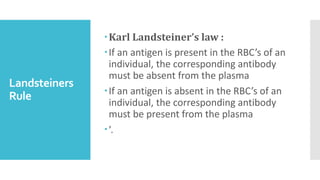
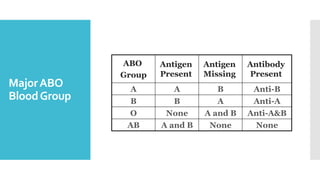
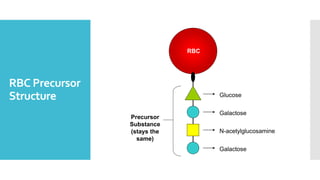
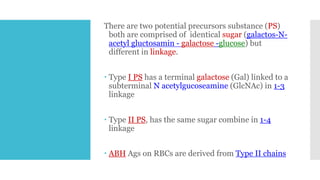
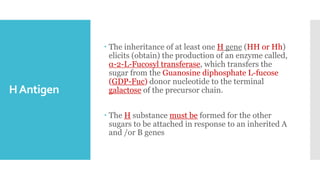
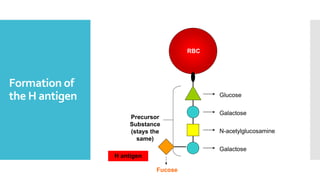
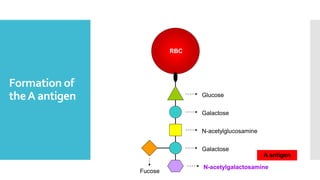
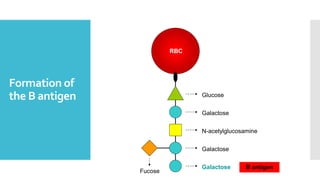
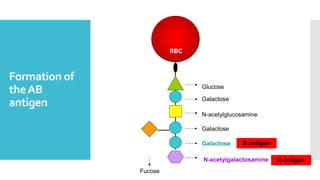
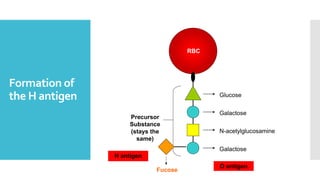
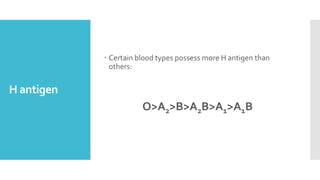
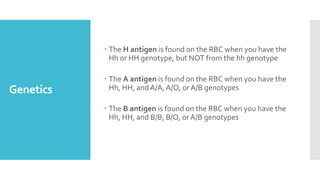
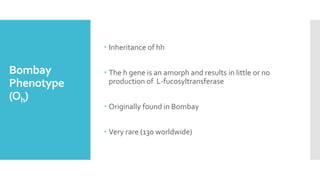
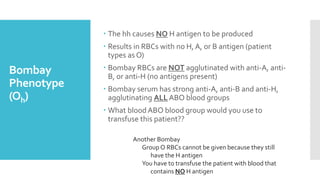
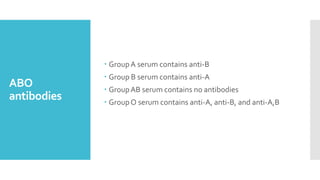
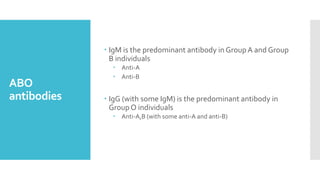
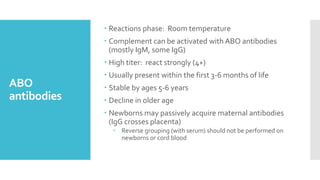
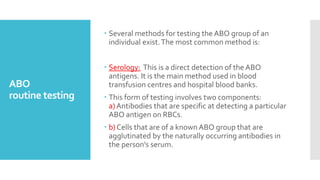
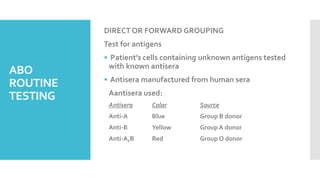
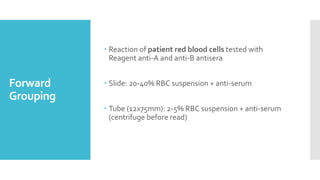
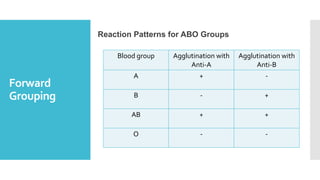
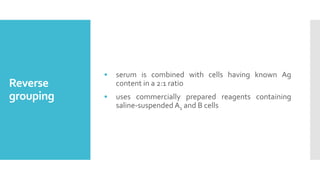
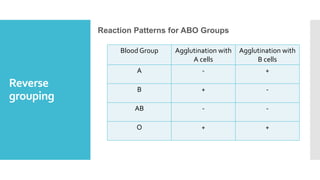
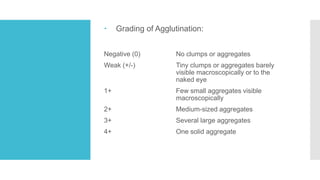
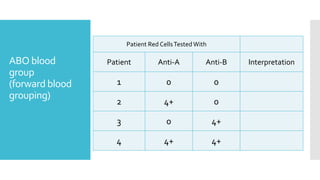
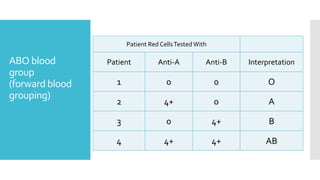
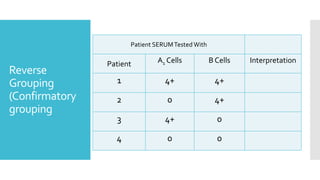
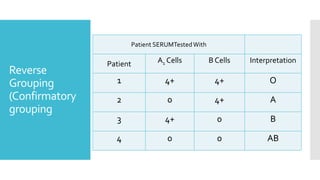
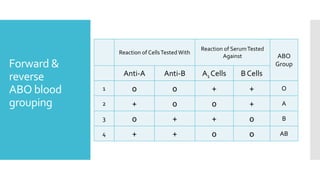
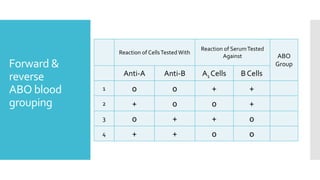
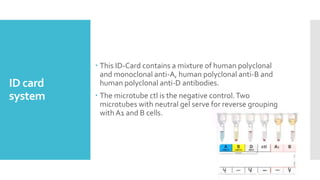
The document summarizes the ABO blood group system, which was discovered in 1901 by Karl Landsteiner. It describes the antigens and antibodies present in the four main blood groups (A, B, AB, and O) based on the presence or absence of the A and B antigens. The genes that code for the A, B, and H antigens are explained, as well as how they produce specific enzymes that add sugars to precursor structures on red blood cells. Forward and reverse blood grouping tests are outlined to determine a person's blood group.