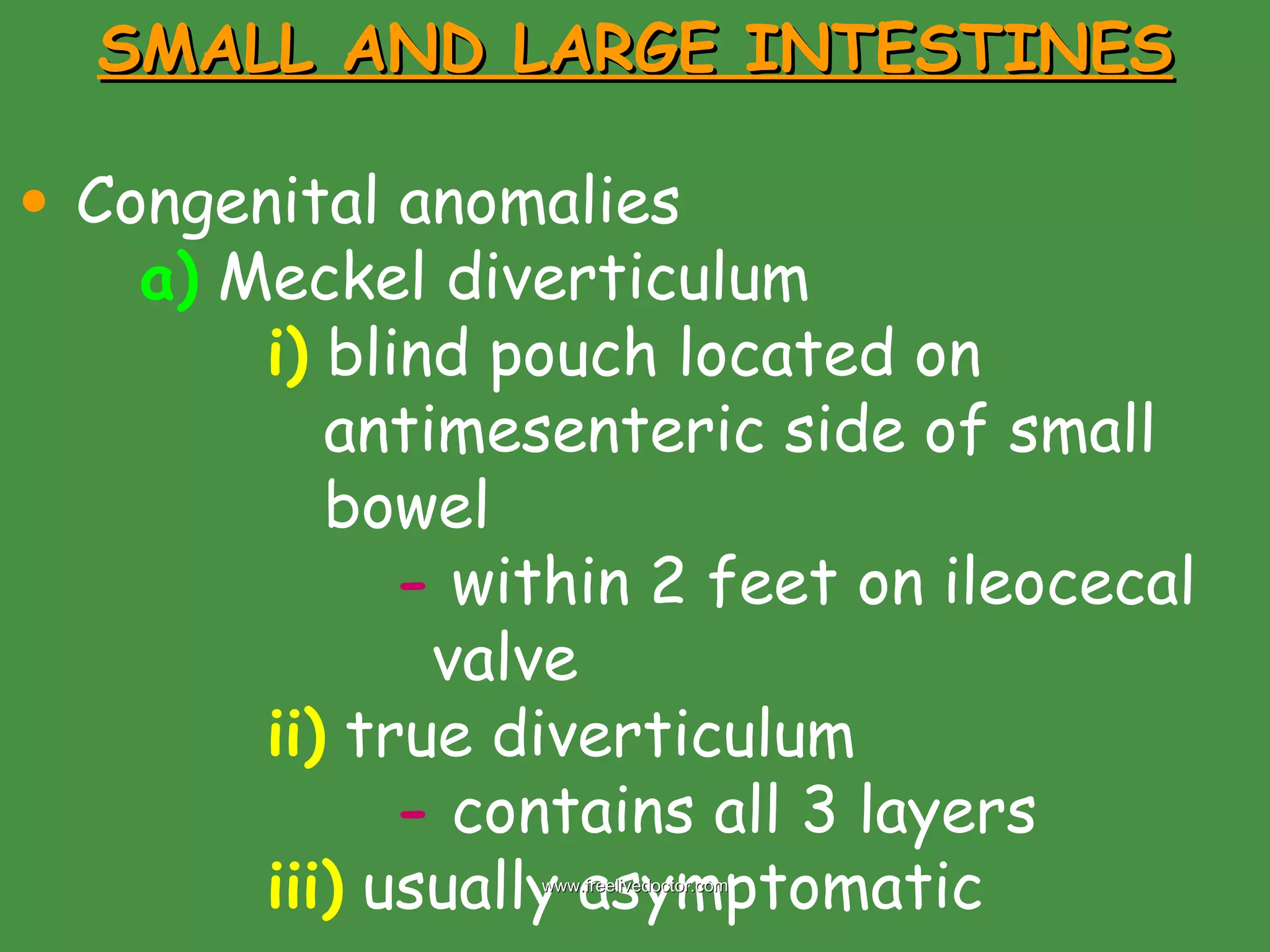
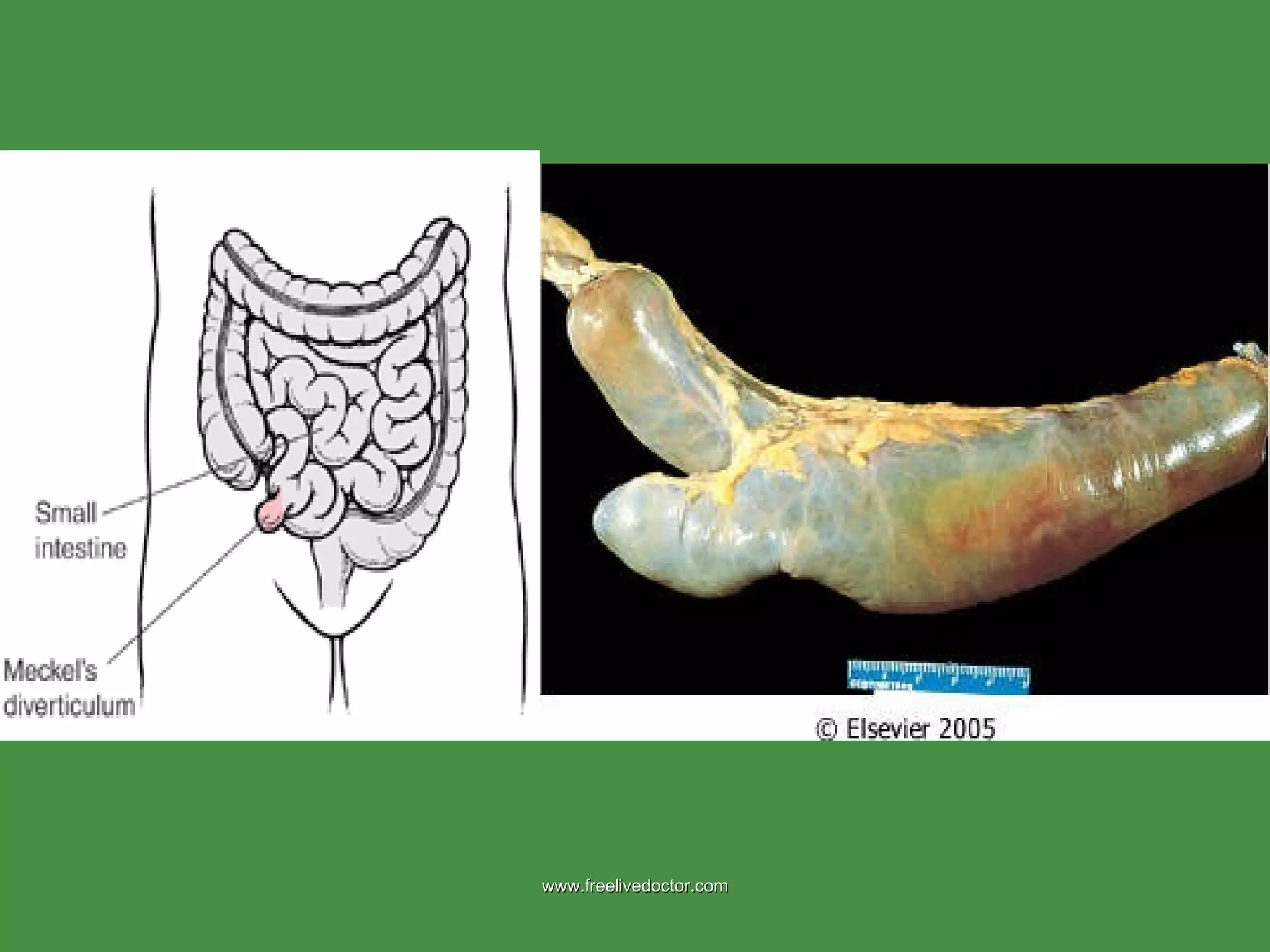
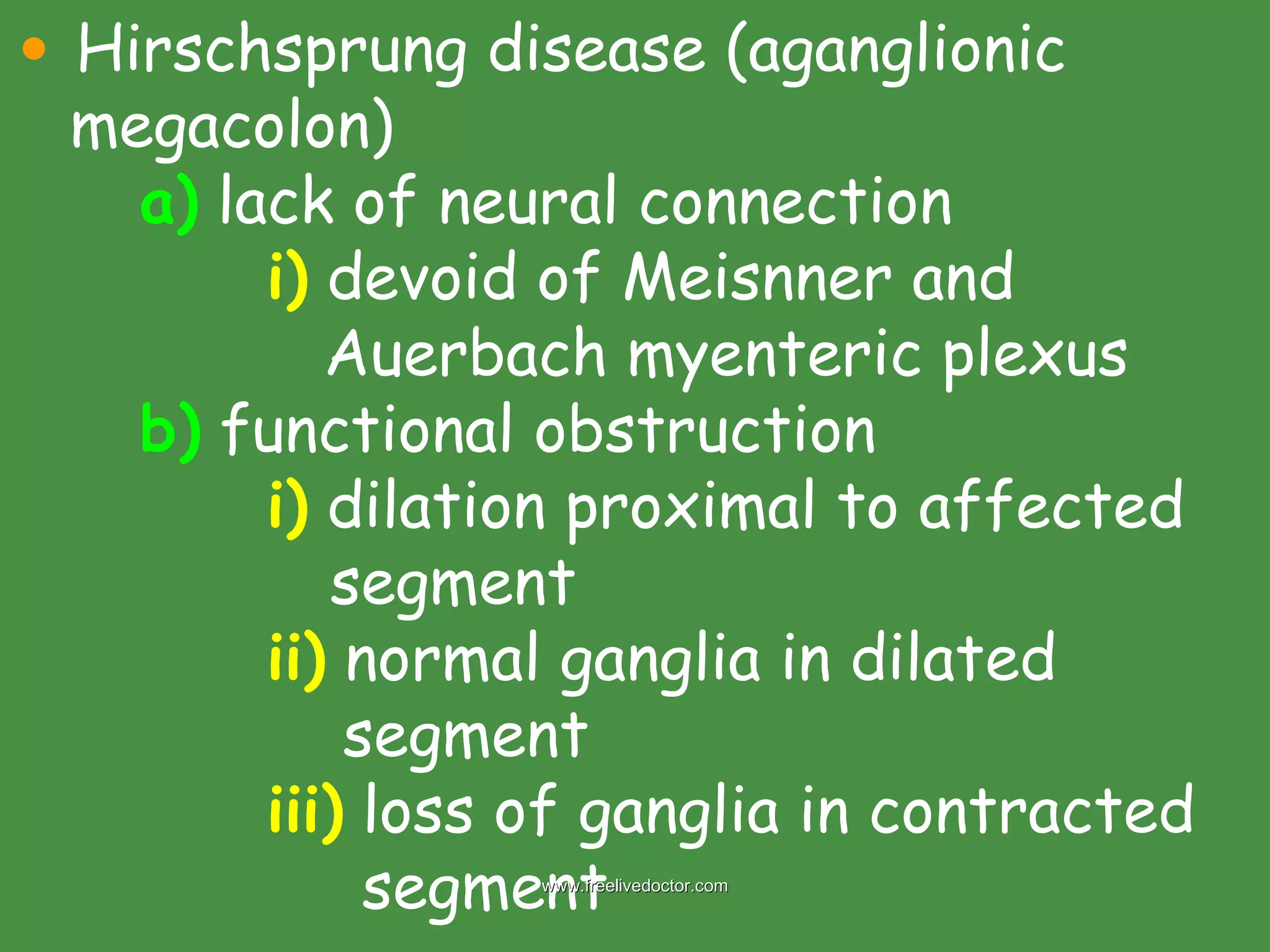
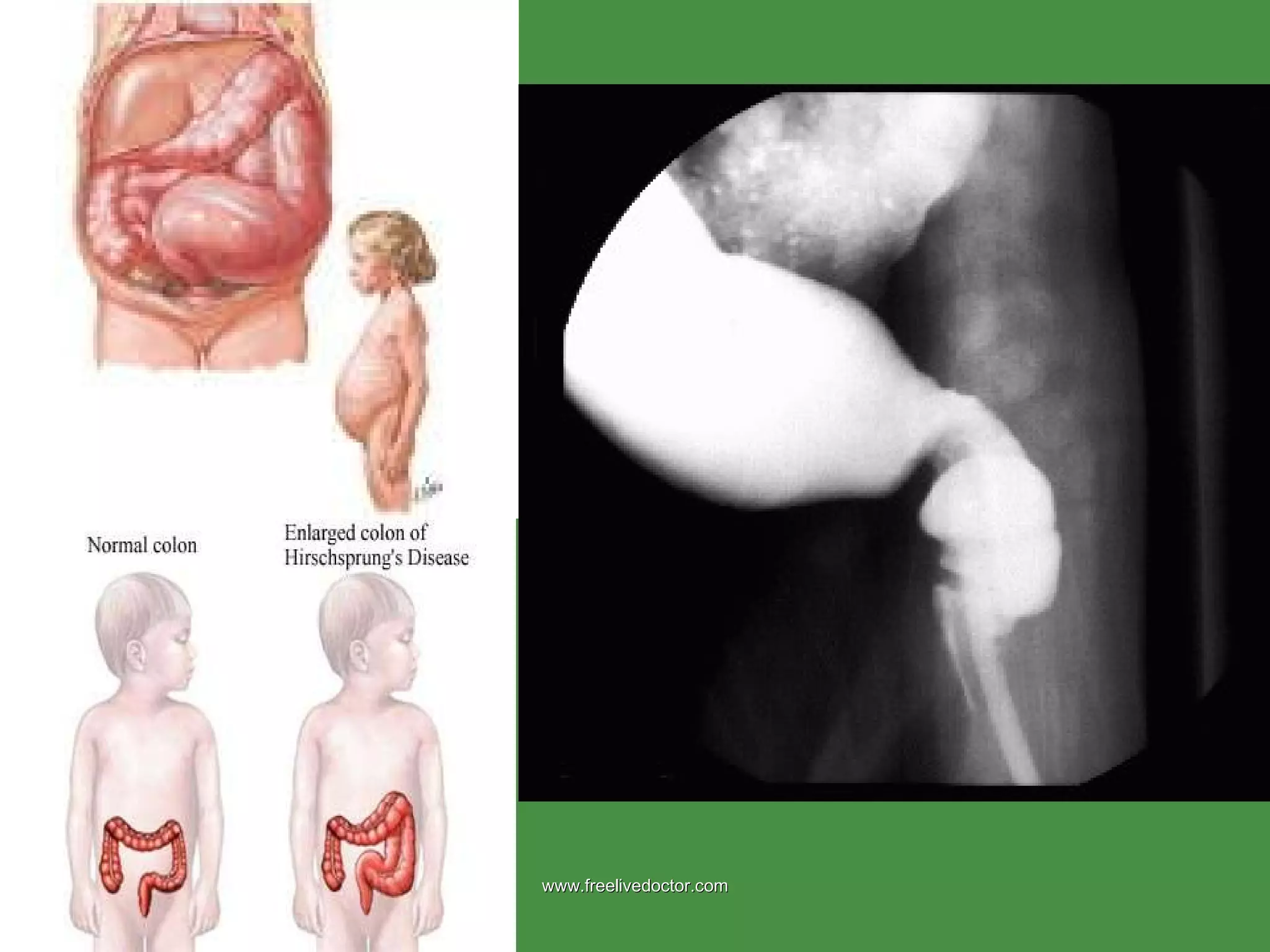
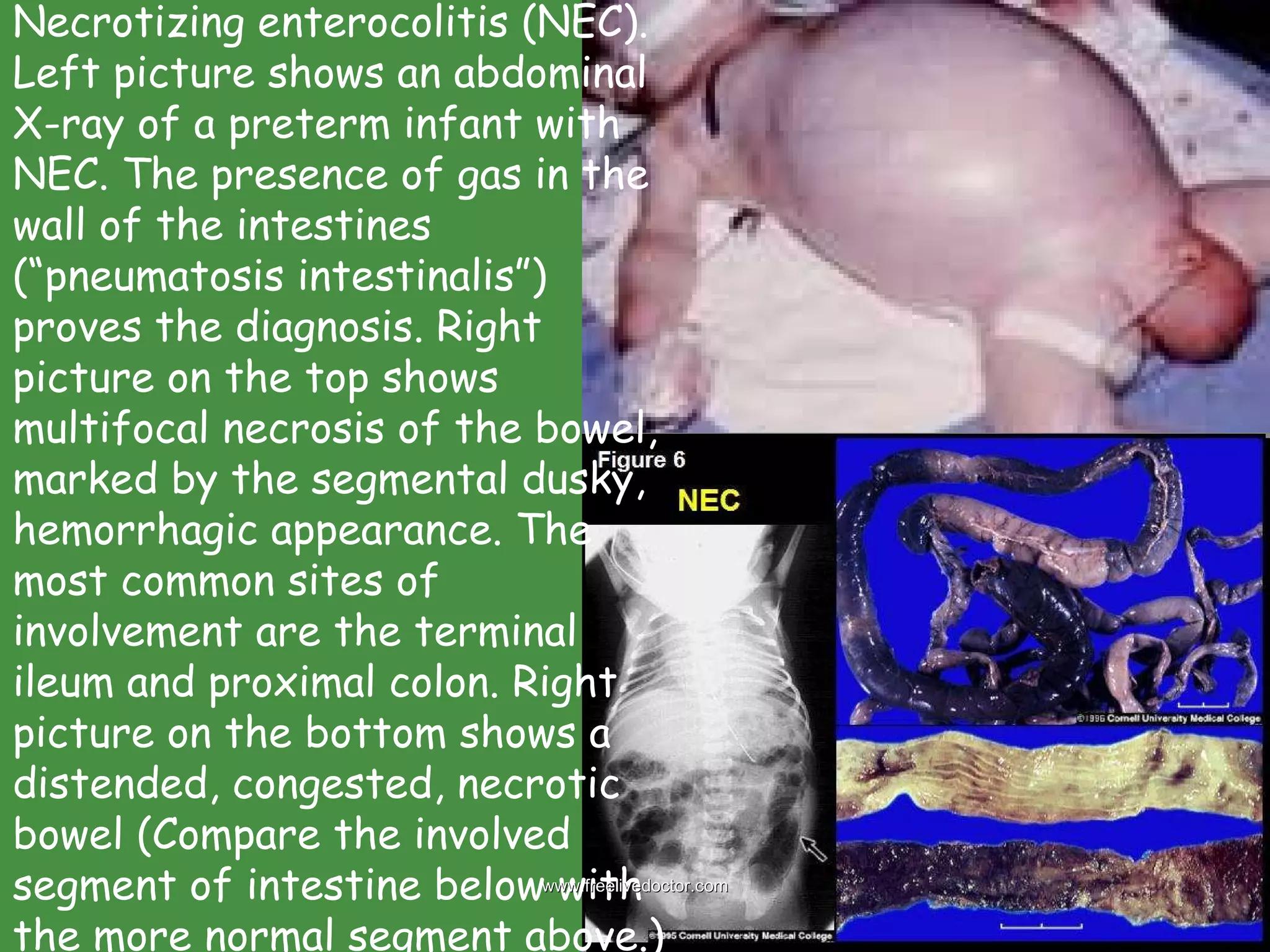
