Embed presentation
Downloaded 208 times

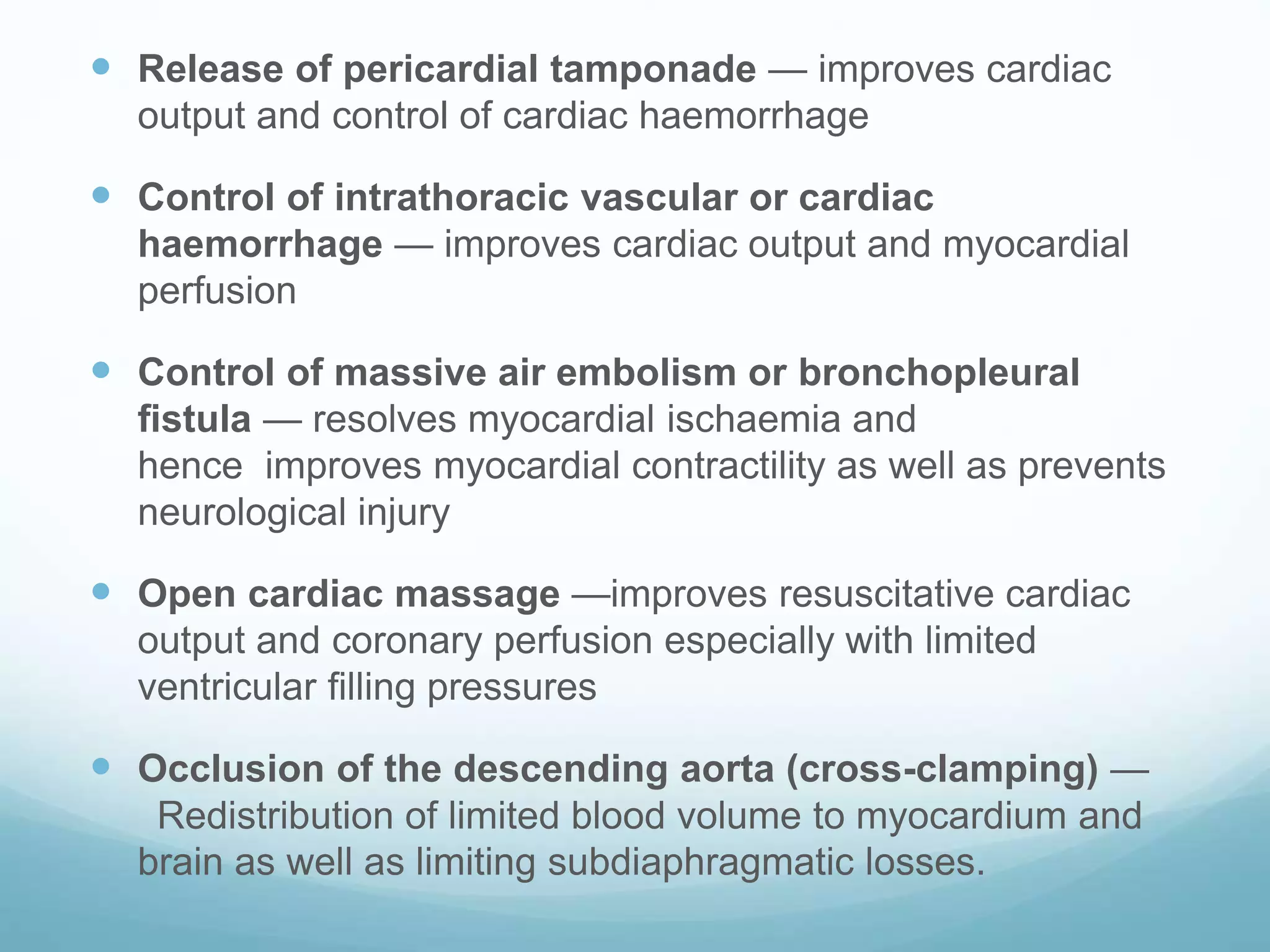
