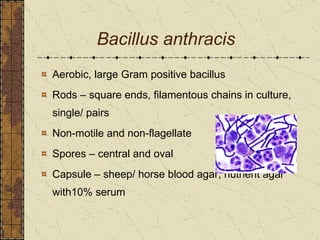
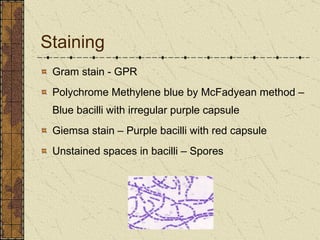
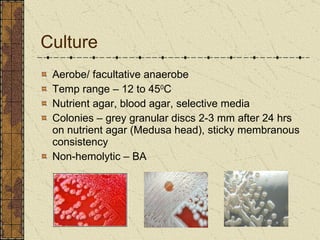
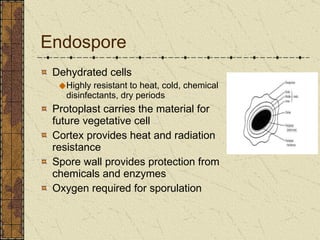
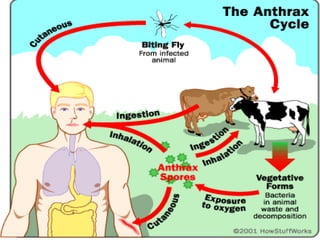
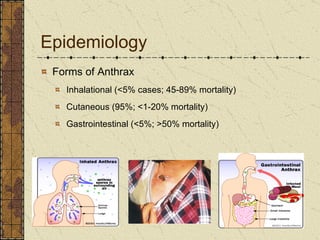
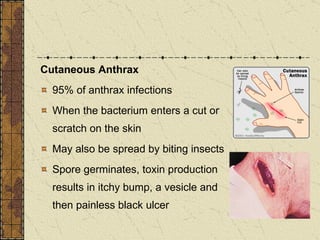
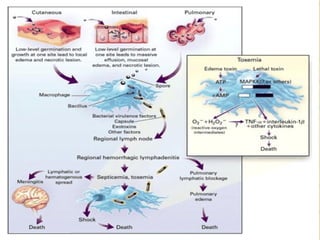
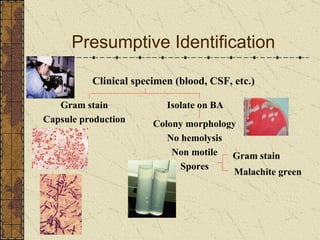
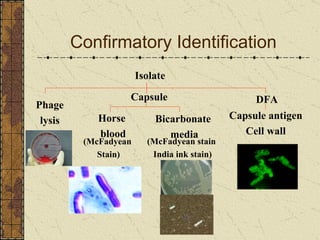
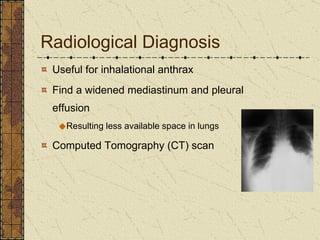
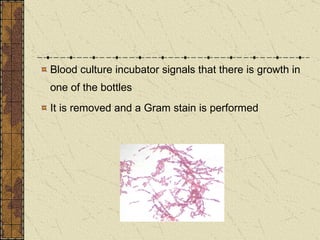
The document discusses Bacillus anthracis, the bacterium that causes anthrax. It describes the morphological and biochemical characteristics of B. anthracis, how it causes disease, methods for laboratory diagnosis of anthrax, treatment and post-exposure prophylaxis. It also discusses anthrax as a potential biological warfare agent and Pakistan's experience investigating suspected anthrax cases after 2001.