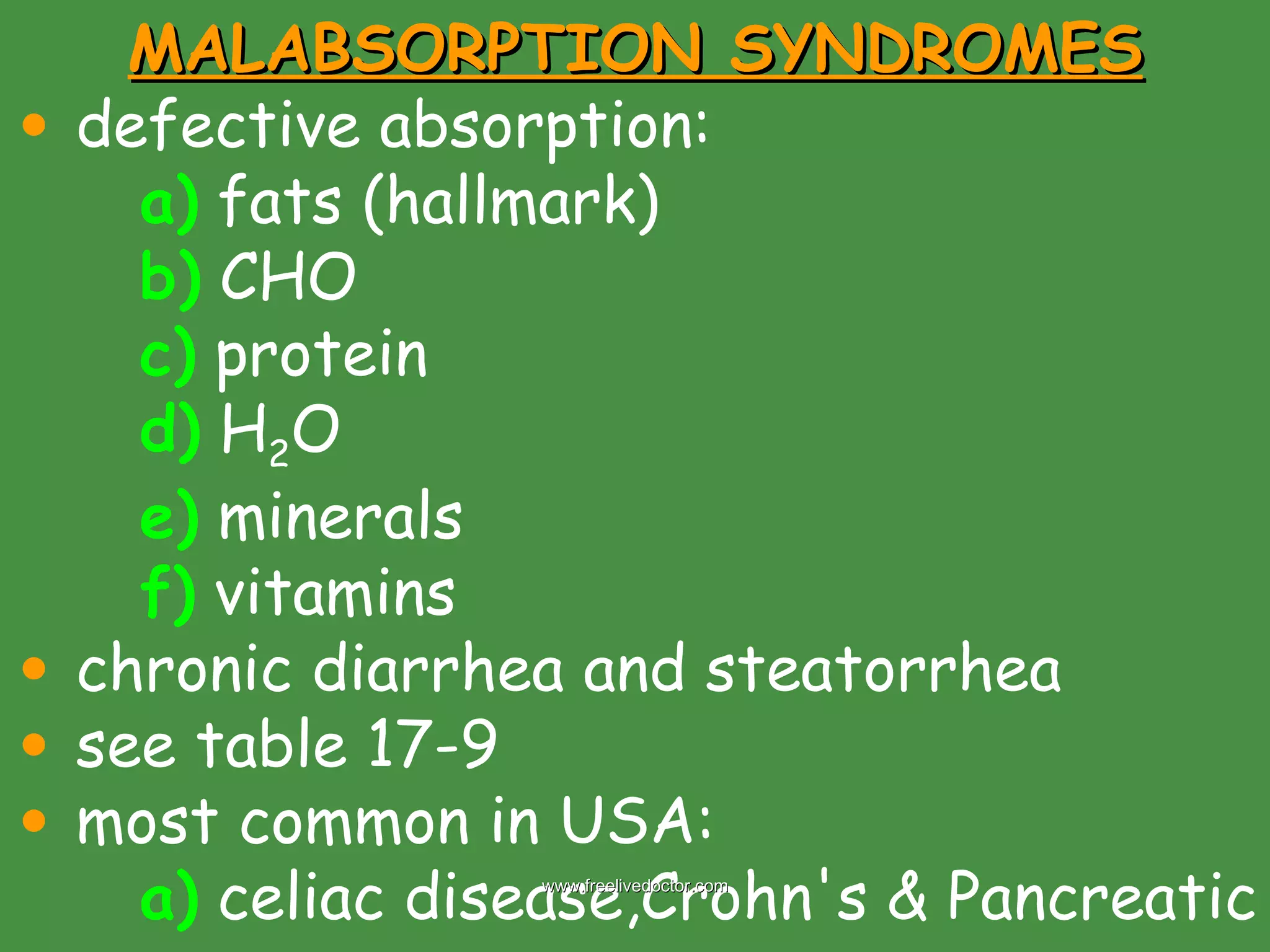
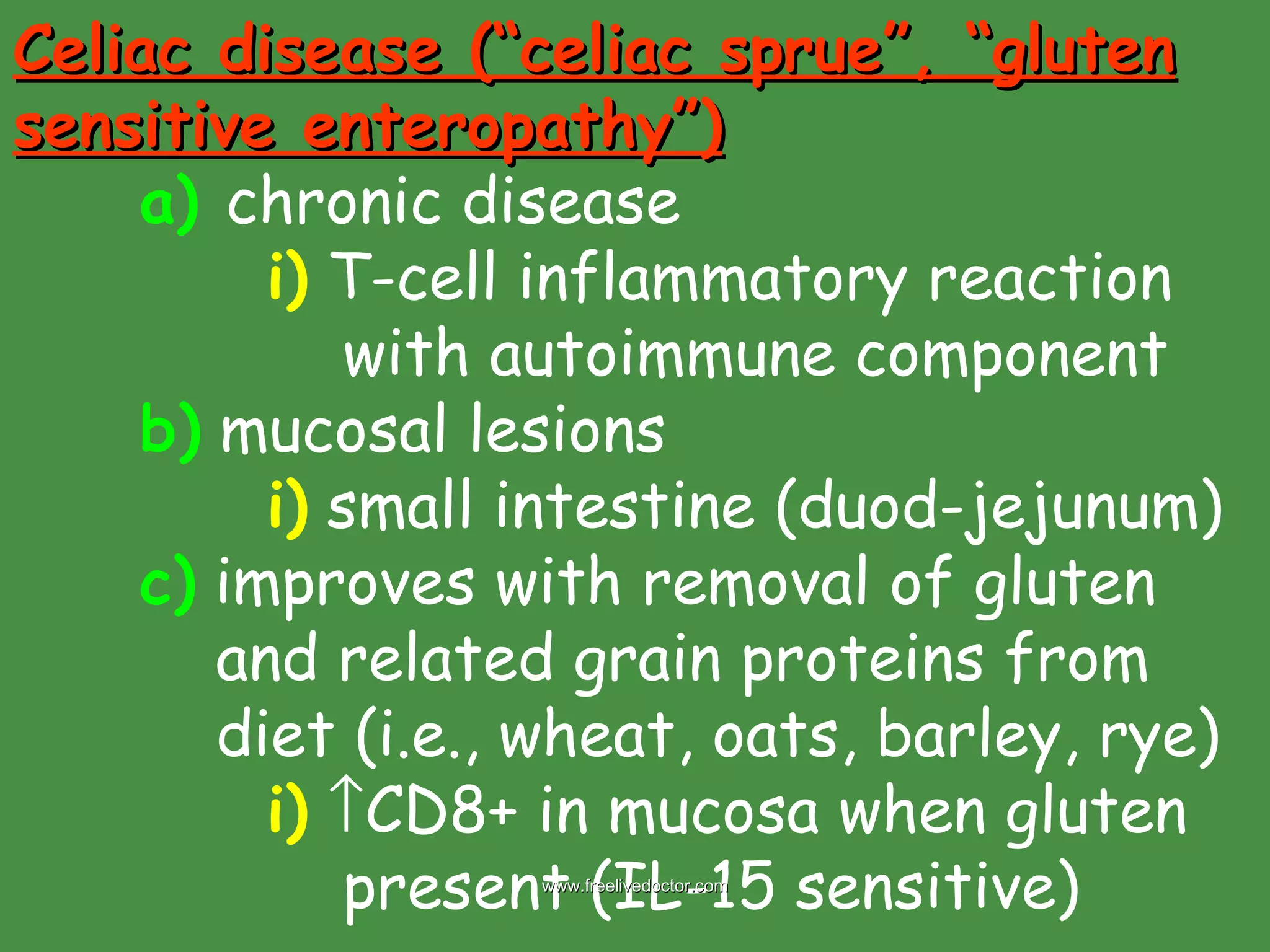
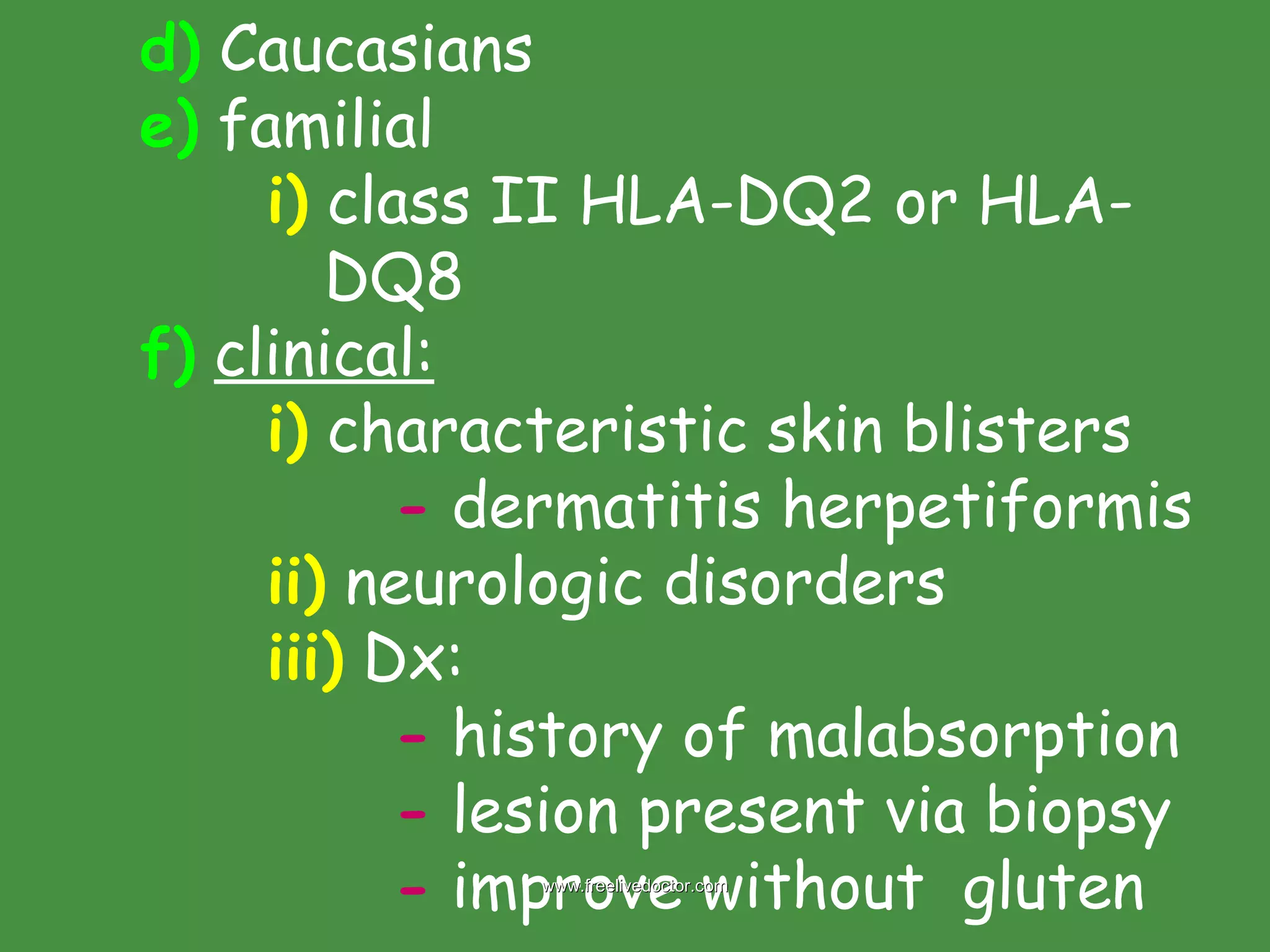
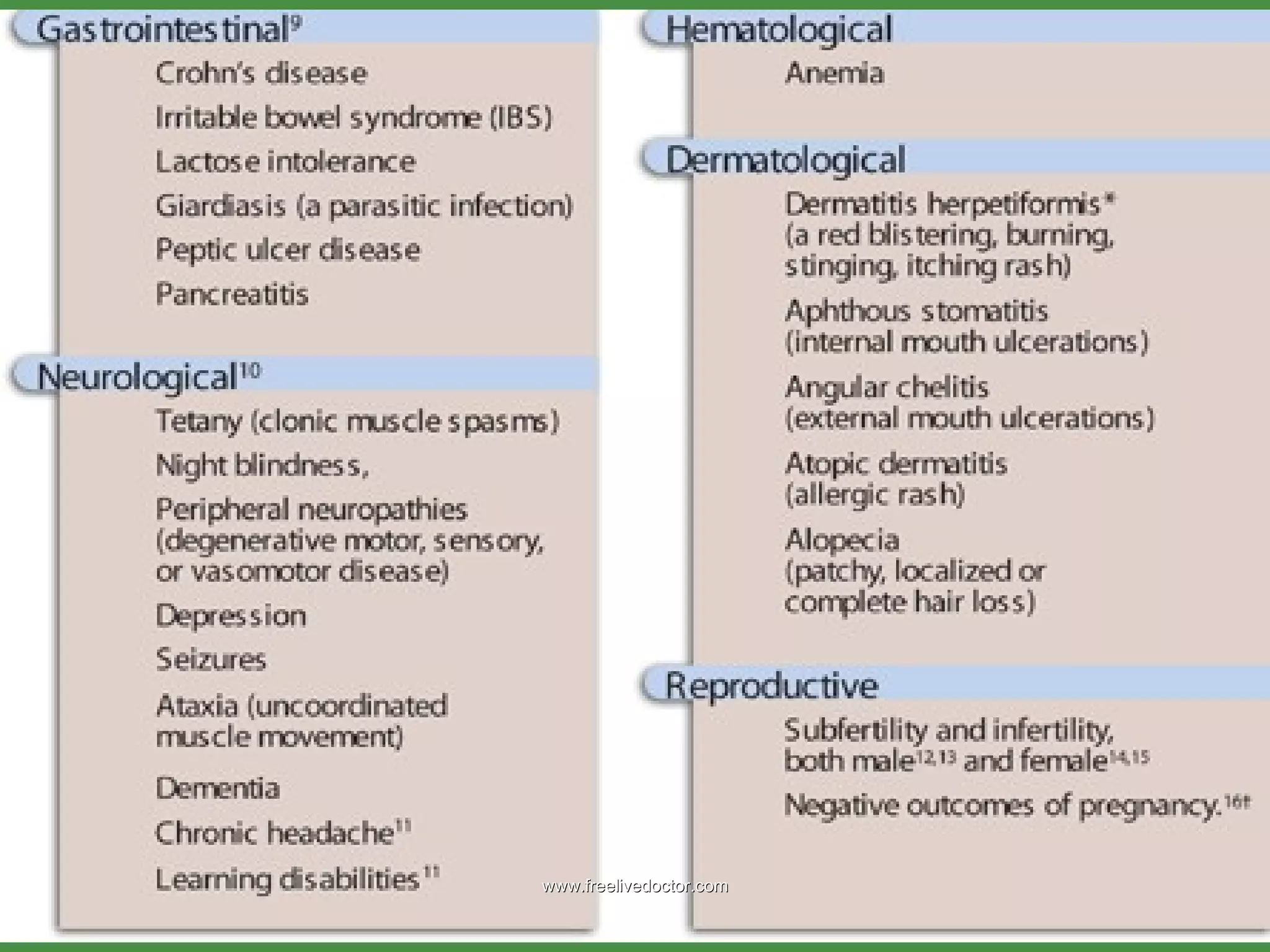
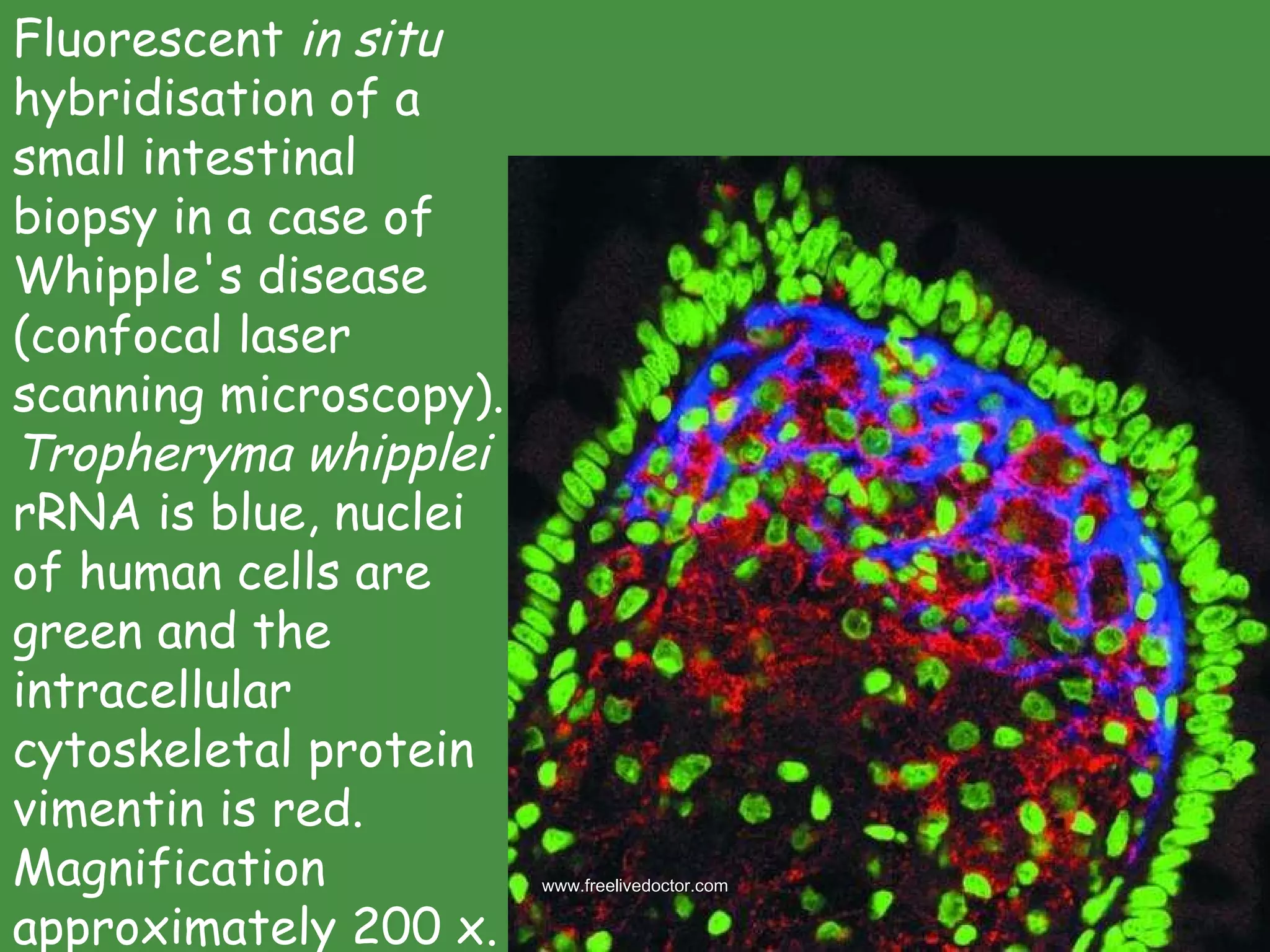
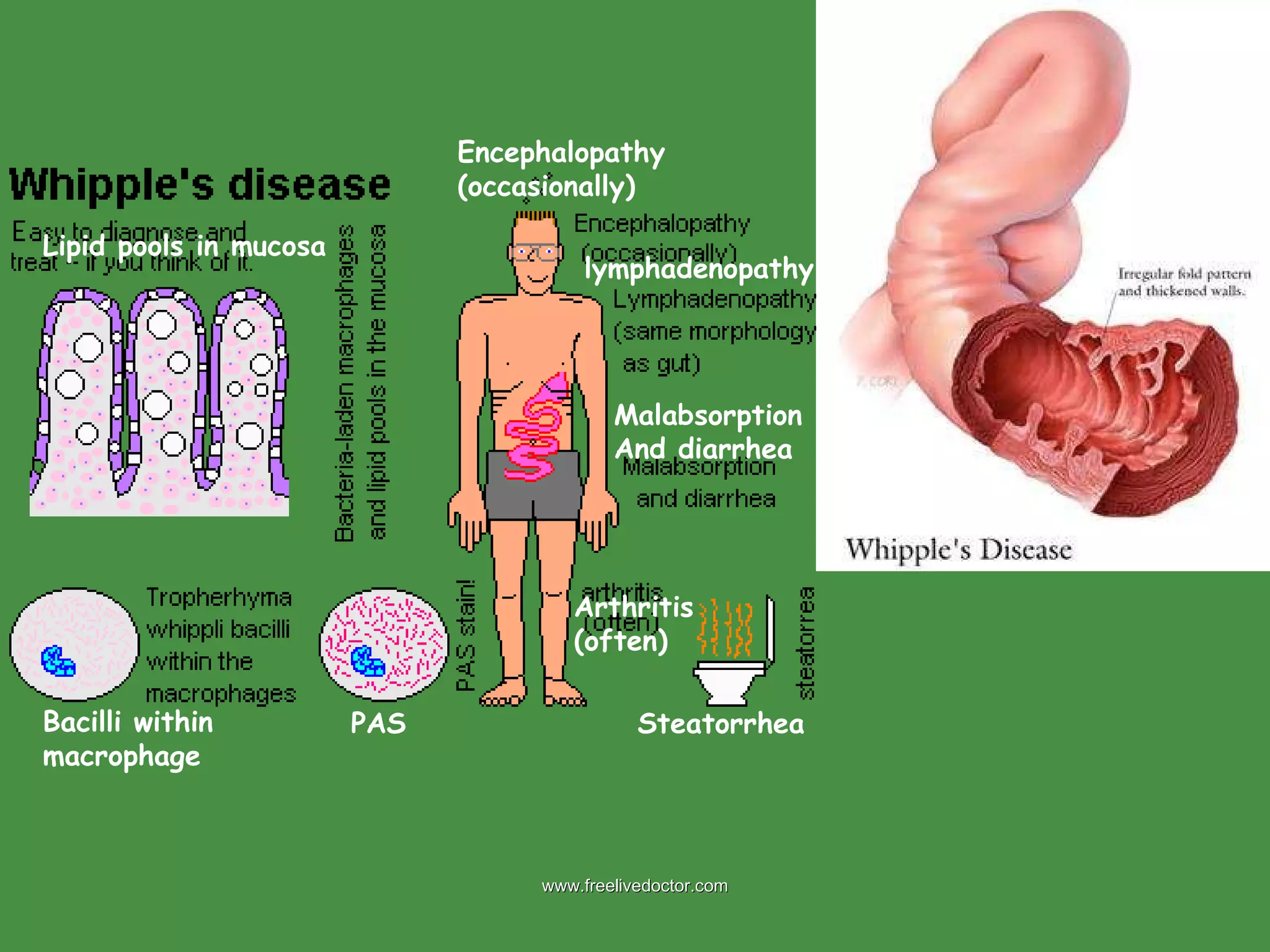
