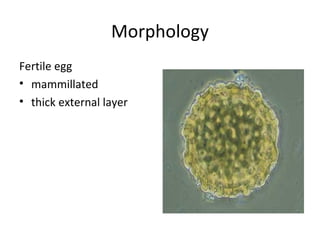
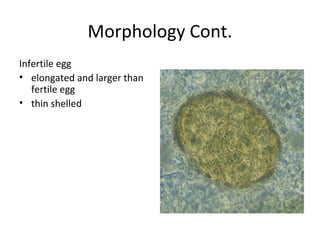
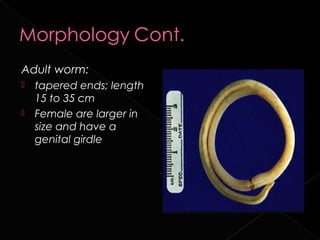
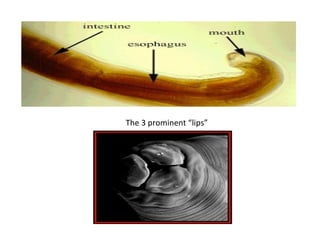
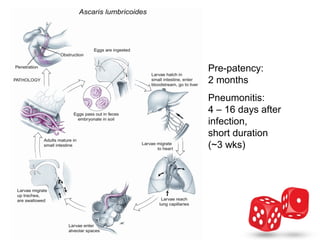
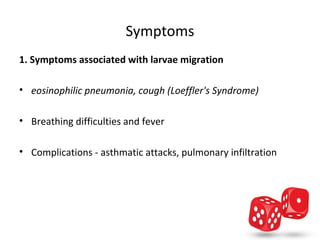
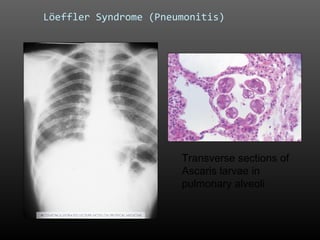
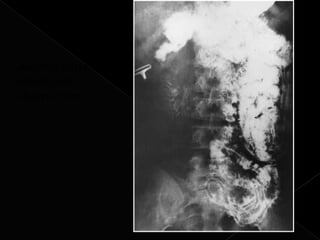
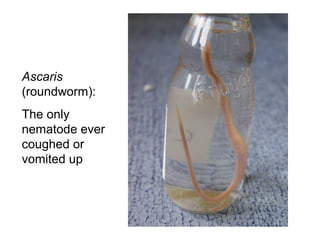
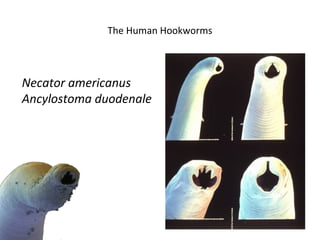
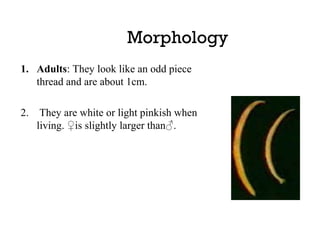
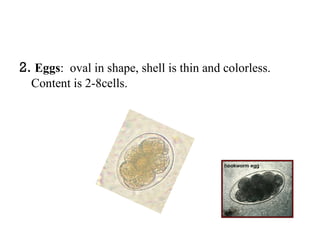
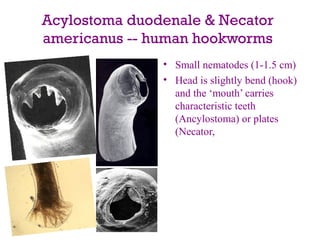
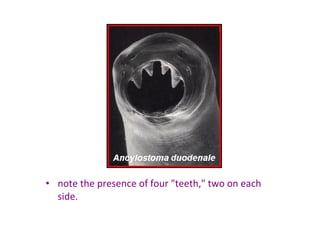
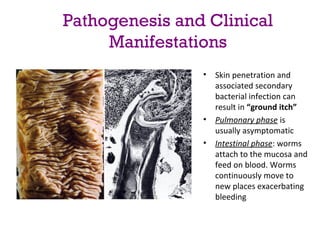
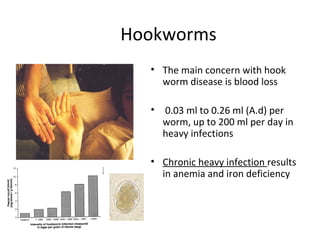
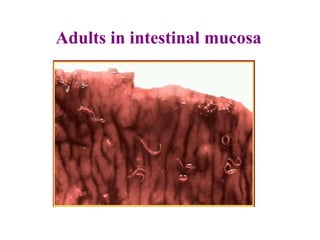
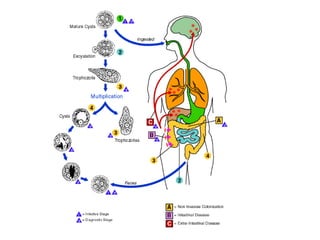
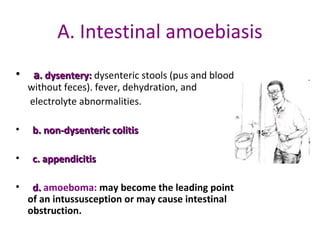
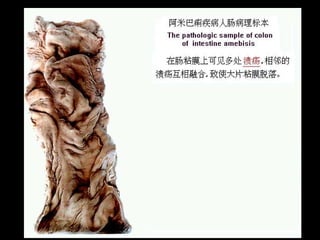
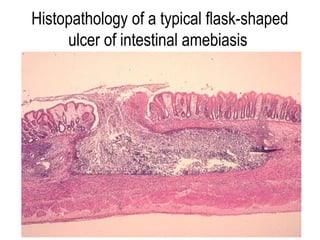
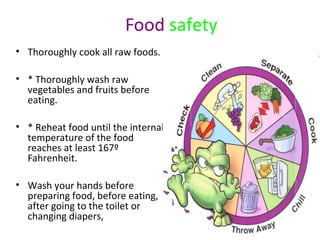
