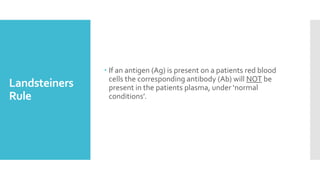
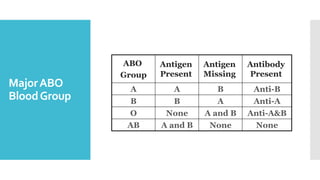
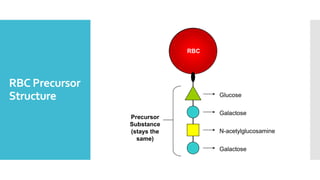
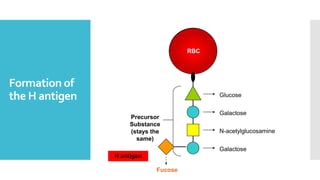
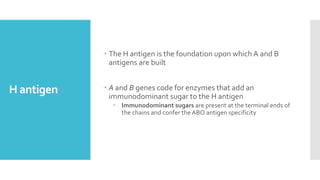
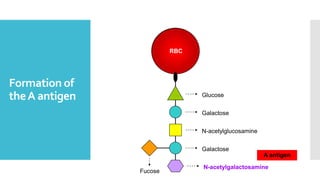
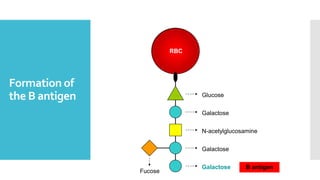
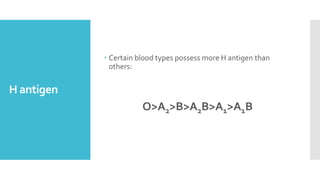
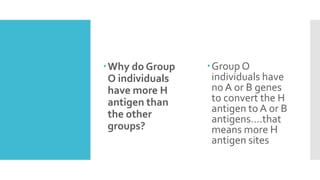
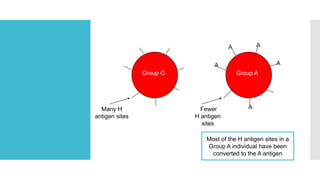
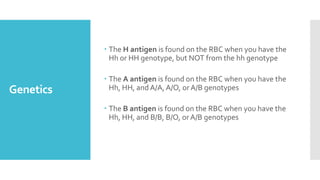
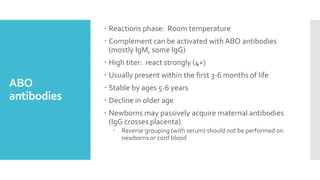
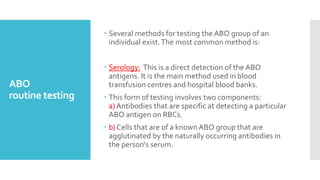
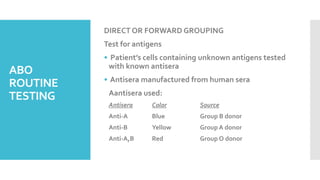
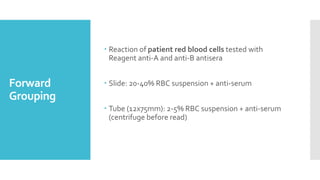
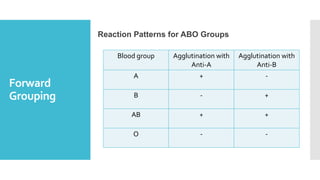
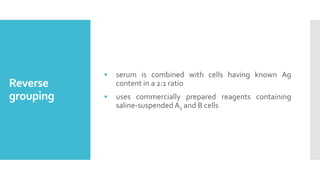
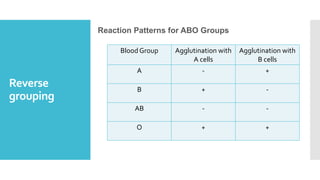
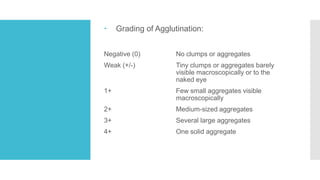
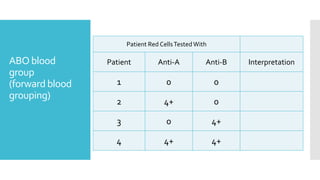
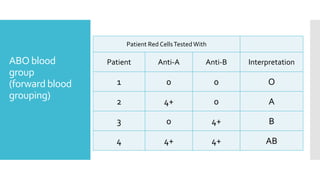
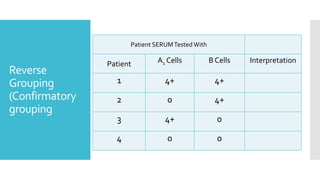
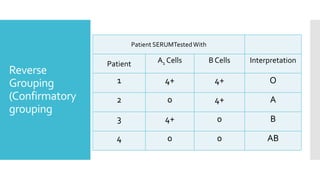
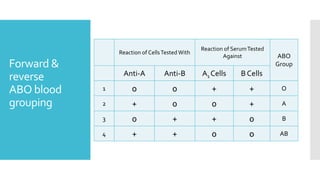
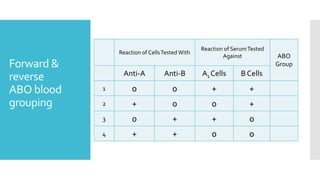
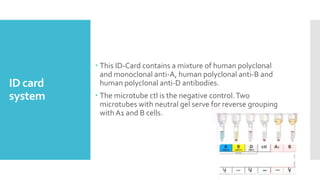
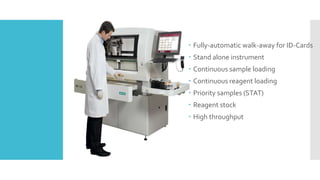
The document summarizes the history and science behind blood grouping and the ABO blood group system. It describes how Karl Landsteiner discovered the major ABO blood groups in 1901. It explains the antigens and antibodies present in each blood group according to Landsteiner's rule. The genetics and biochemistry of the ABO blood group system are covered, including how the H, A, and B antigens are synthesized on red blood cells. Common blood grouping techniques like forward and reverse grouping are also summarized.