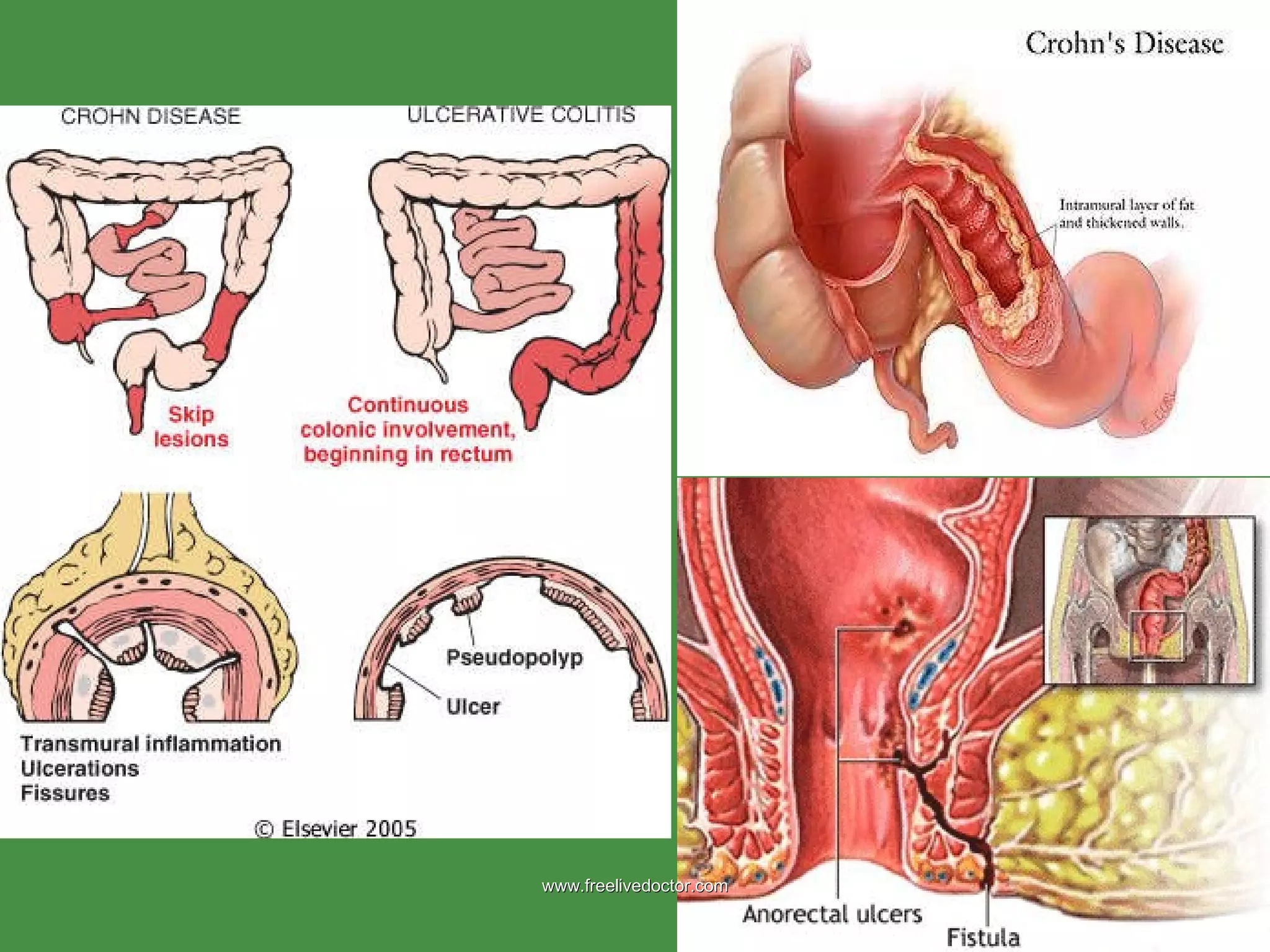
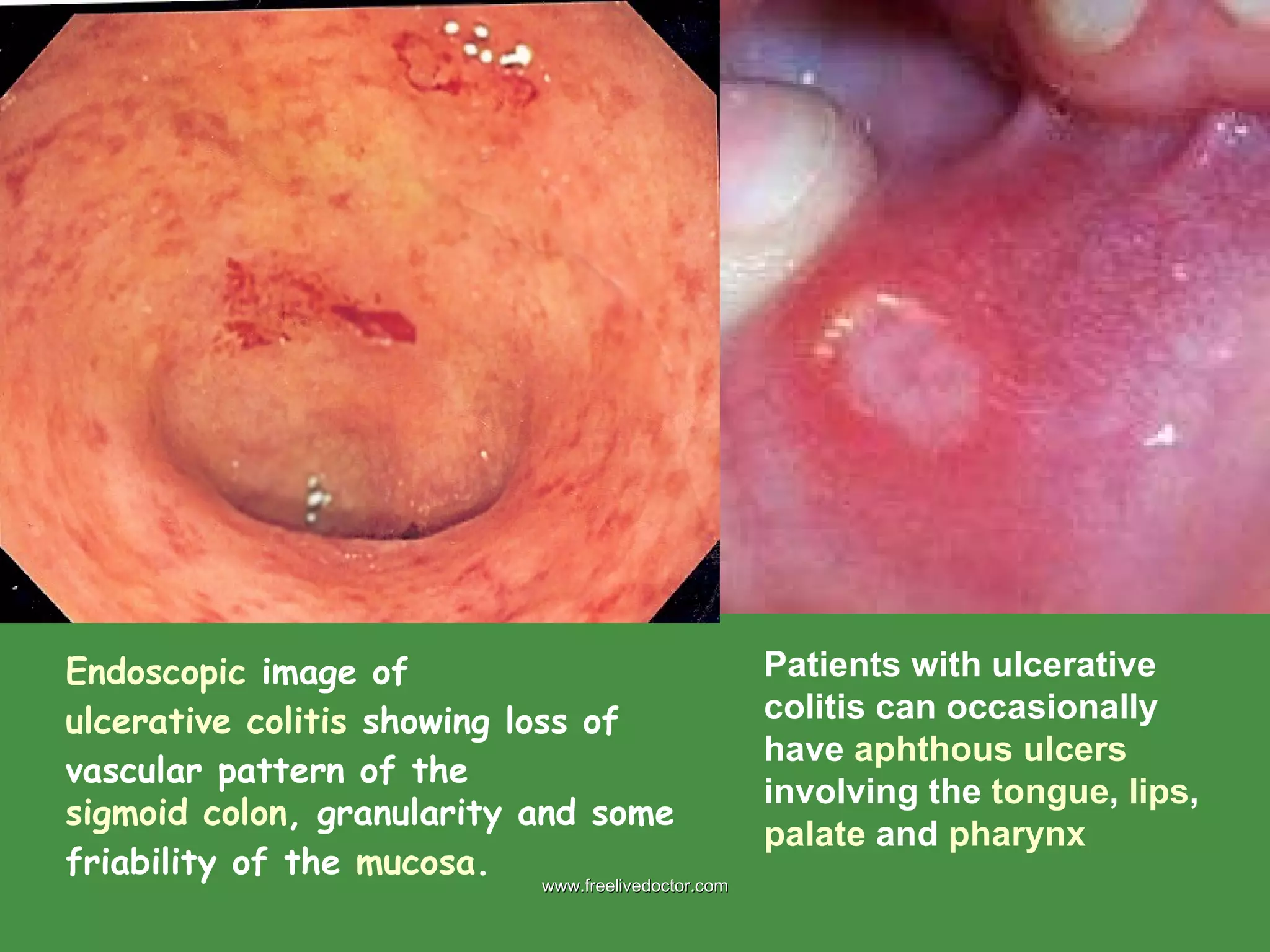
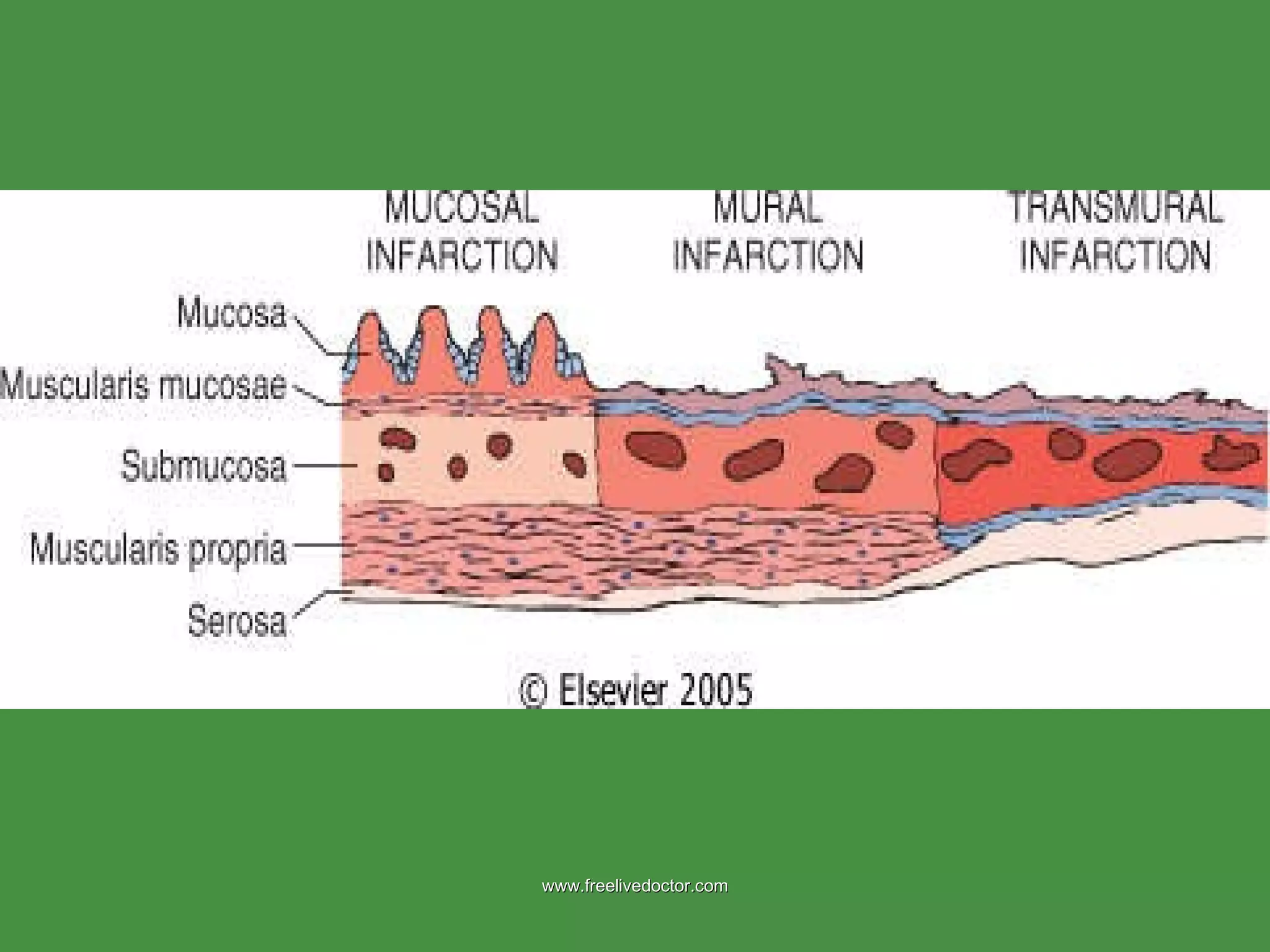
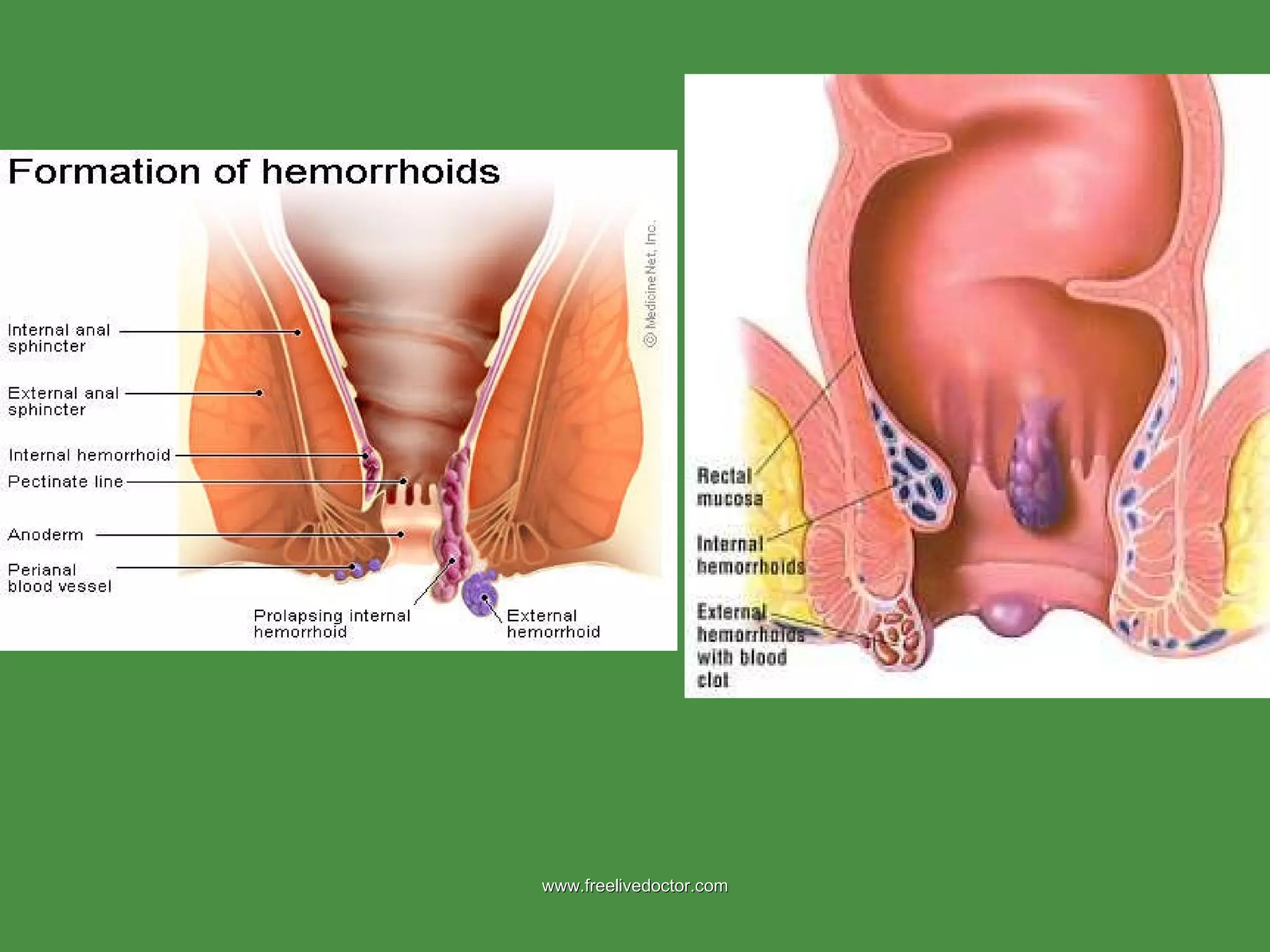
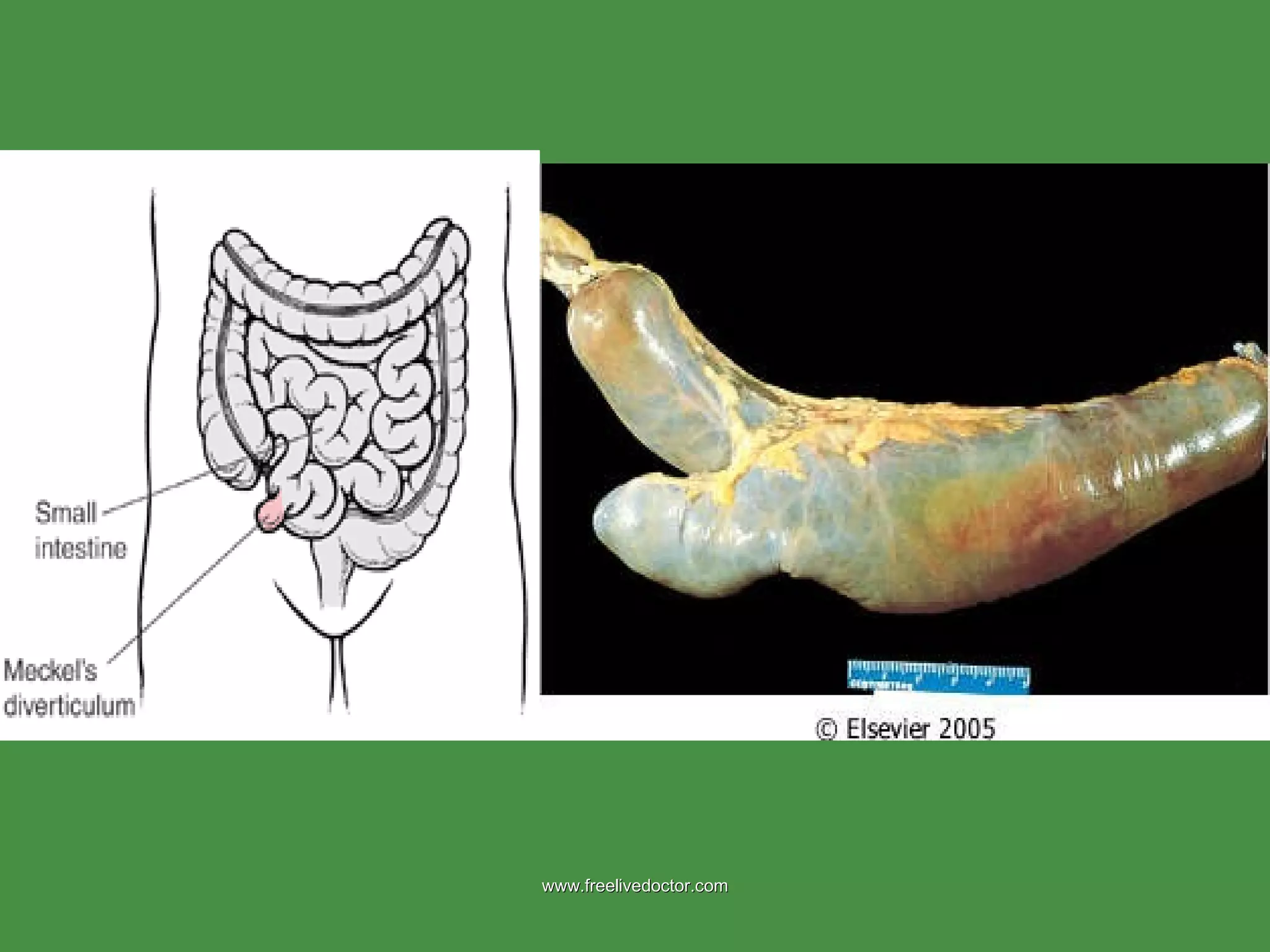
