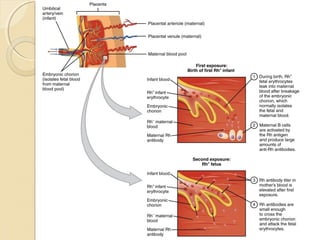
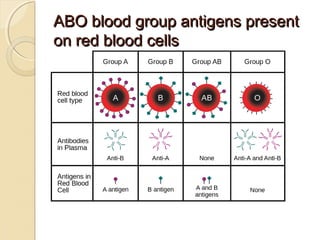
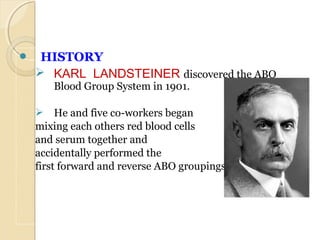
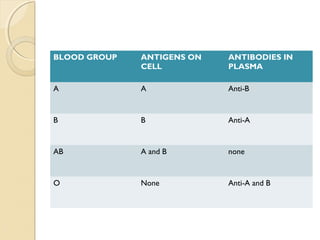
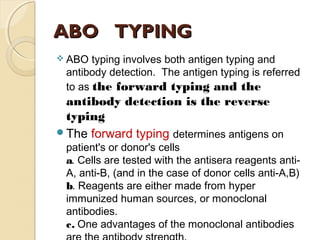
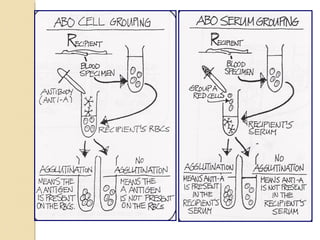
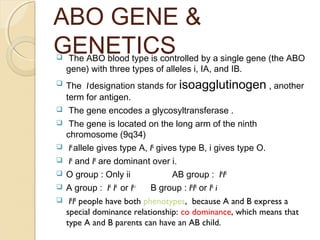
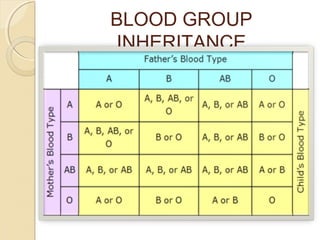
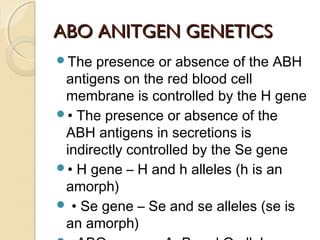
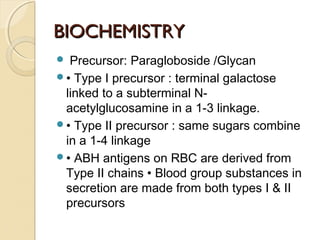
The ABO blood group system is the most significant in human blood transfusion, involving antigens present on red blood cells and associated antibodies. Discovered by Karl Landsteiner in 1901, ABO typing is essential for compatibility in blood transfusions, where the presence of anti-A or anti-B antibodies must be considered. Additionally, the system includes gene inheritance principles, the Bombay phenotype, and implications for Rh factors during blood transfusions and pregnancy.
![BOMBAY GROUPBOMBAY GROUP
The h/h blood group, also known as Oh[
or
the Bombay blood group, is a rare blood
type. This blood [phenotype] was first
discovered in Bombay, now known
as Mumbai, in India, by Dr. Y.M.Bhende in
1952.
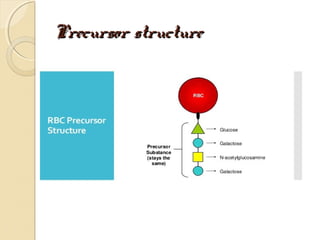
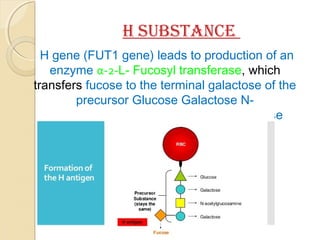
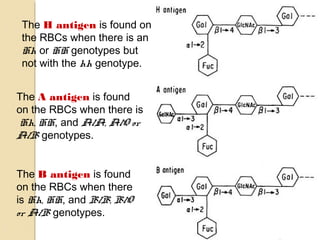
The Hh blood group contains one antigen,
the H antigen, which is found on virtually all
RBCs and is the building block for the
production of the antigens within the ABO
blood group.](https://image.slidesharecdn.com/abobloodgroupsystem-170121130000/85/Abo-blood-group-system-23-320.jpg)