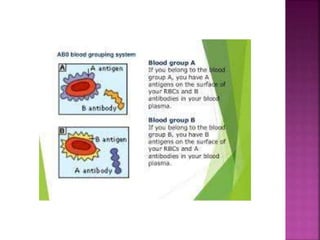
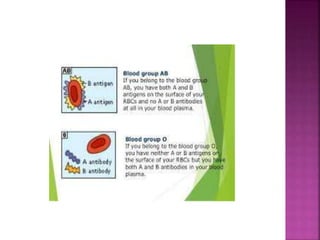
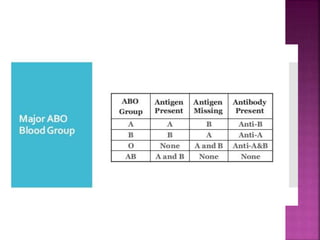
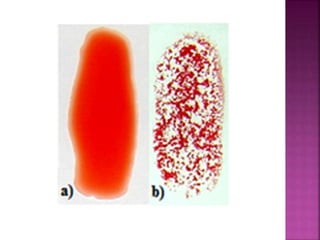
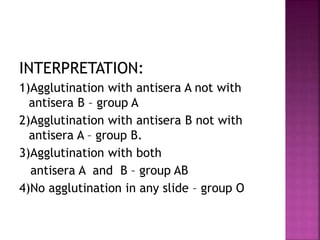
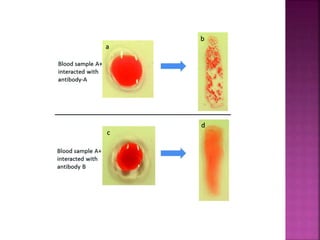
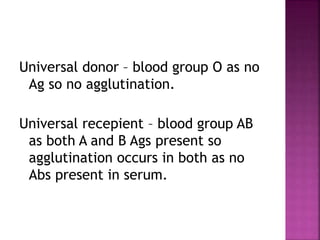
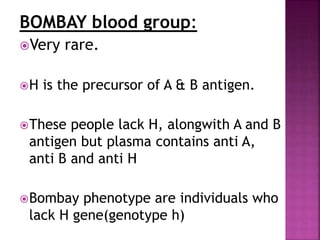
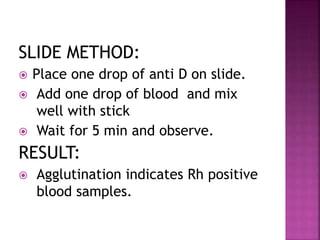
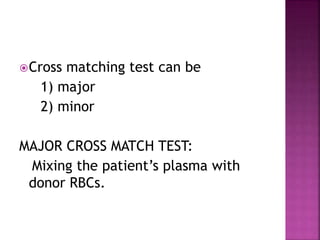
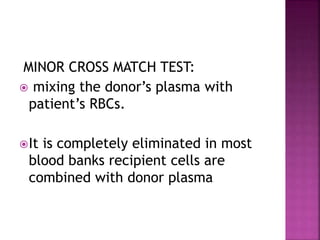
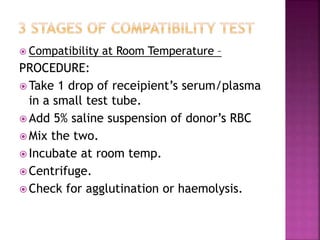
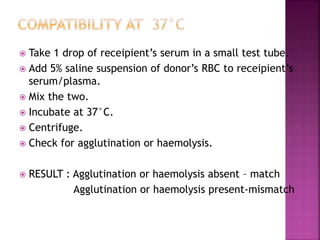
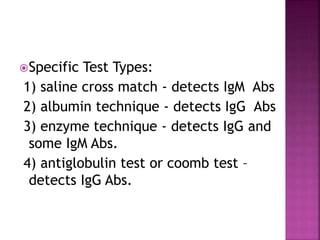
This document discusses blood grouping and Rh typing. It begins by explaining that blood grouping is based on the antigens present on red blood cells, with ABO and Rh being clinically most important. It then covers the history and discovery of blood grouping, the various blood group systems, and Landsteiner's law regarding antigens and antibodies. The rest of the document discusses methods for blood grouping and Rh typing, including slide and tube methods. It covers interpretation of results, universal donor/recipient groups, and rare Bombay blood group. The importance and techniques of cross-matching for blood transfusions are also summarized.