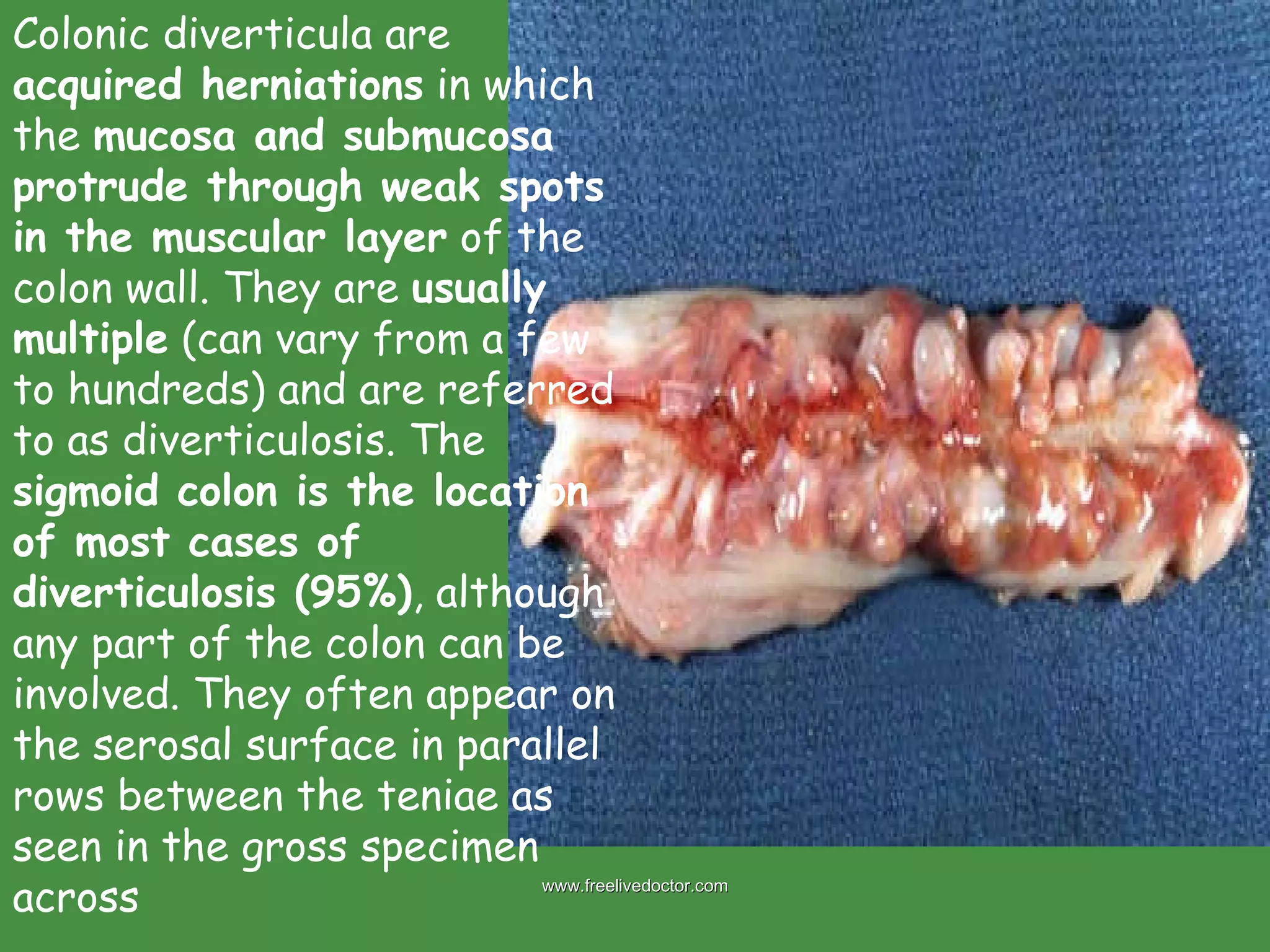
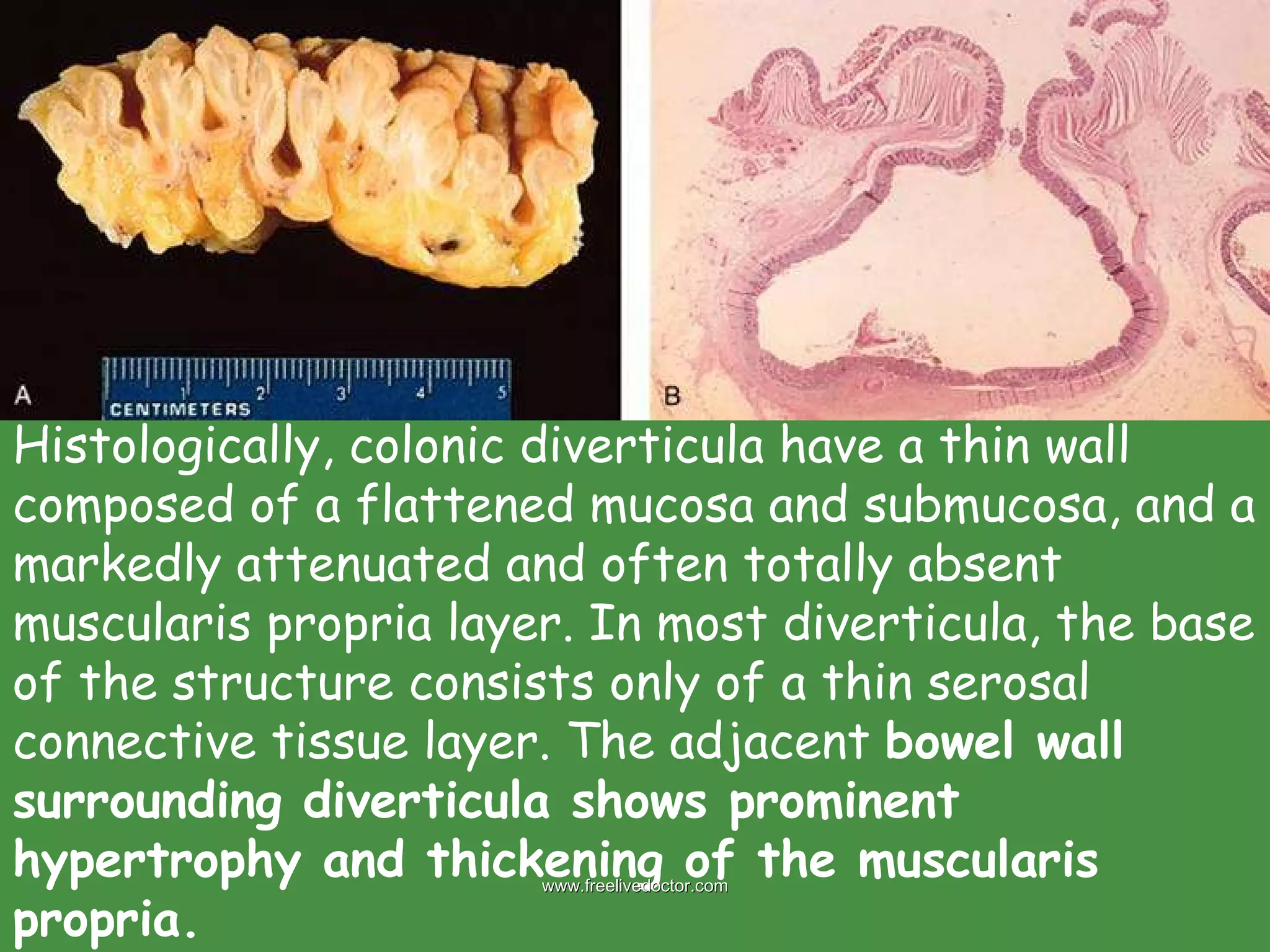
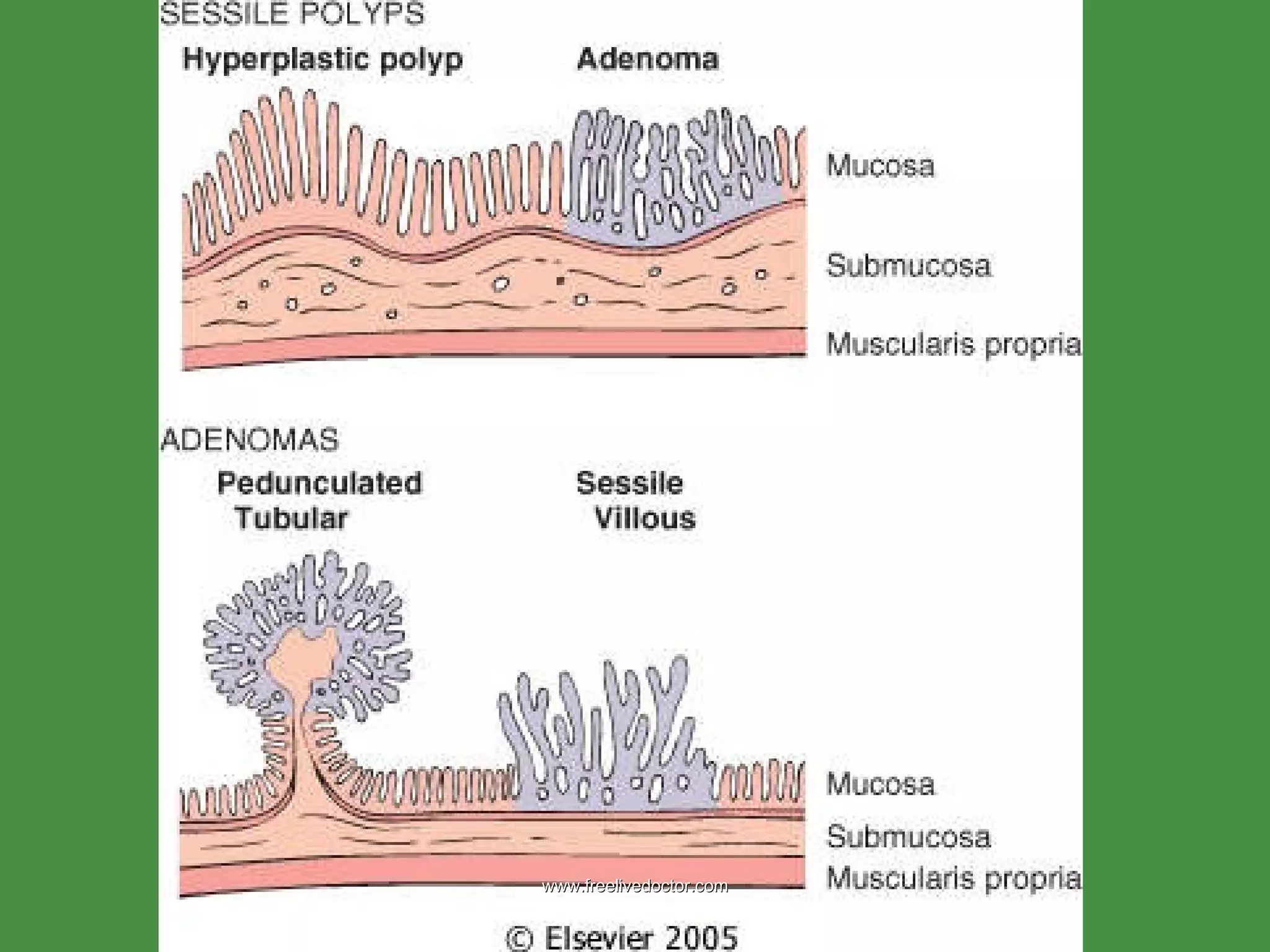
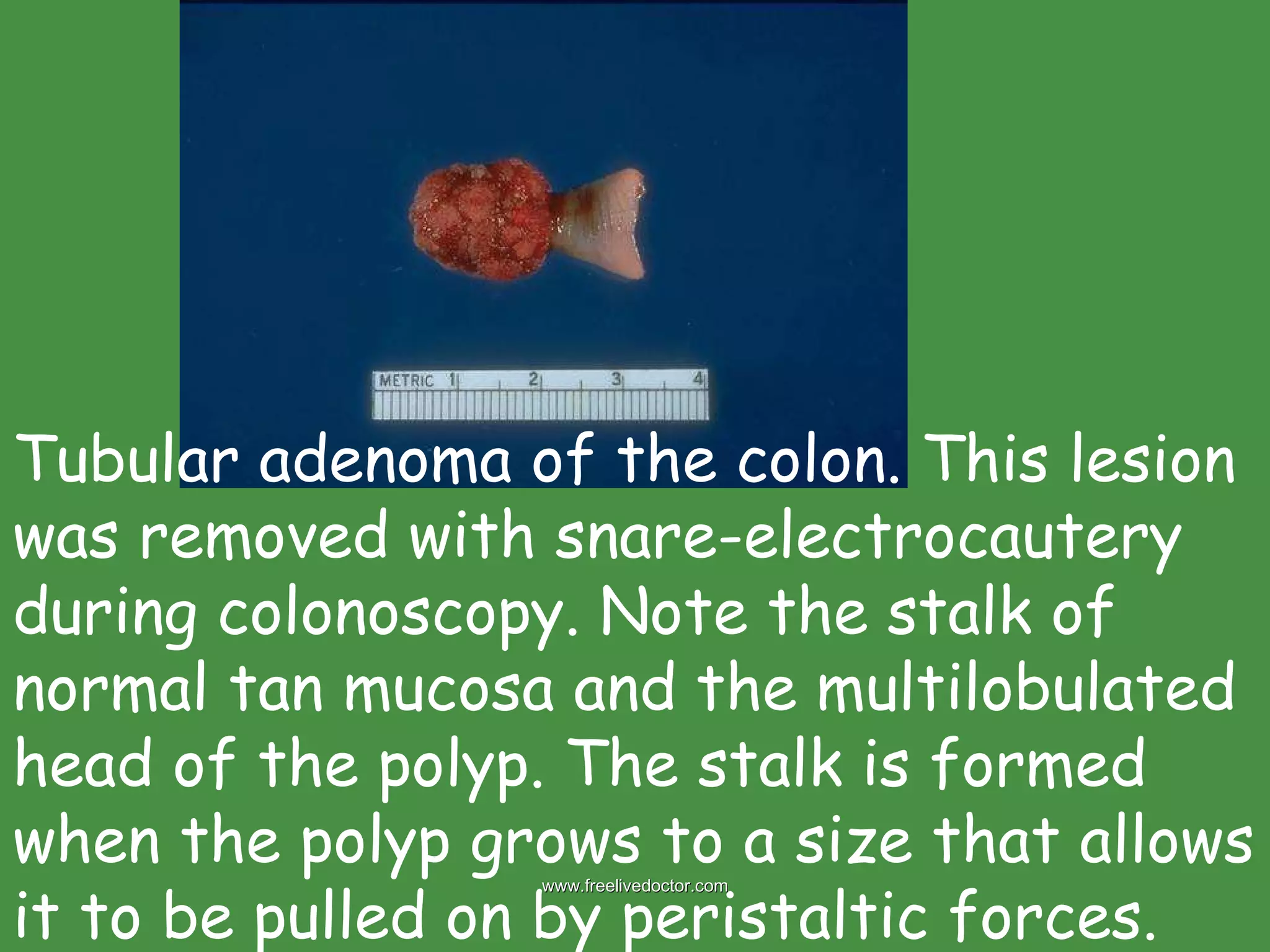
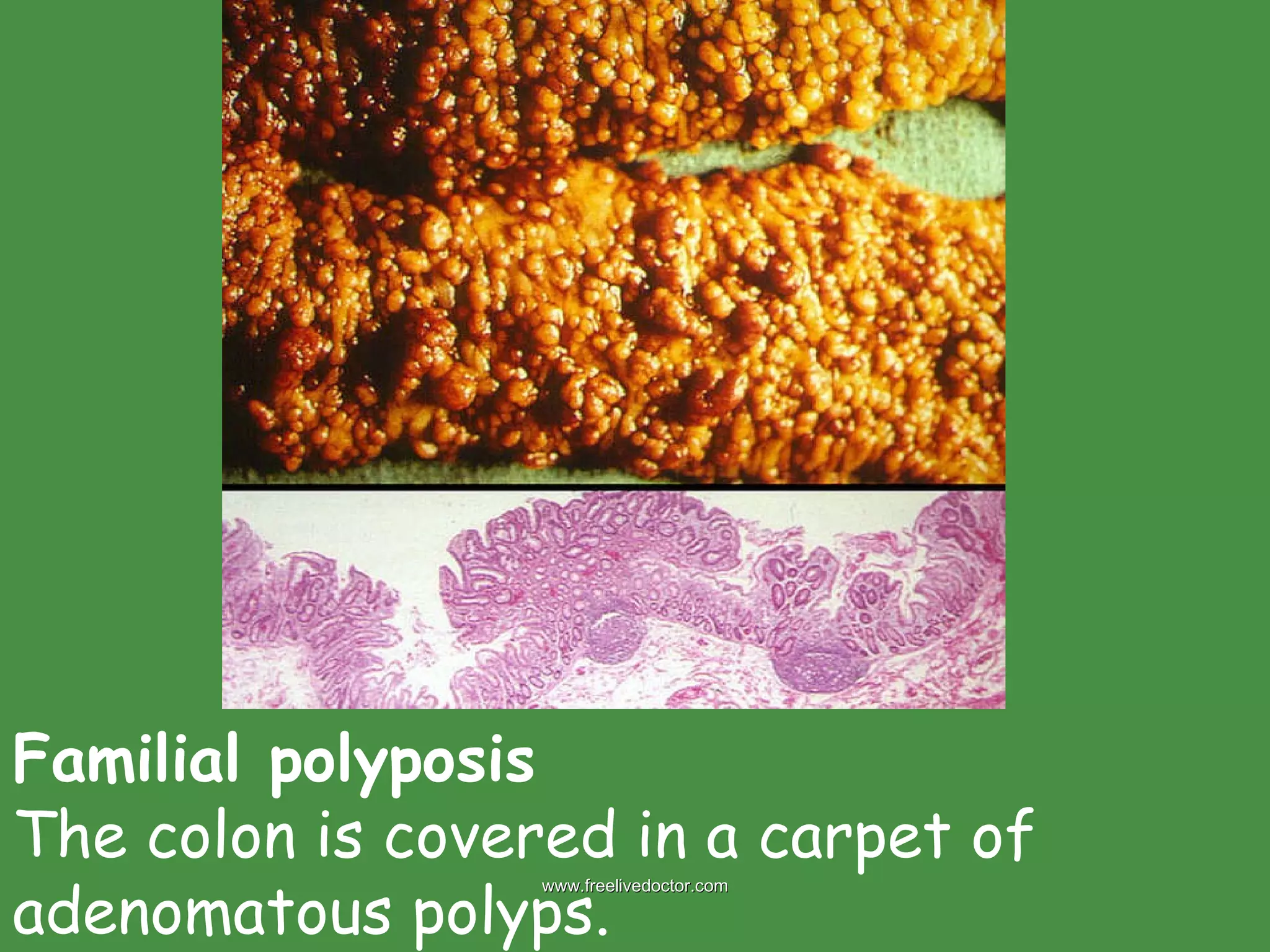
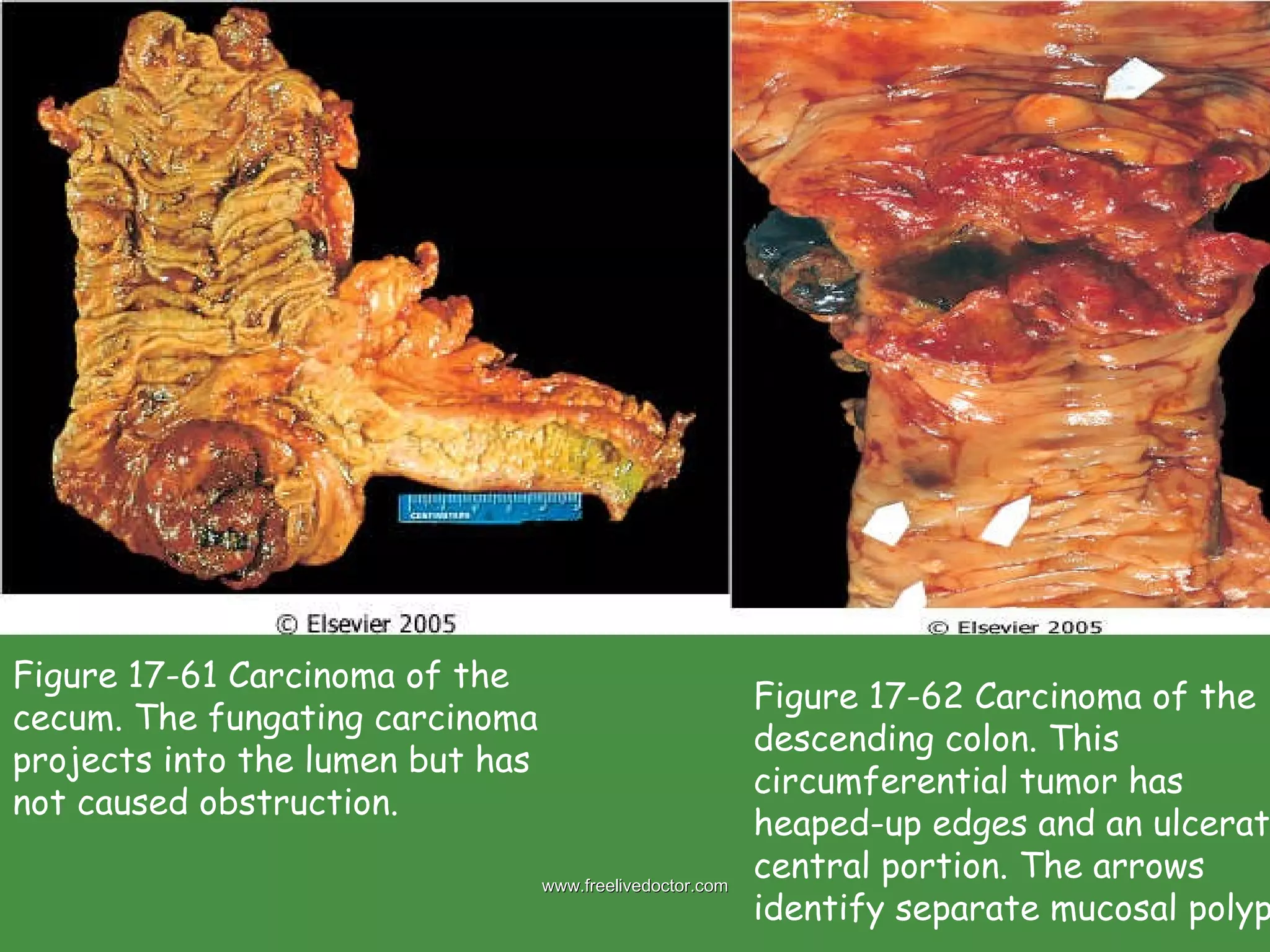