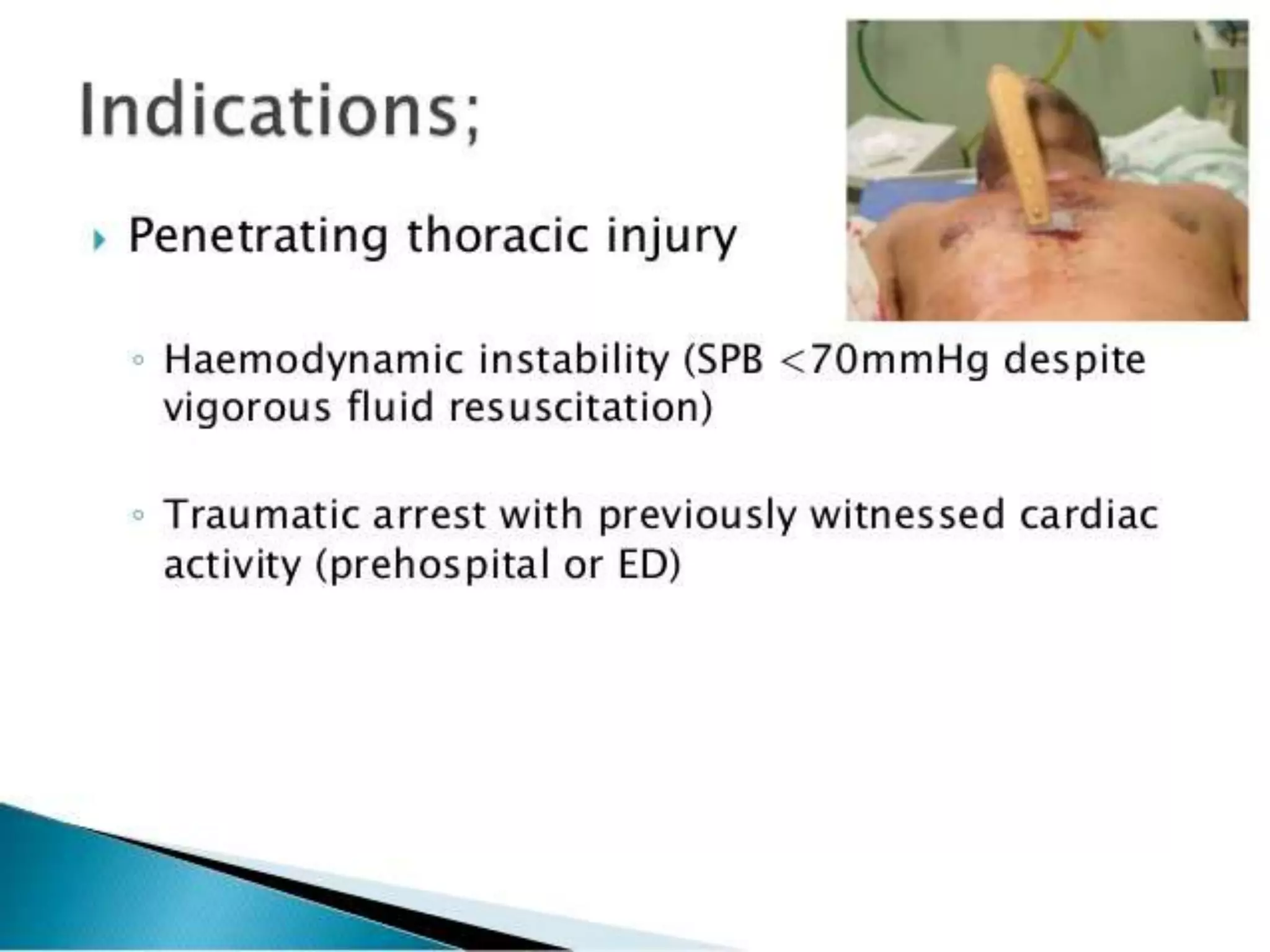
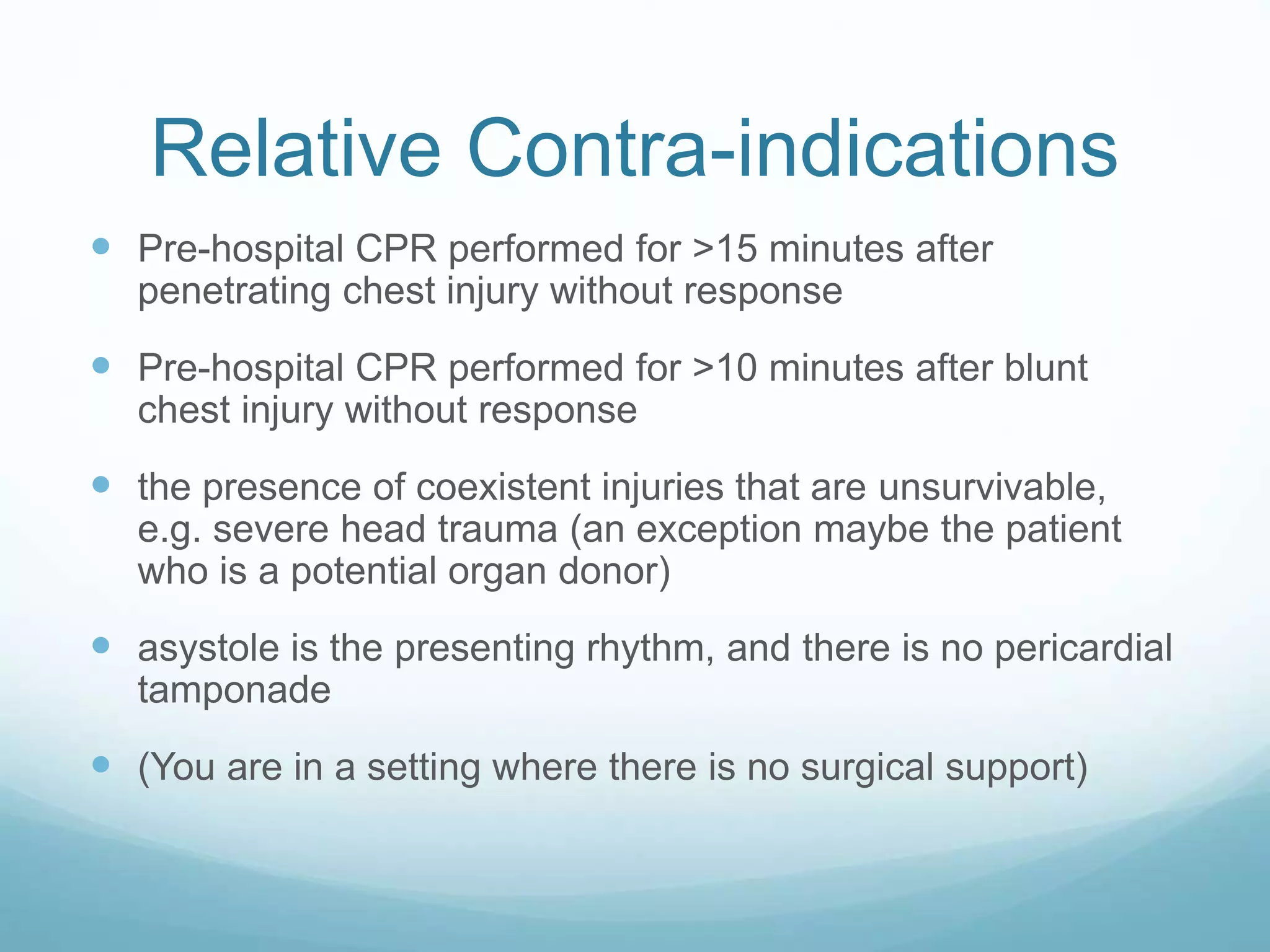
