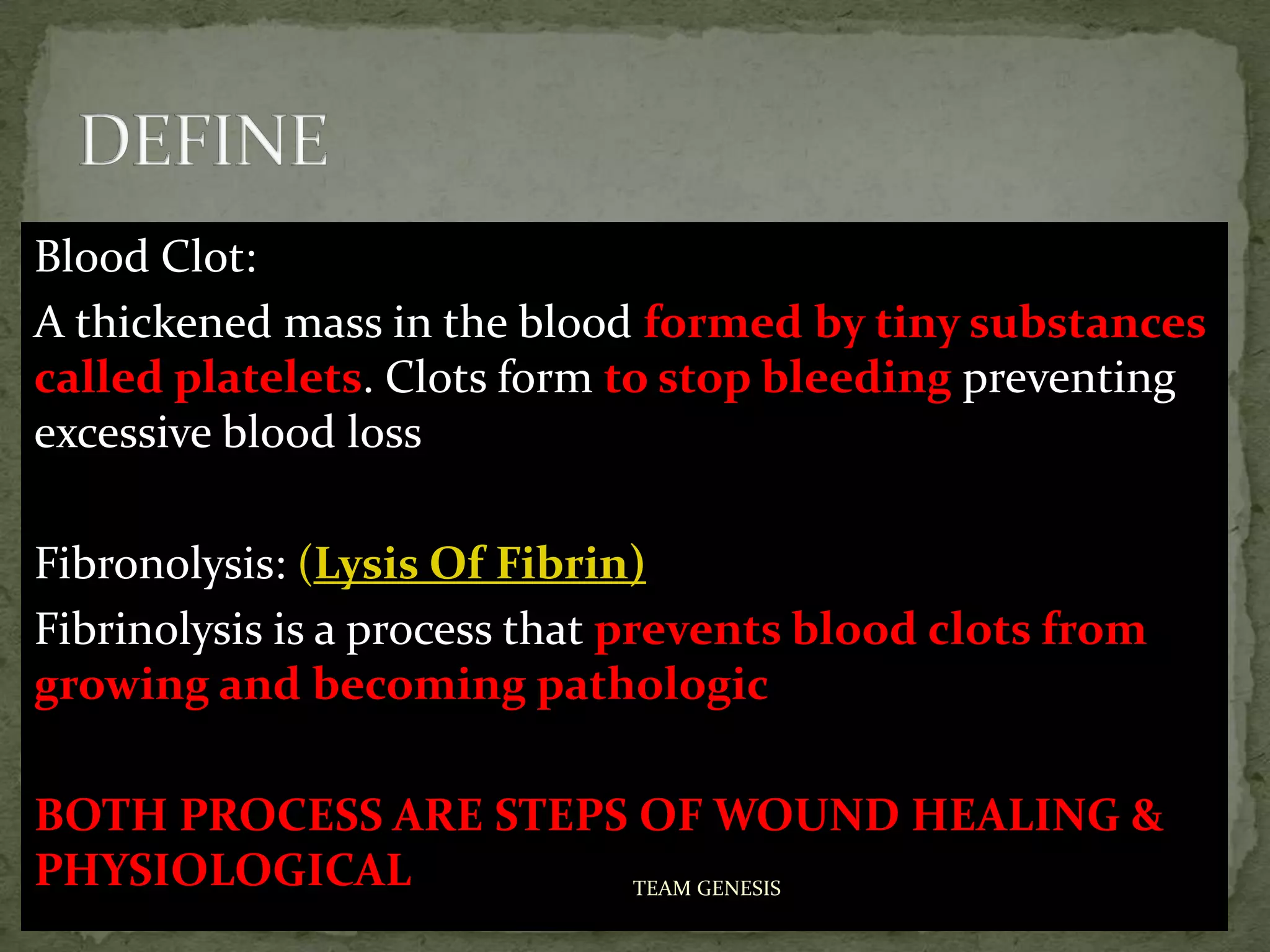
This document discusses the processes of hemostasis, thrombosis, and fibrinolysis. It defines key terms like blood clot, platelet, fibrin, coagulation cascade, and anticoagulants. The document describes the steps of primary hemostasis which involves platelet adhesion and activation at the site of injury. It also outlines the secondary hemostasis process known as the coagulation cascade that generates thrombin and ultimately forms a fibrin clot to stop bleeding. The roles of fibrinolysis and anticoagulant pathways in regulating clot formation are also summarized.