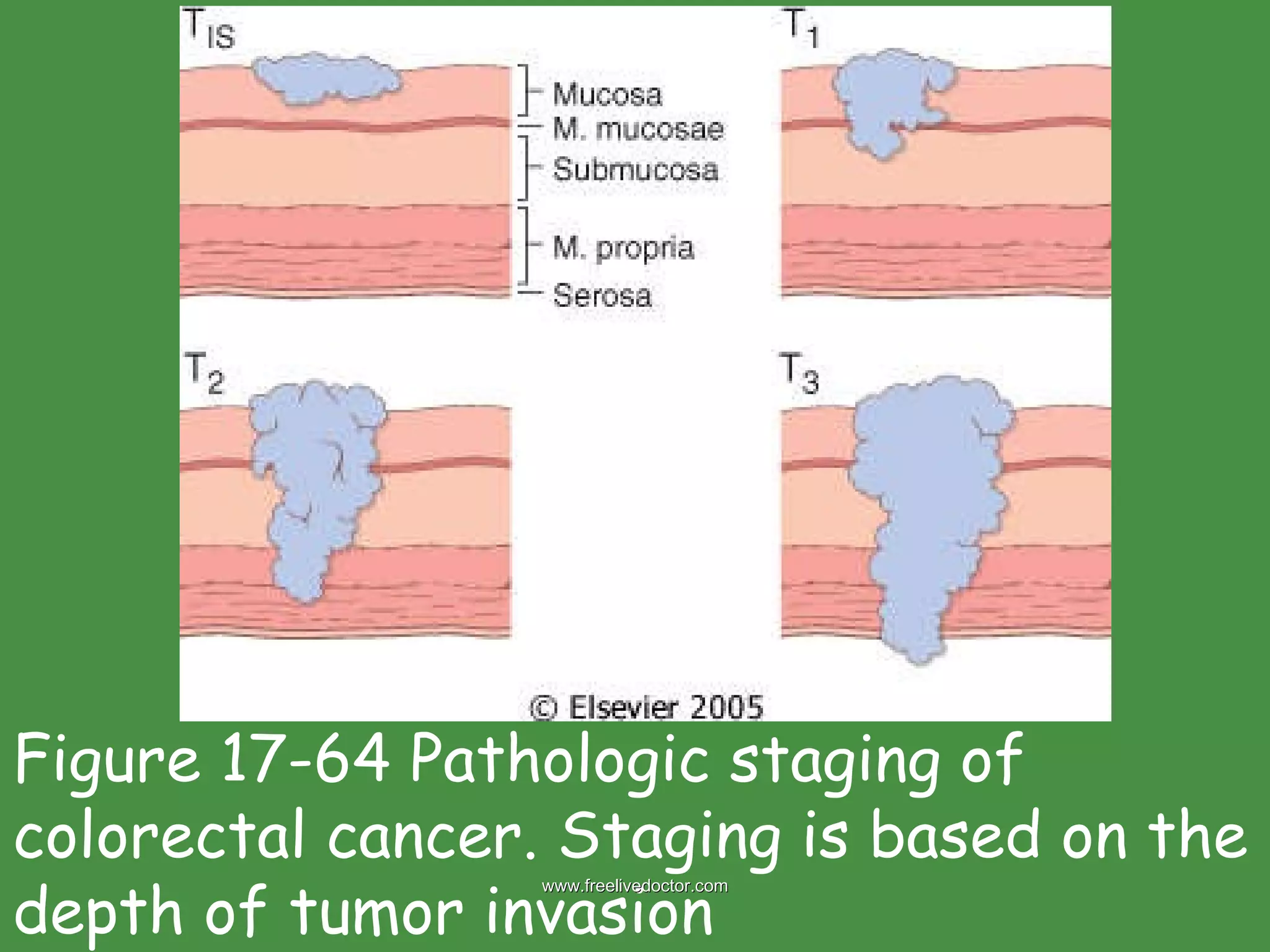
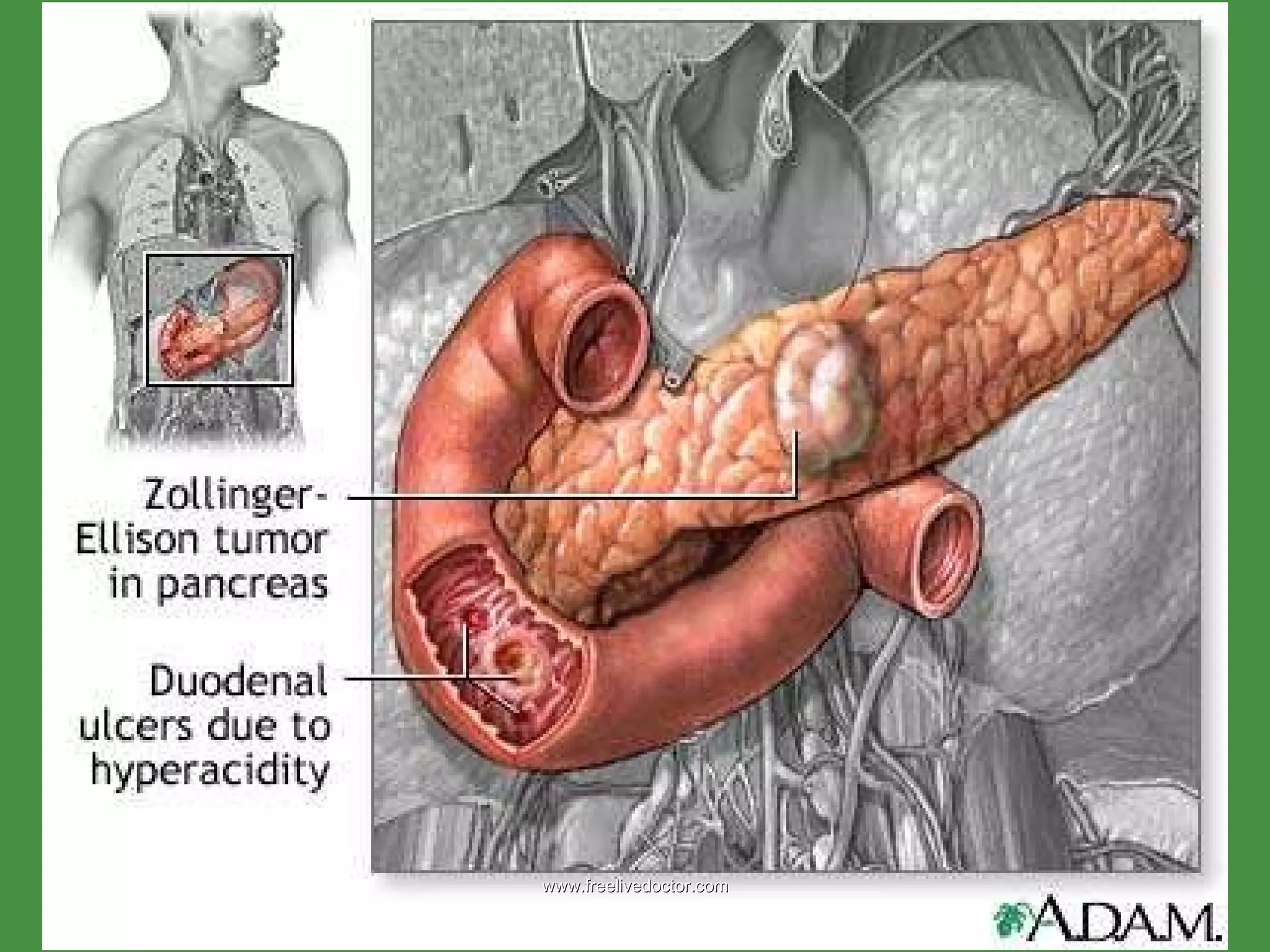
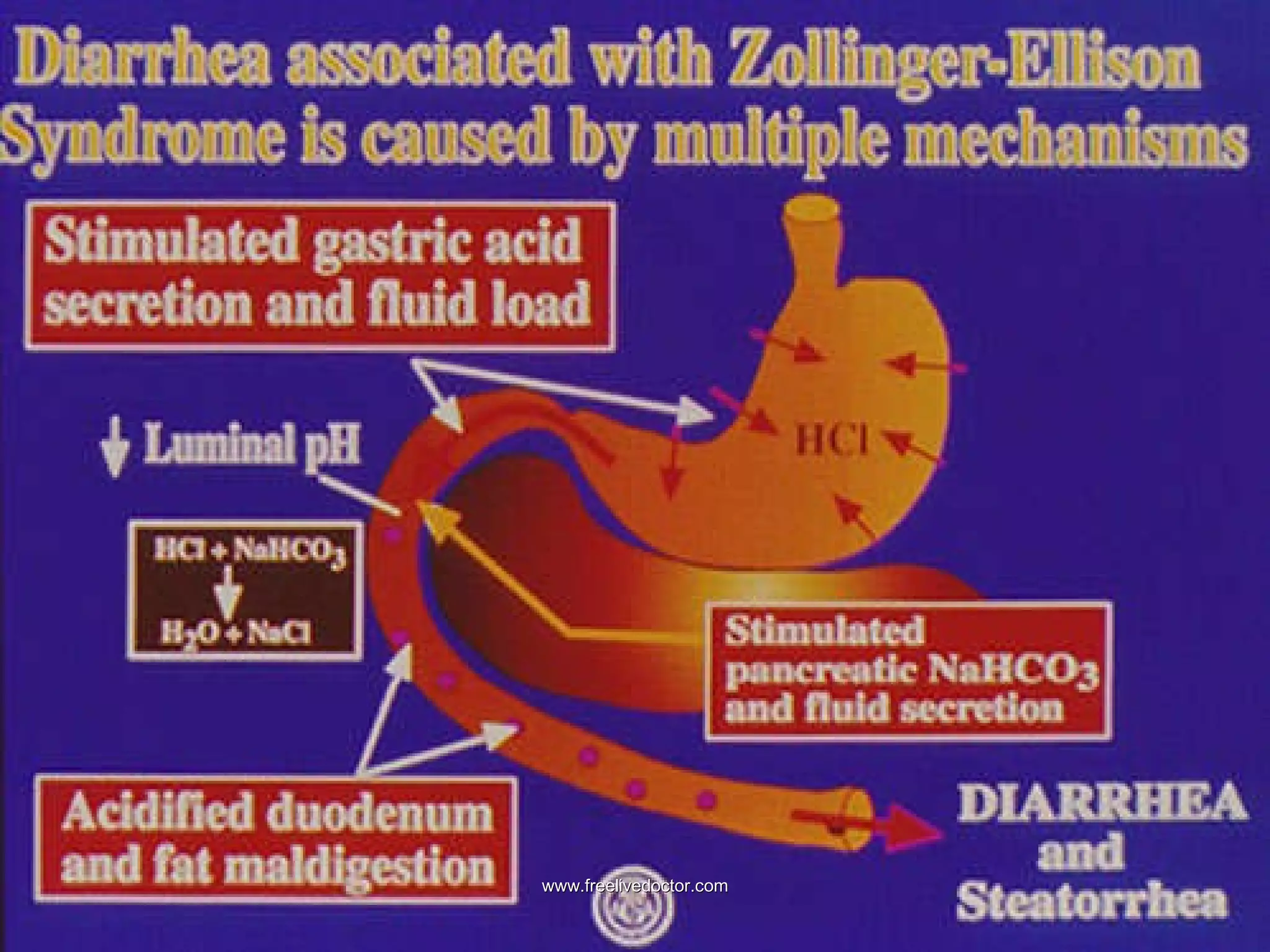
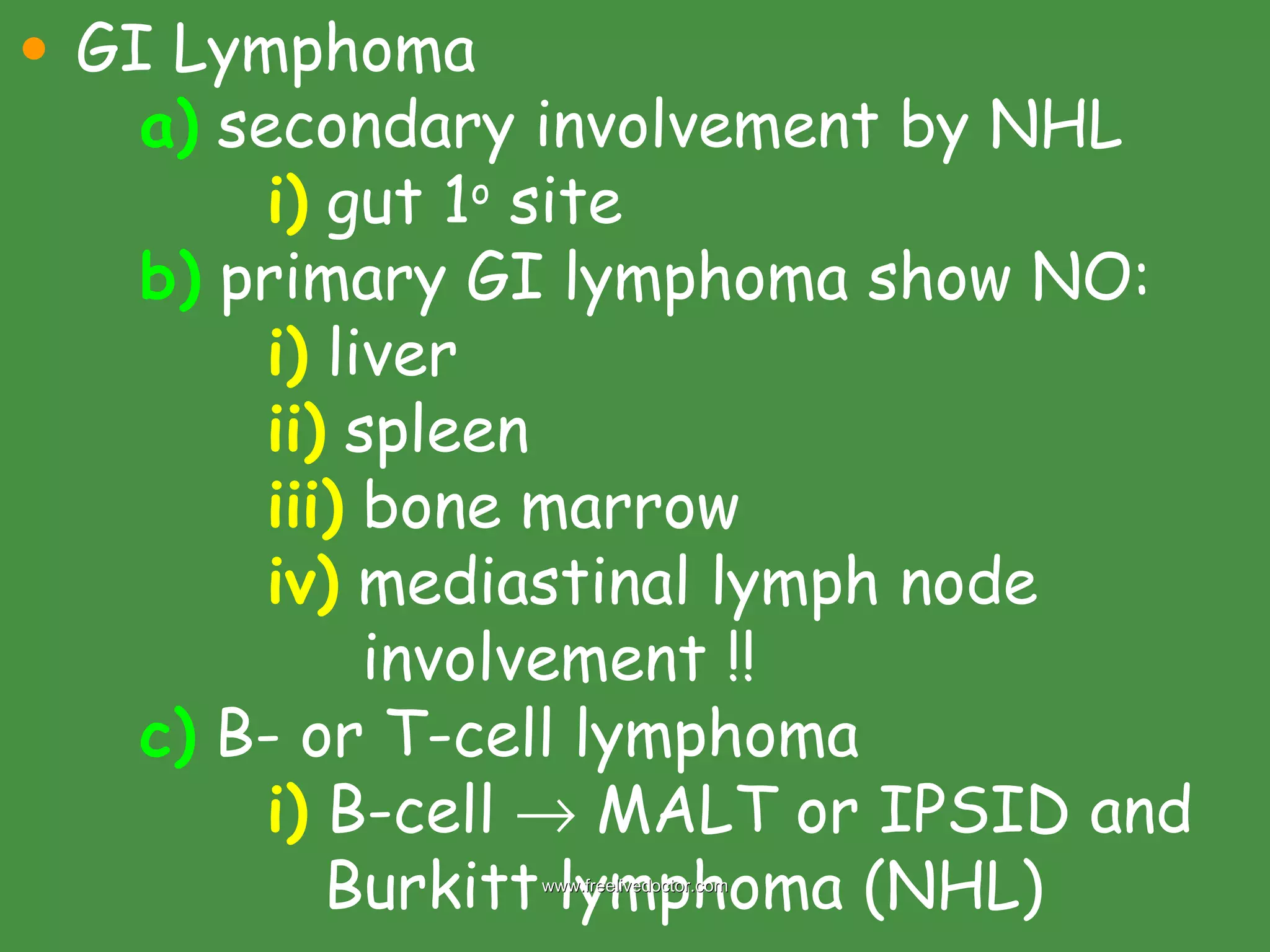
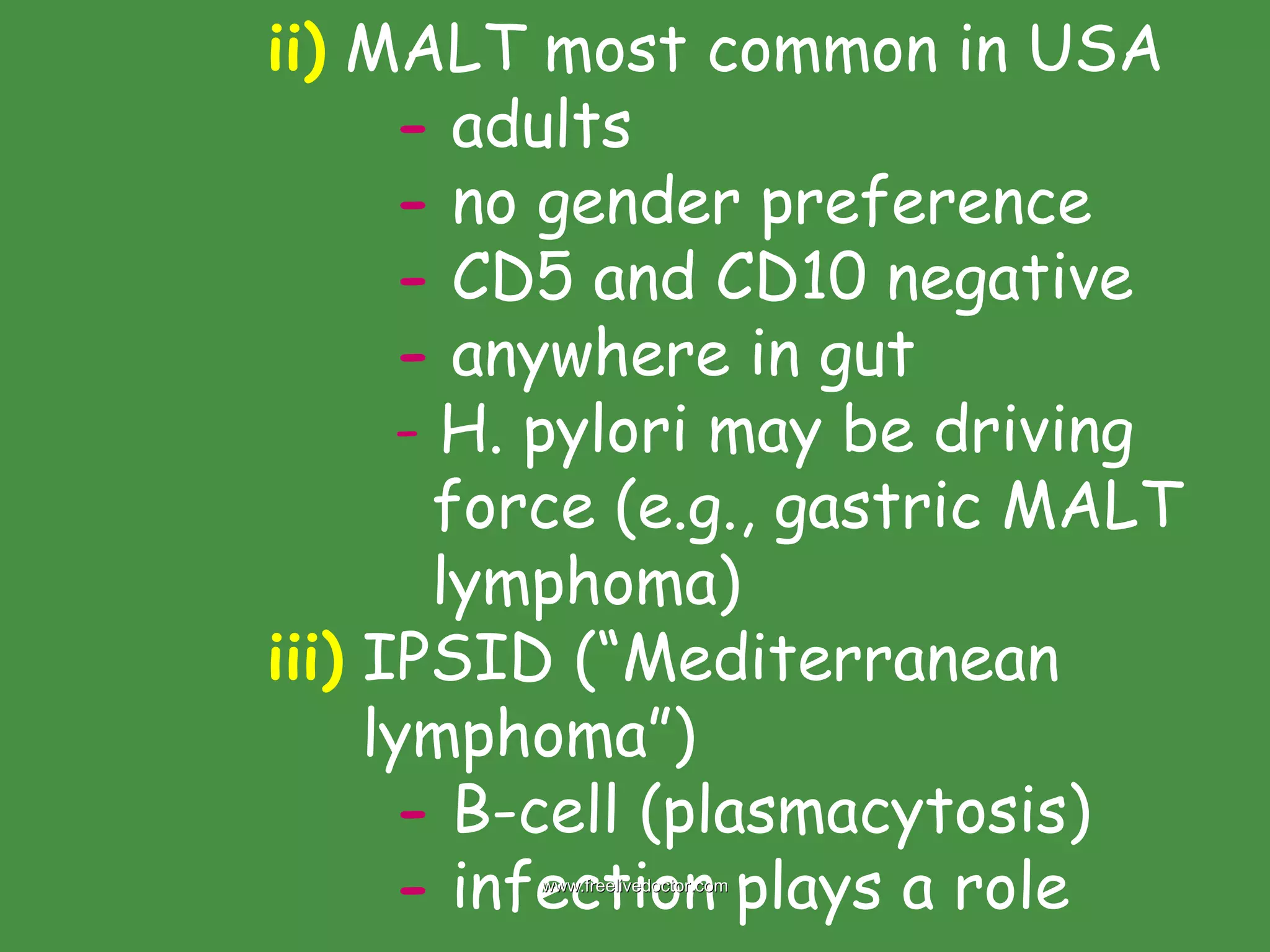
