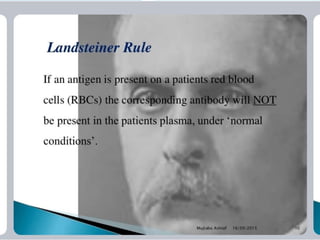
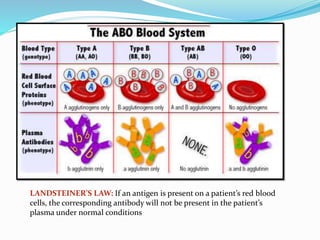
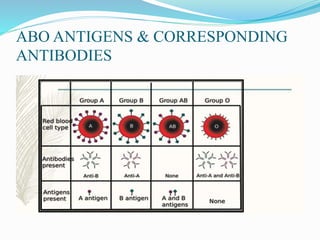
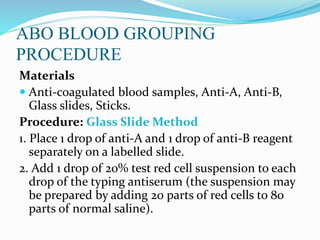
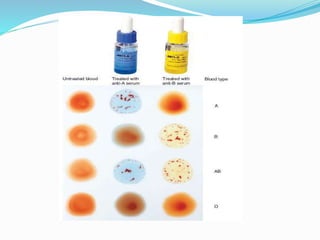
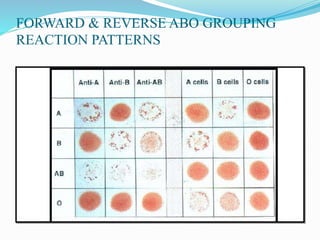
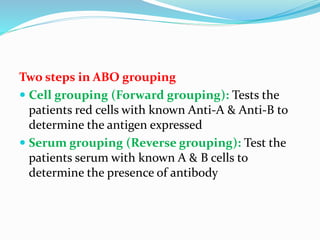
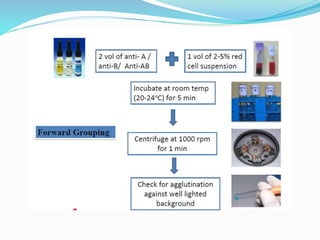
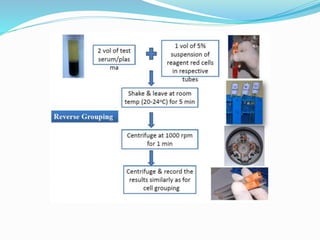
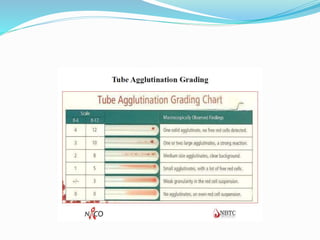
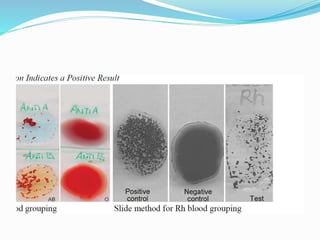
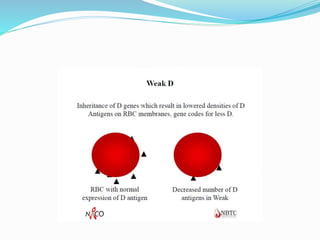
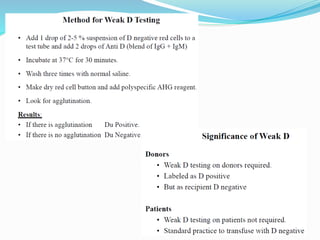
This document discusses the importance of blood grouping and provides information about ABO and Rh blood group systems. It explains that blood grouping is done to ensure safe blood transfusions, as incompatible blood types can cause agglutination of red blood cells. ABO blood grouping identifies the presence of A and B antigens on red blood cells and corresponding anti-A and anti-B antibodies in plasma. Rh blood grouping identifies the presence of the RhD antigen. The document outlines the procedures for performing forward and reverse blood grouping to determine a person's blood type according to these systems. It also discusses some rare blood types like the Bombay phenotype.