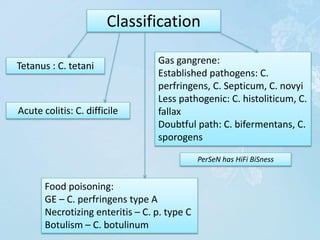
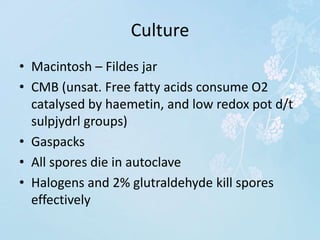
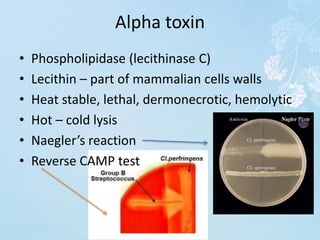
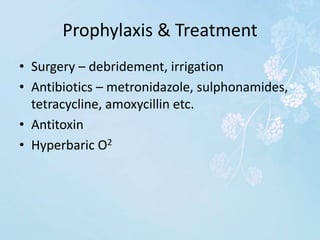
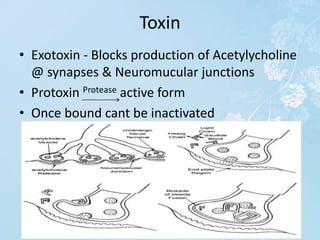
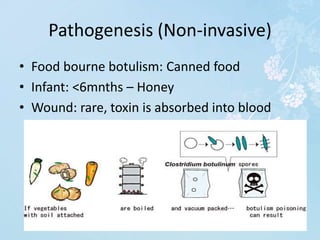
Clostridium are anaerobic, spore-forming bacteria found in soil and the gastrointestinal tract of humans and animals. Certain Clostridium species cause diseases like tetanus, gas gangrene, and food poisoning. They produce potent exotoxins and can be diagnosed through gram staining, culture techniques, and toxin detection assays. Treatment involves surgery, antibiotics, antitoxins, and in some cases hyperbaric oxygen therapy. Vaccination provides protection against tetanus.