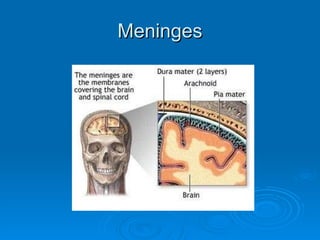
This document provides an overview of central nervous system (CNS) infections, including:
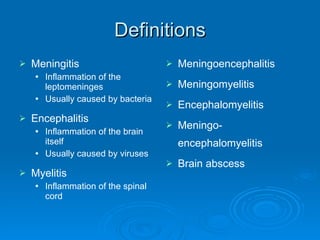
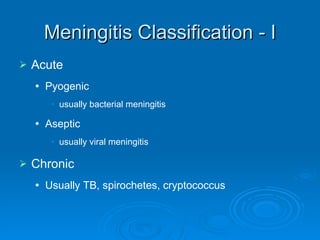
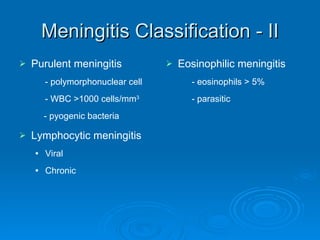
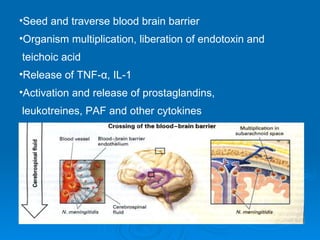
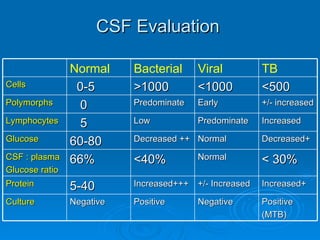
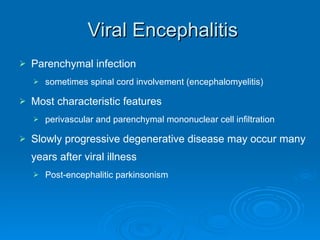
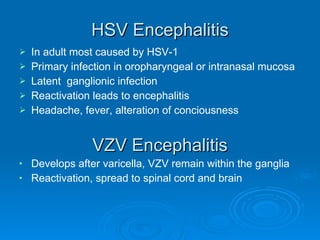
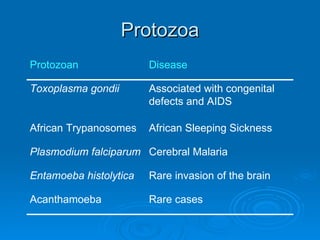
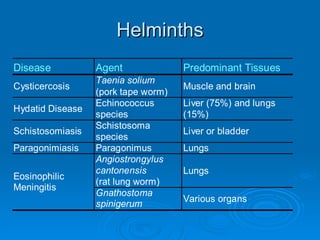
1. CNS infections can be classified by the organ involved (e.g. meningitis, encephalitis) or by pathogen (e.g. bacteria, viruses, fungi).
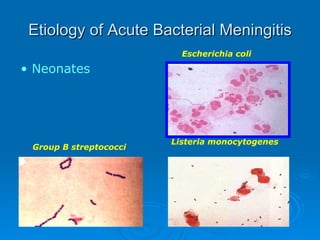
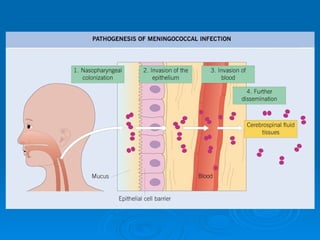
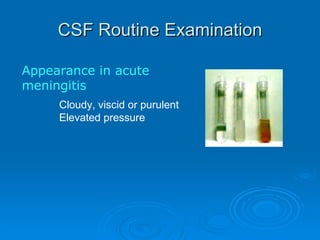
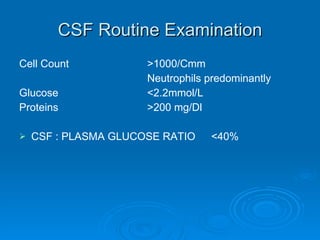
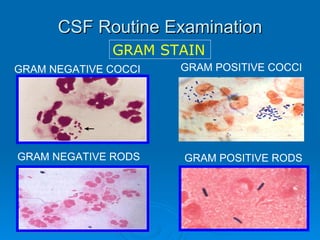
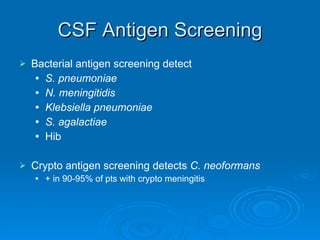
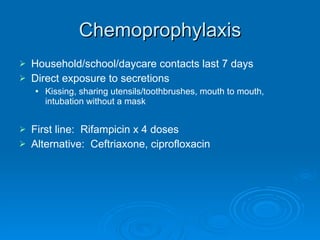
2. Common causes of acute bacterial meningitis include Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. Viral meningitis is usually caused by enteroviruses.
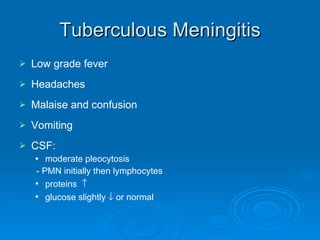
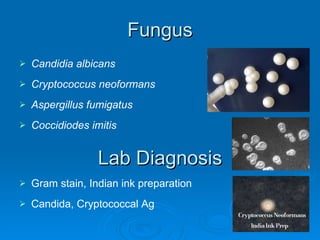
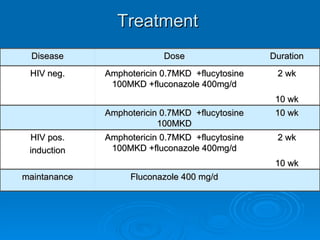
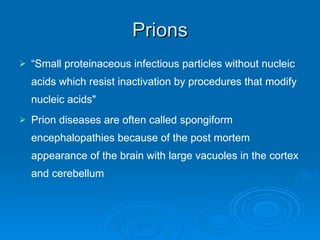
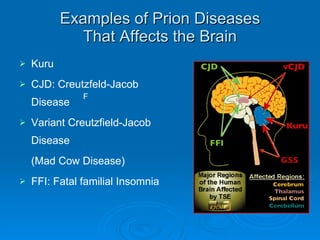
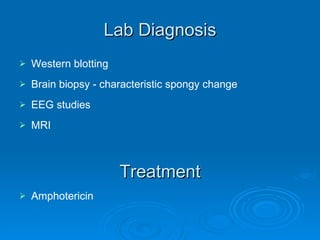
3. Chronic CNS infections include tuberculosis (TB), neurosyphilis, fungal infections (e.g. cryptococcosis), and prion diseases (e.g. Cre