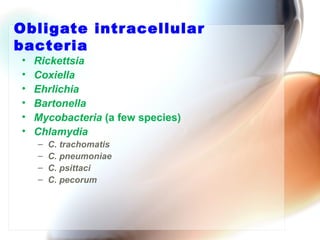
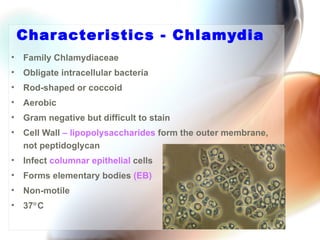
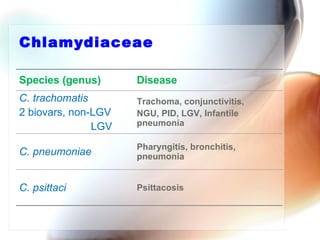
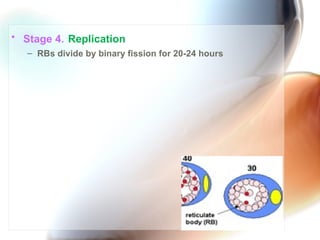
Chlamydia is an obligate intracellular bacterium that causes trachoma, a leading cause of preventable blindness, as well as sexually transmitted diseases like pelvic inflammatory disease; it has a unique developmental cycle alternating between infectious elementary bodies and metabolically active reticulate bodies; symptoms can range from eye infections to urethritis and proctitis depending on the Chlamydia species.