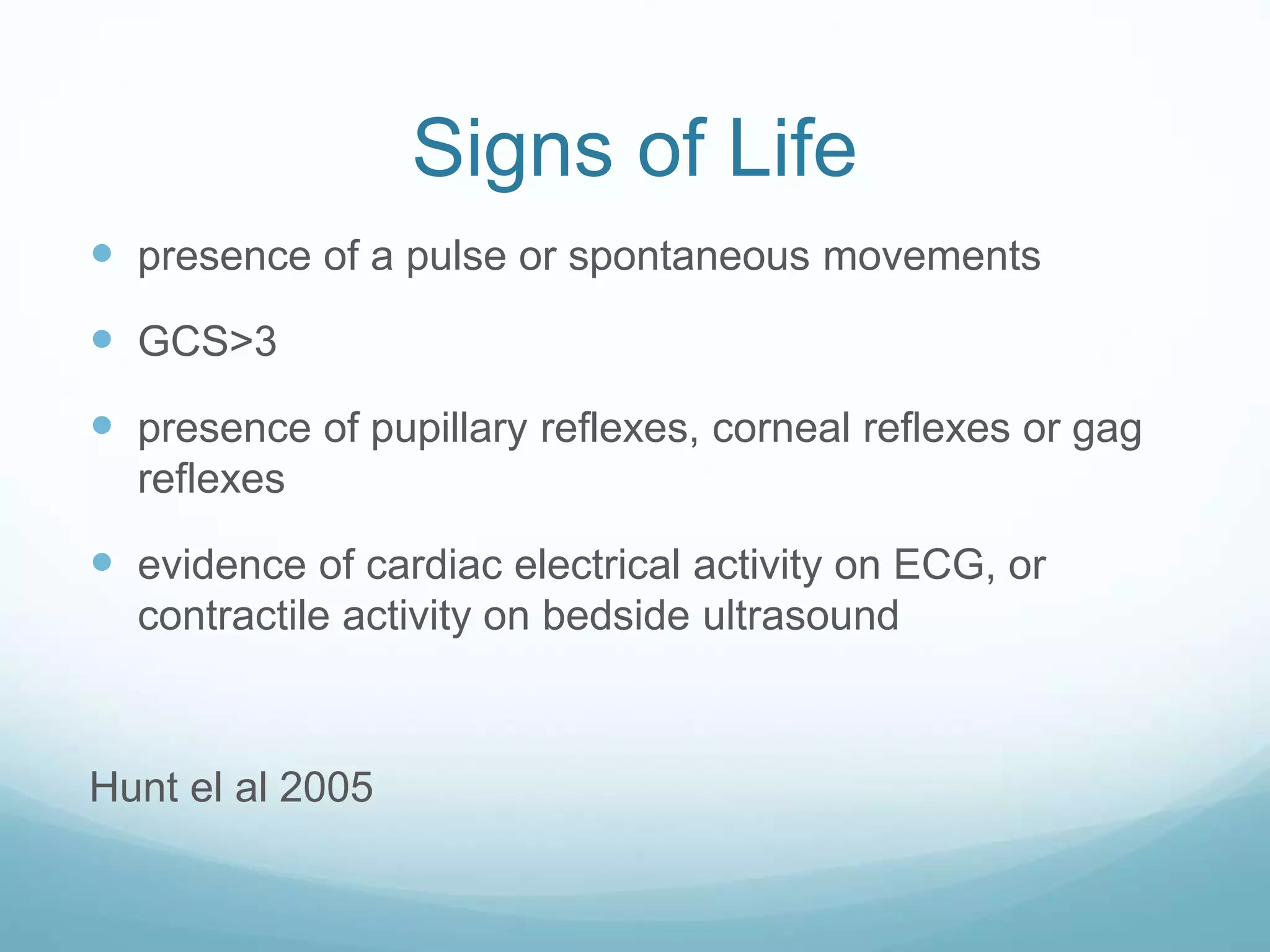
