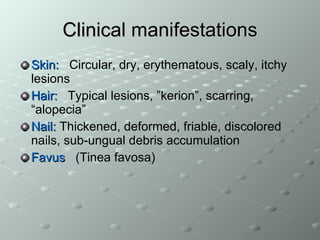
1. The document discusses various types of tinea or dermatophytosis, a fungal infection of the skin, hair, and nails, caused by dermatophyte fungi including Trichophyton, Epidermophyton, and Microsporum genera.
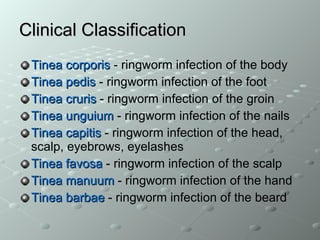
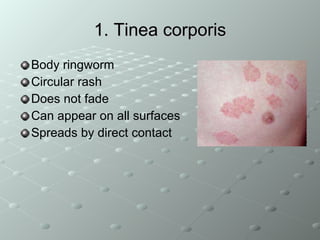
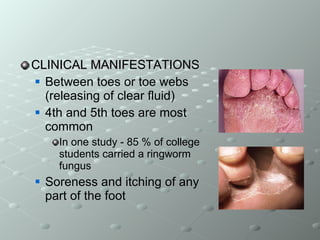
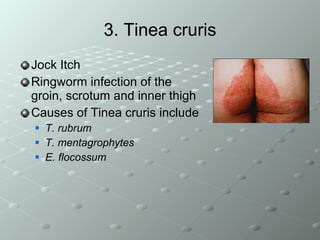
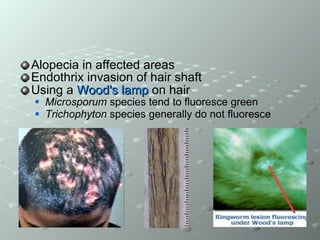
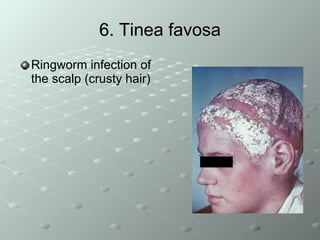
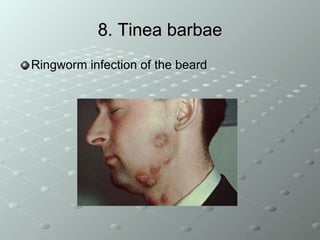
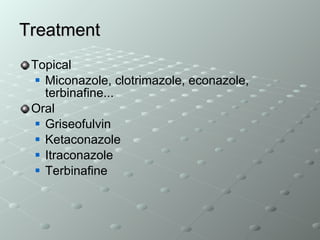
2. It describes the clinical manifestations and treatment of common types of tinea infections such as tinea corporis (ringworm of the body), tinea pedis (athlete's foot), tinea cruris (jock itch), tinea unguium (nail infection), tinea capitis (ringworm of the scalp), and tinea barbae (ringworm of the beard).
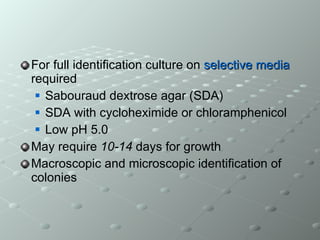
3. Laboratory