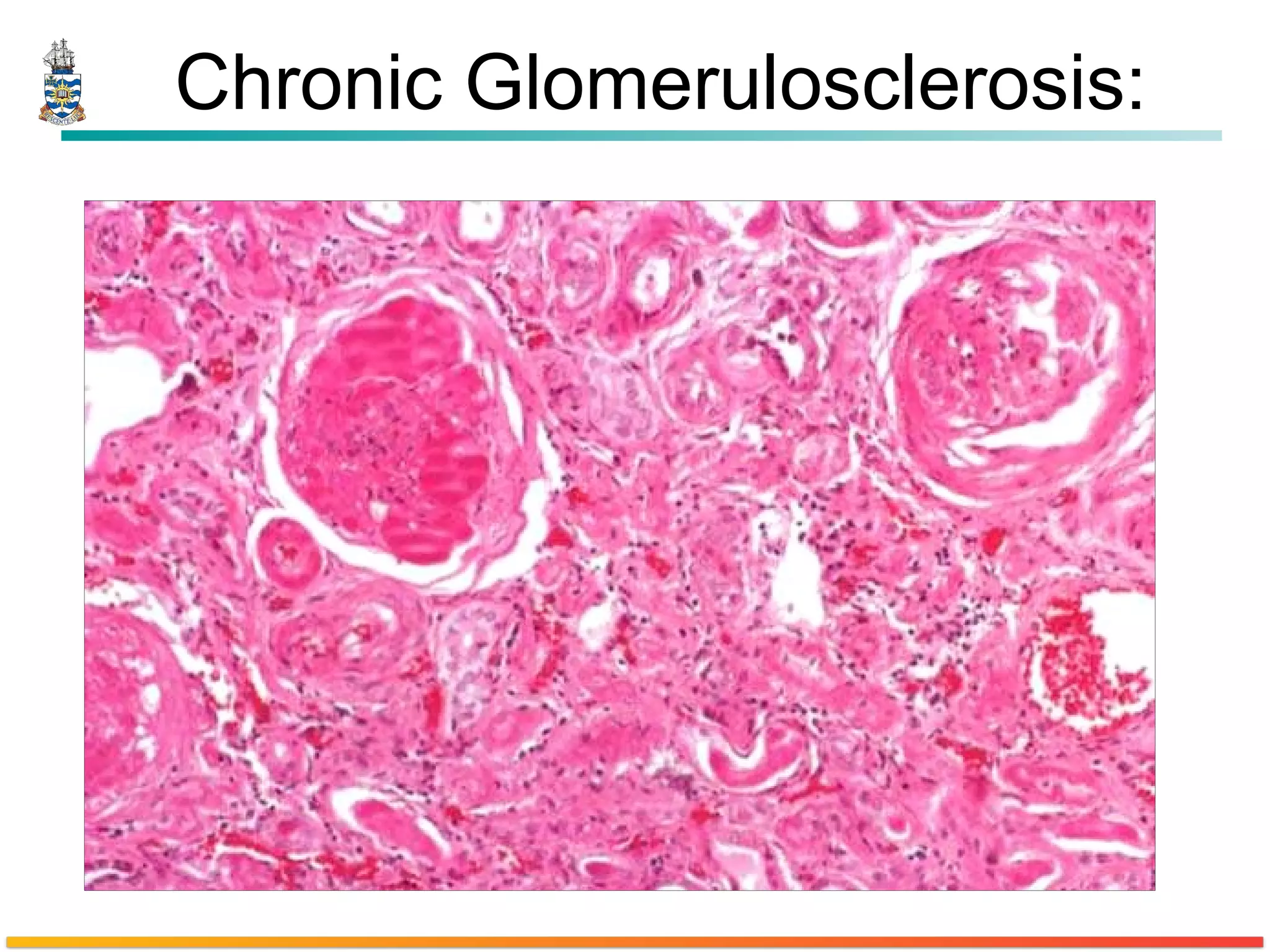
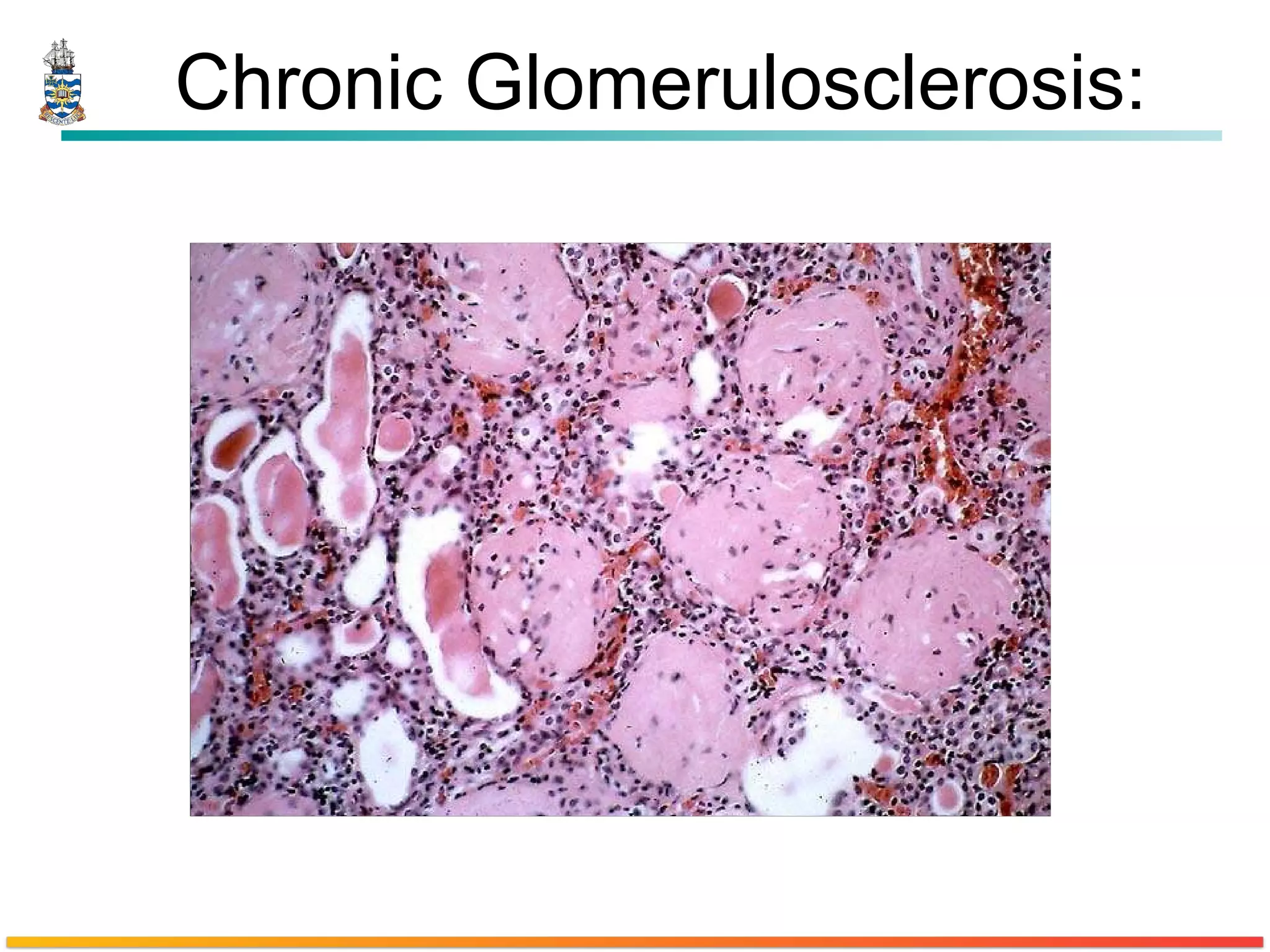
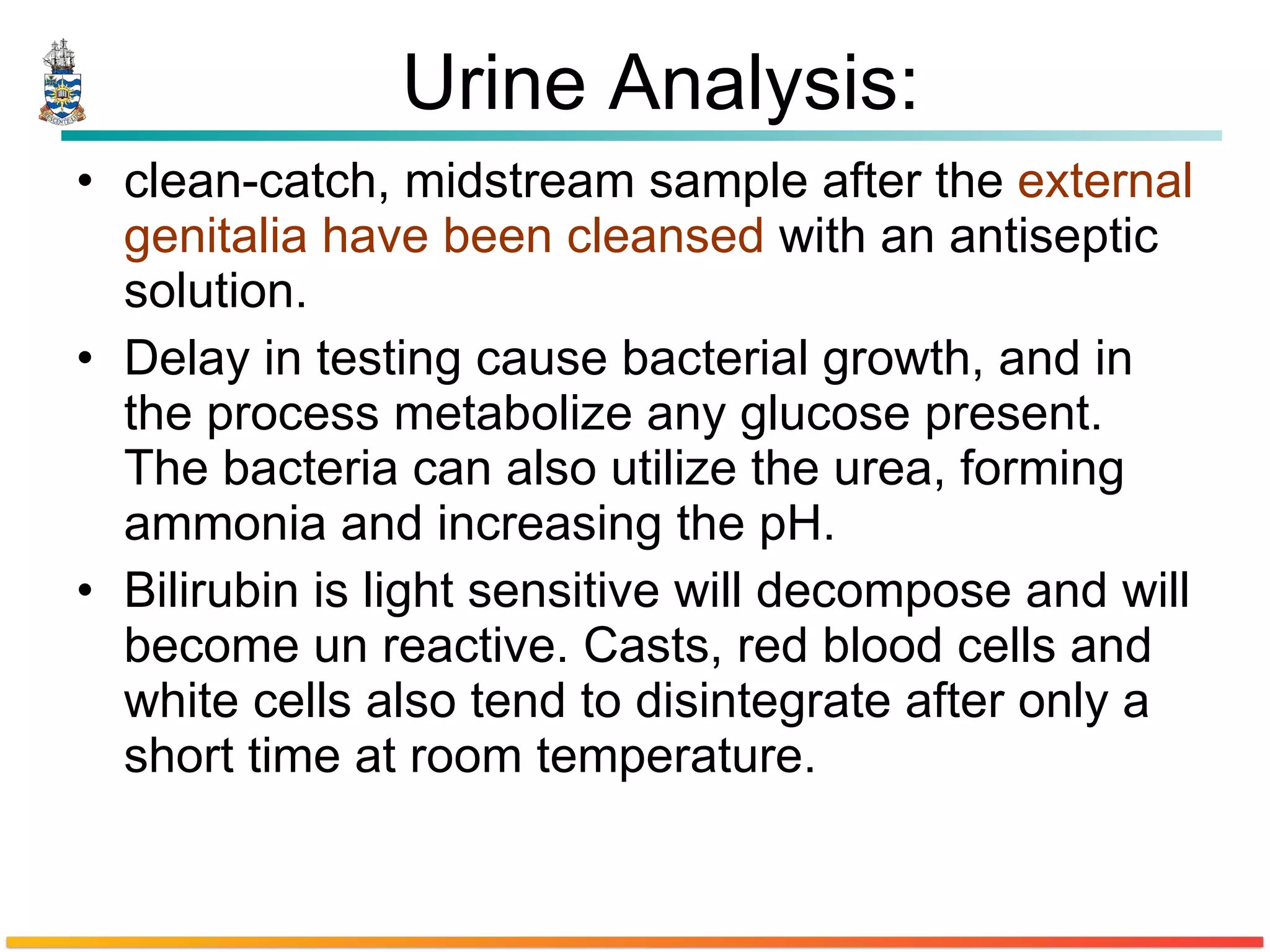