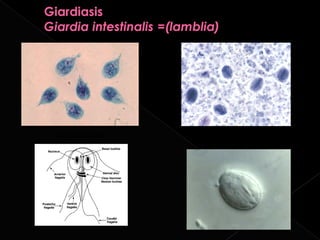
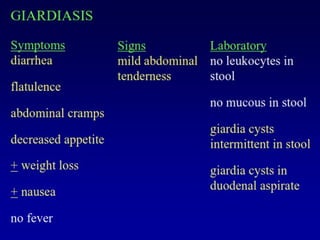
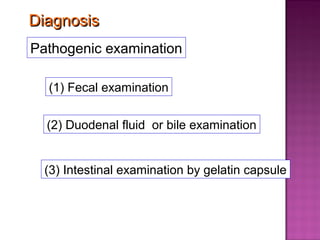
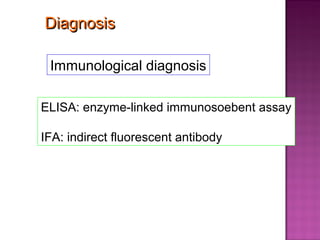
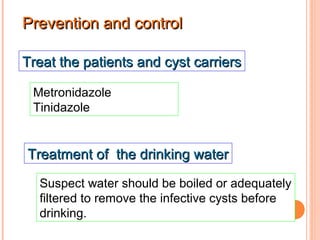
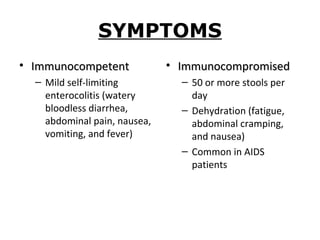
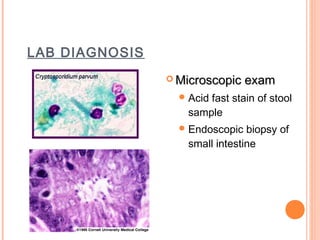
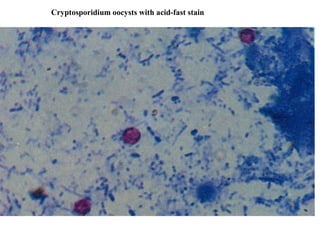
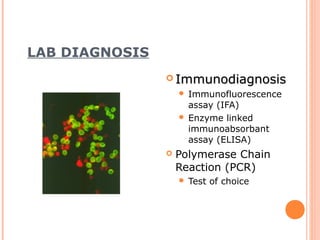
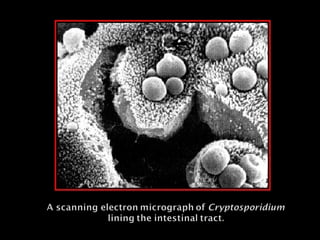
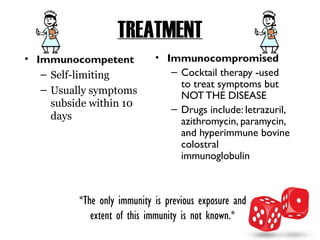
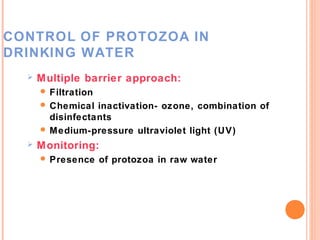
The document discusses several intestinal protozoa and helminths including Ascaris lumbricoides, hookworms, Entamoeba histolytica, Giardia lamblia, and Cryptosporidium. It describes the morphology, life cycles, transmission routes, clinical manifestations, diagnosis, and treatment of each parasite. Prevention focuses on proper sanitation, hygiene practices like handwashing, water treatment, and health education.