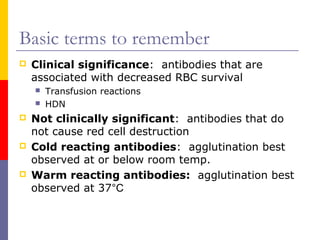
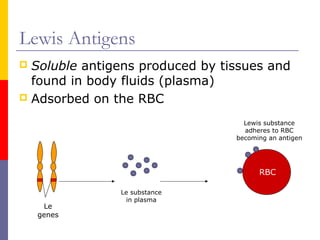
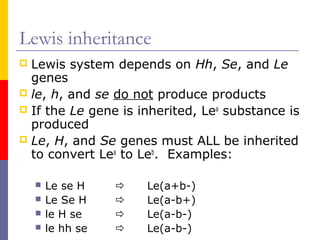
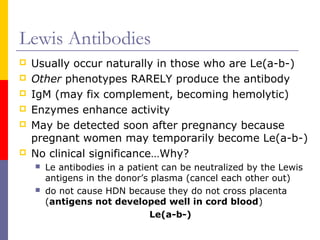
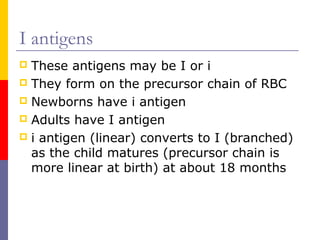
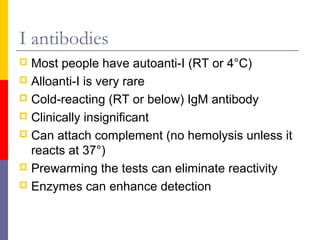
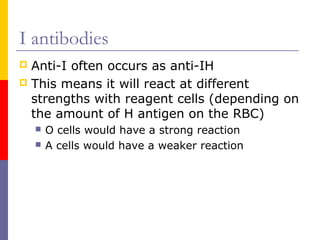
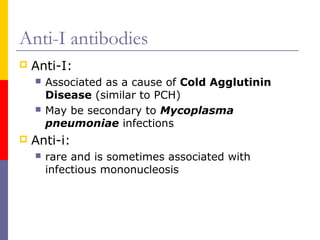
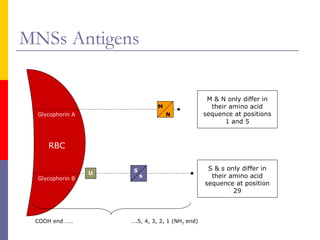
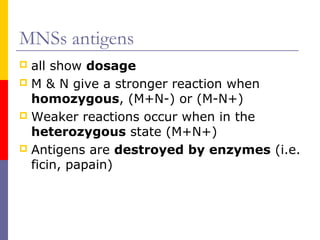
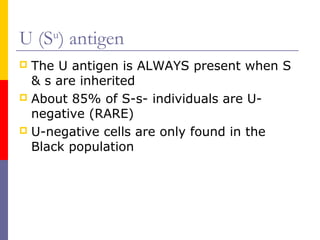
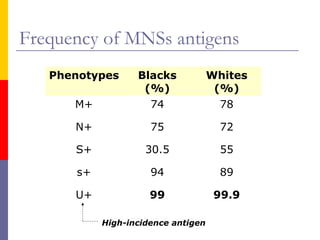
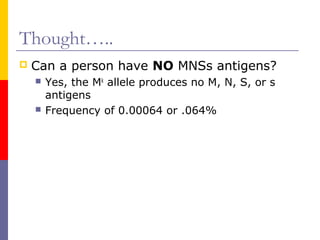
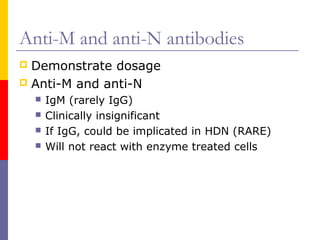
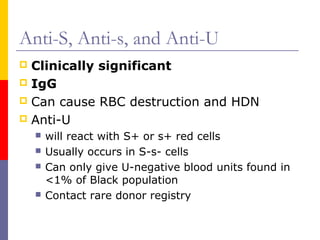
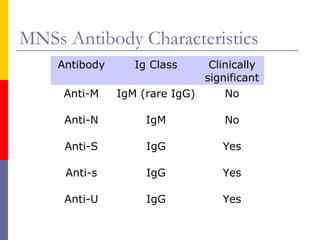
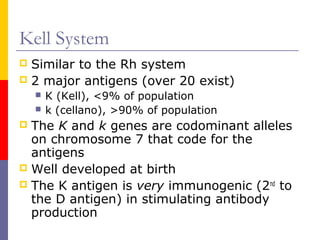
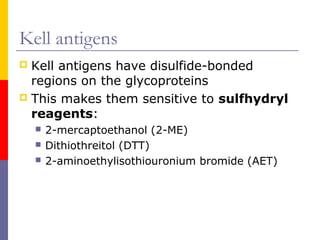
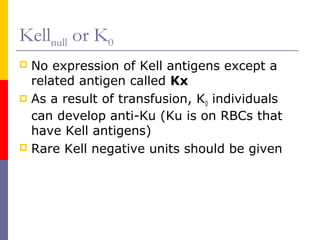
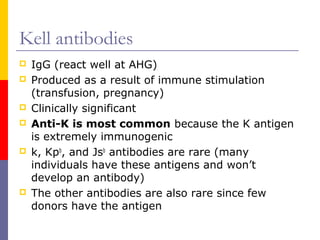
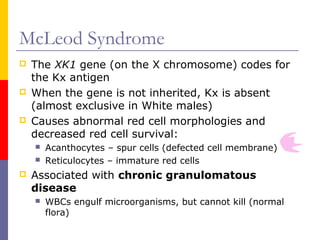
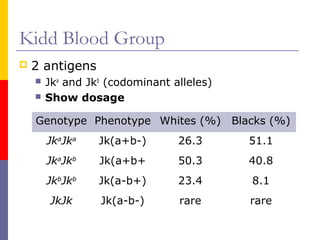
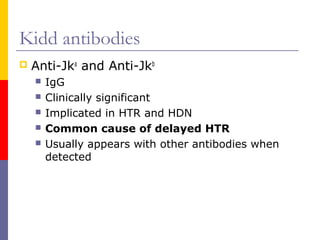
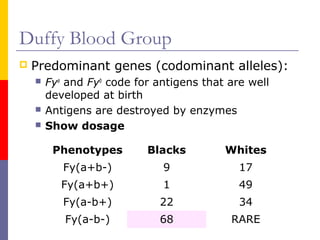