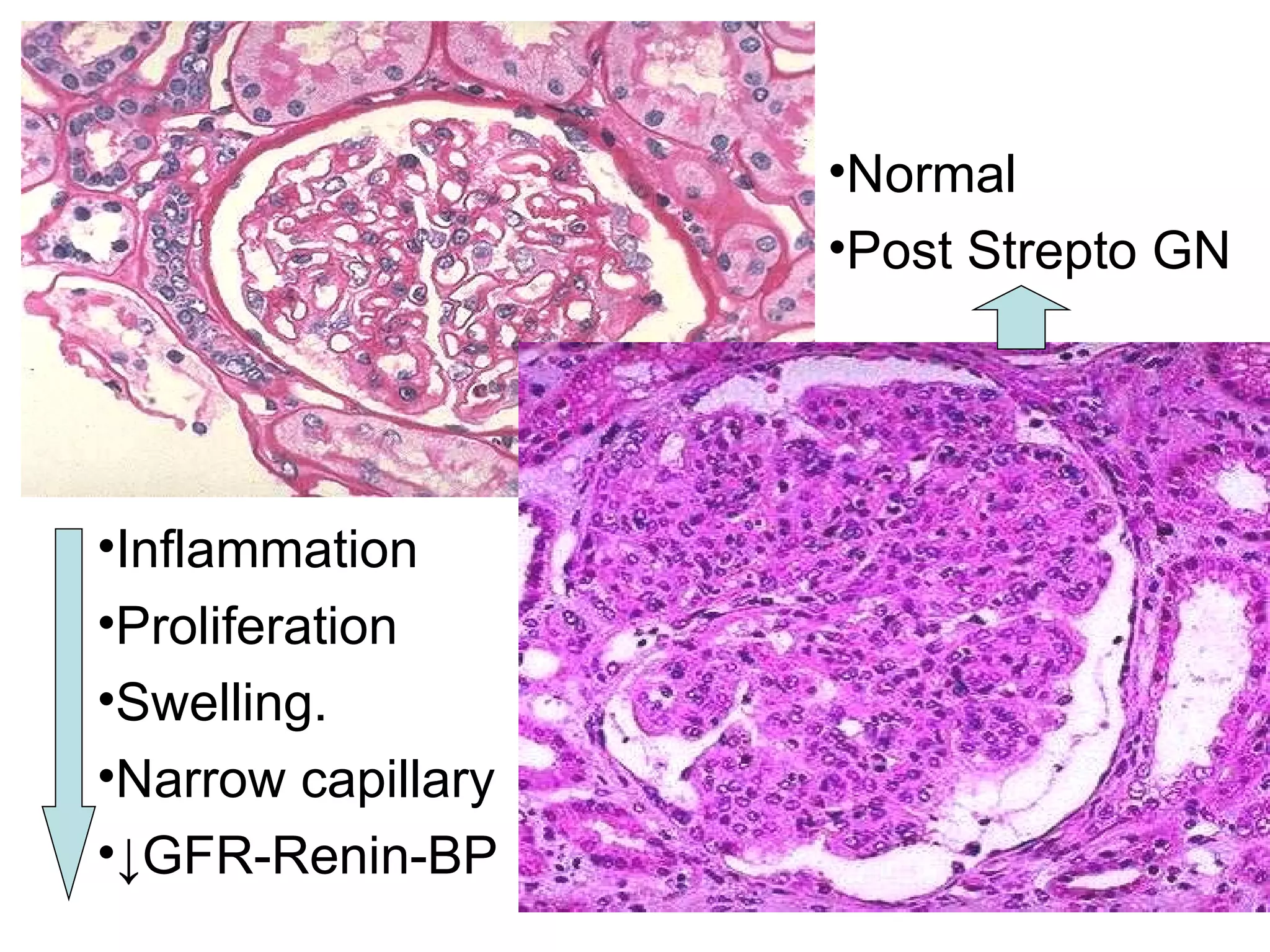
The document describes a case of a 37-year-old woman with type 1 diabetes presenting with various symptoms including dysuria, urinary frequency, fatigue, and edema. Laboratory tests showed elevated blood sugar, proteinuria, and urine positive for nitrates, ketones, glucose, protein, and red blood cells. A renal biopsy showed glomerulonephritis.