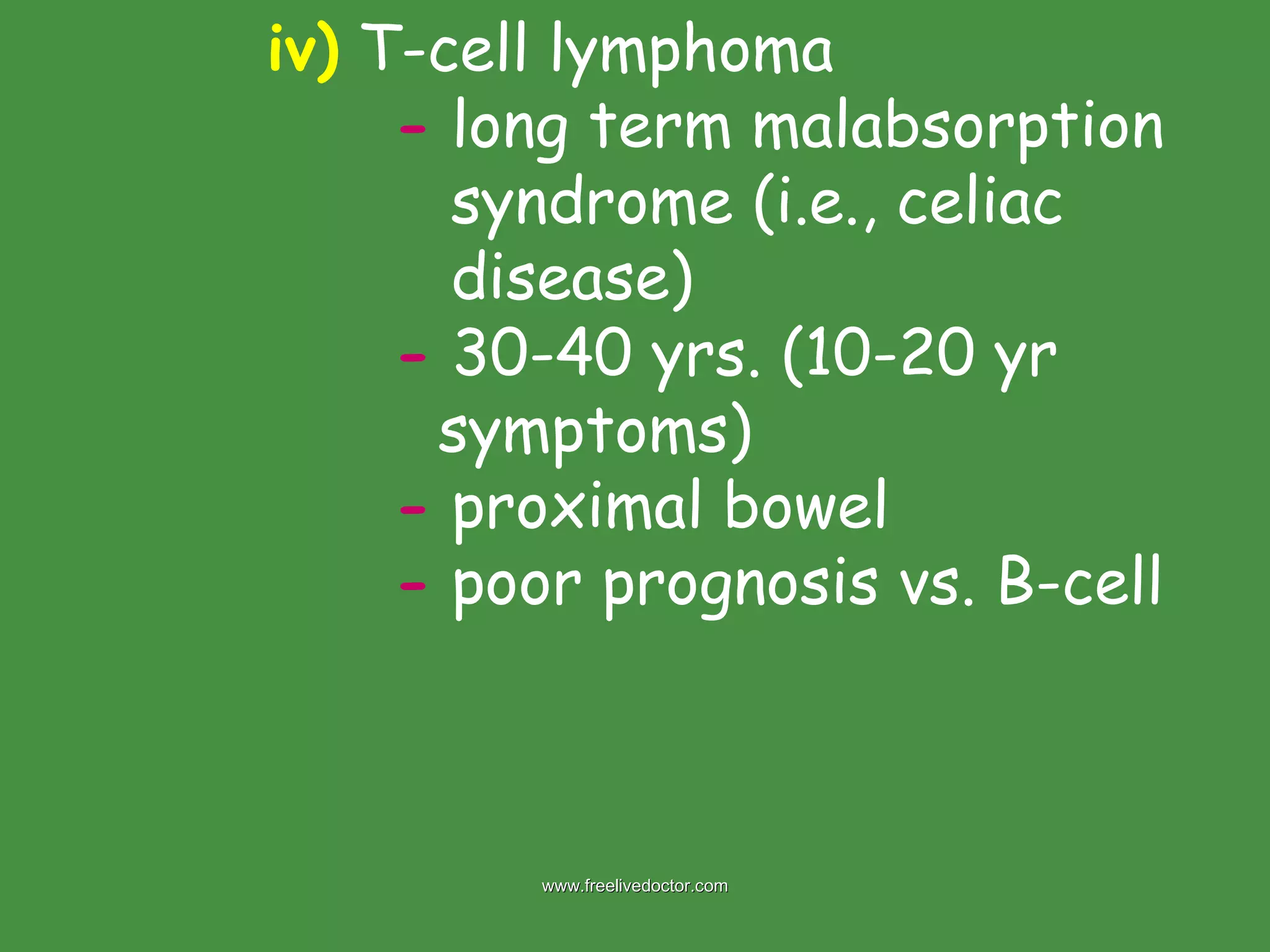
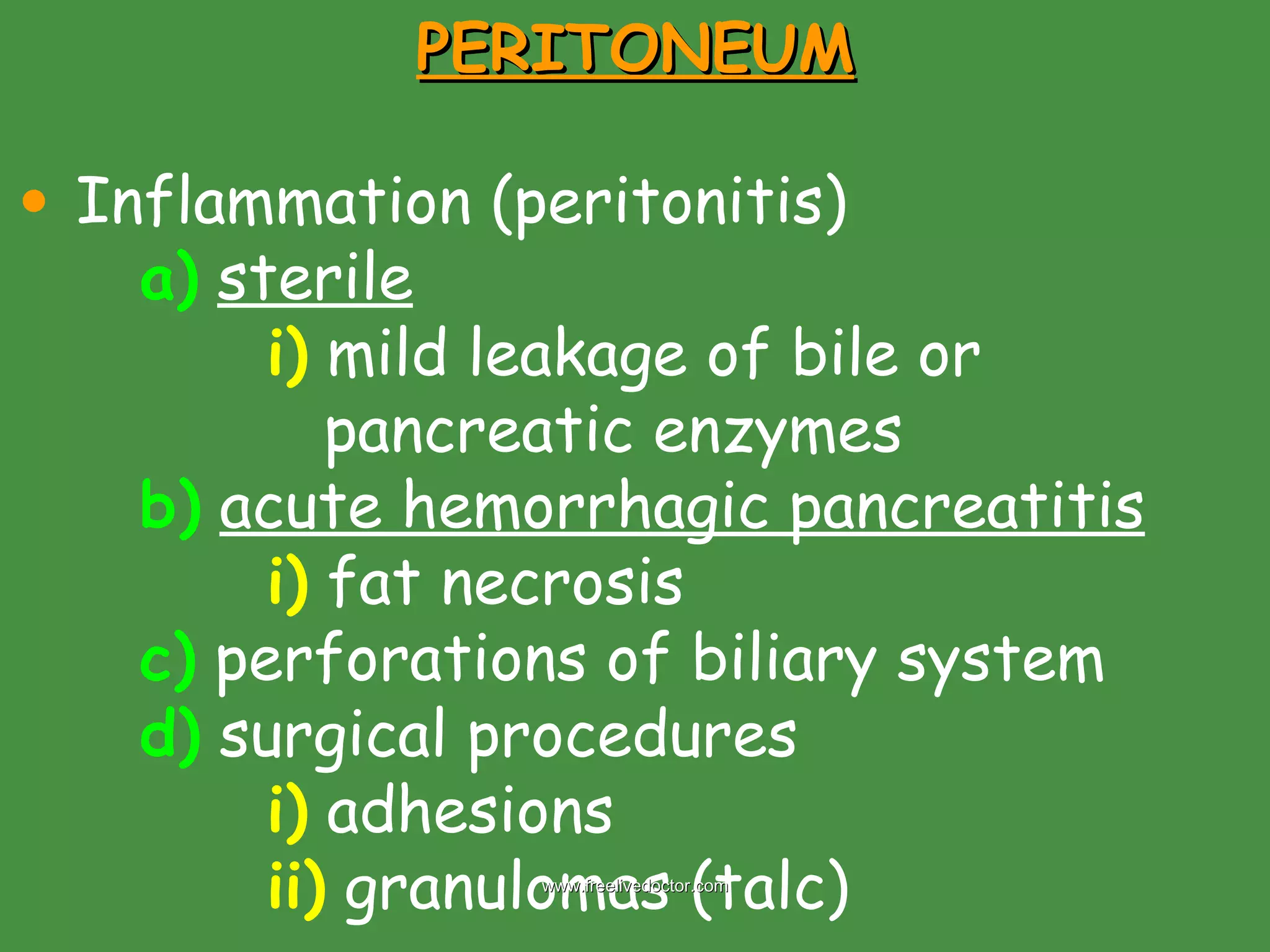
The document discusses several congenital and acquired abnormalities of the small and large intestines. It describes Meckel's diverticulum, Hirschsprung's disease, infectious enterocolitis including rotavirus, and necrotizing enterocolitis in neonates. It also discusses malabsorption syndromes such as celiac disease, tropical sprue, and Whipple's disease. Inflammatory bowel diseases like Crohn's disease and ulcerative colitis are compared. Other topics covered include intestinal obstruction, intestinal ischemia, hemorrhoids, diverticular disease, and intestinal neoplasms.