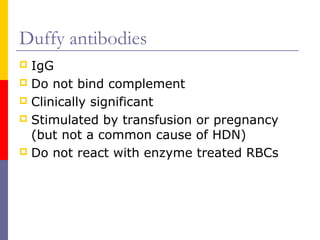
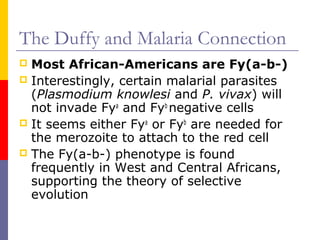
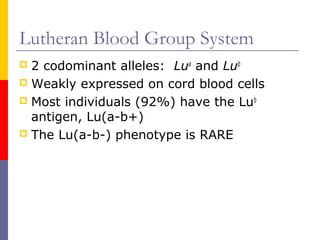
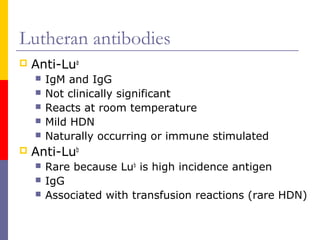
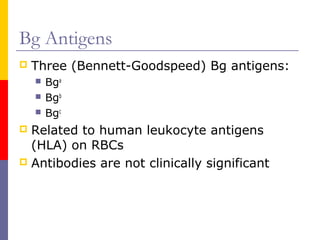
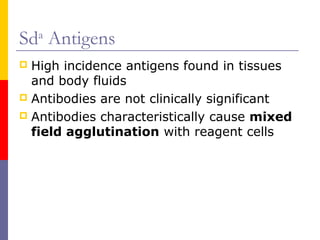
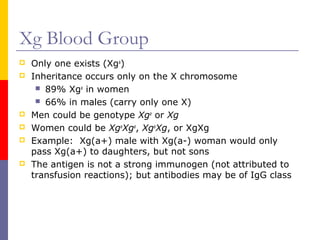
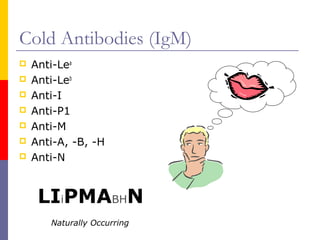
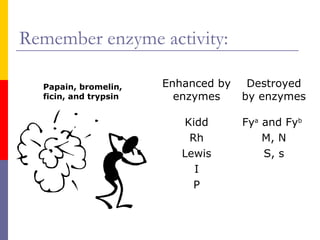
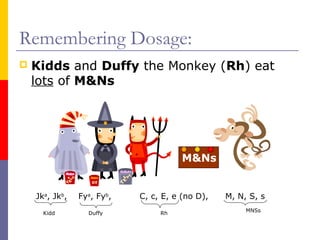
This document discusses several major blood group systems including Lewis, I, P, MNSs, Kell, Kidd, Duffy, Lutheran, Bg, Sda, and Xg. It provides information on the antigens and genes involved in each system, the clinical significance of associated antibodies, and inheritance patterns. Some key points covered include that Lewis, I, and P antigens produce cold-reacting antibodies while Kell, Kidd, and Duffy produce warm-reacting antibodies. The MNSs, Kell, and Kidd systems can produce clinically significant antibodies implicated in hemolytic transfusion reactions and hemolytic disease of the newborn.