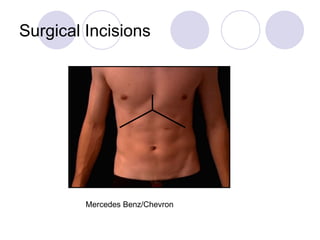
The document discusses surgical wounds and infections, detailing classifications of surgical procedures and the associated risks of wound infections. It covers stages of wound healing, types of tissue response to injury, the process of inflammation, and factors influencing scarring. Additionally, it provides guidelines for prevention, techniques for effective wound healing, and the management of abnormal scars.