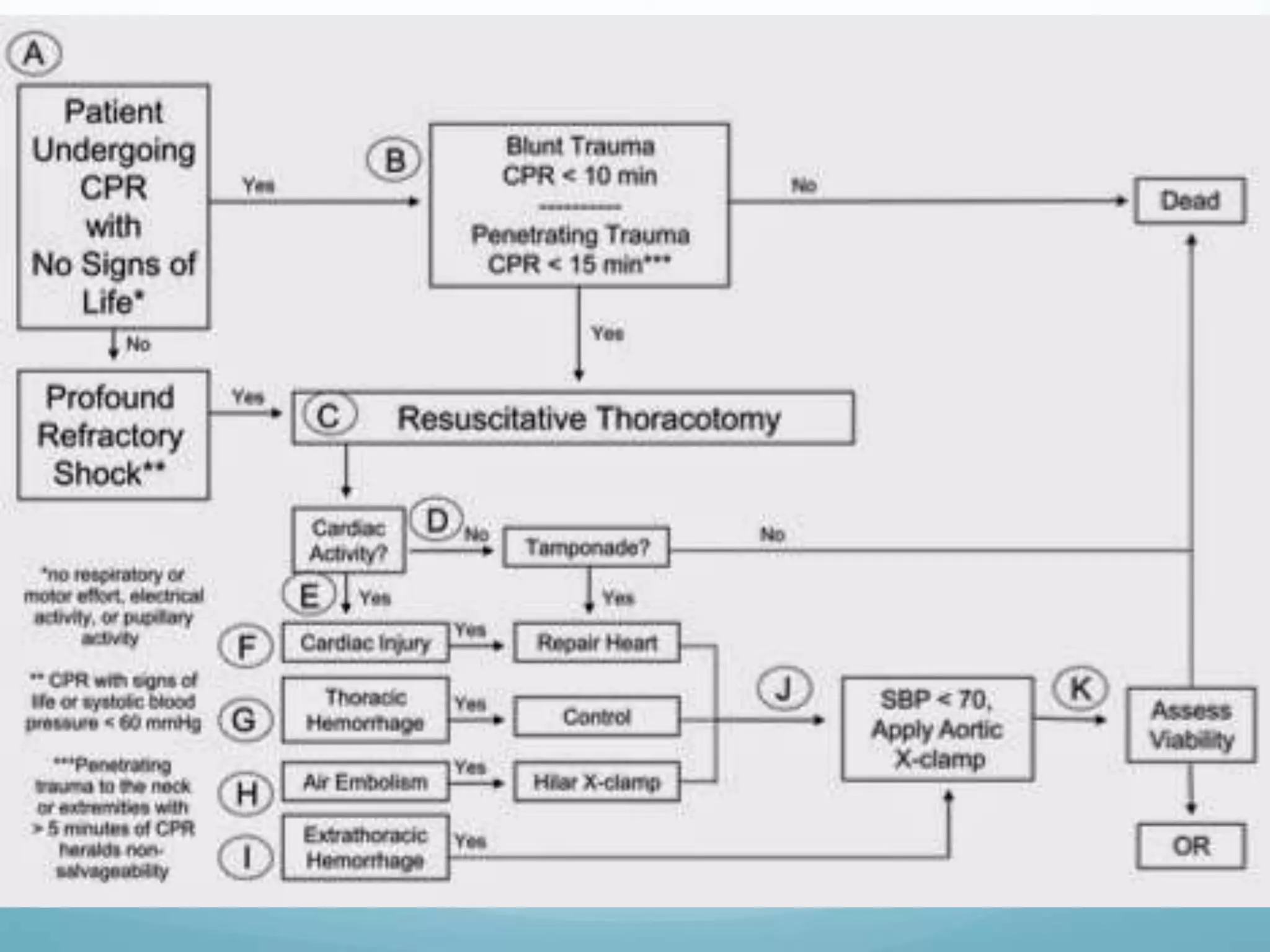
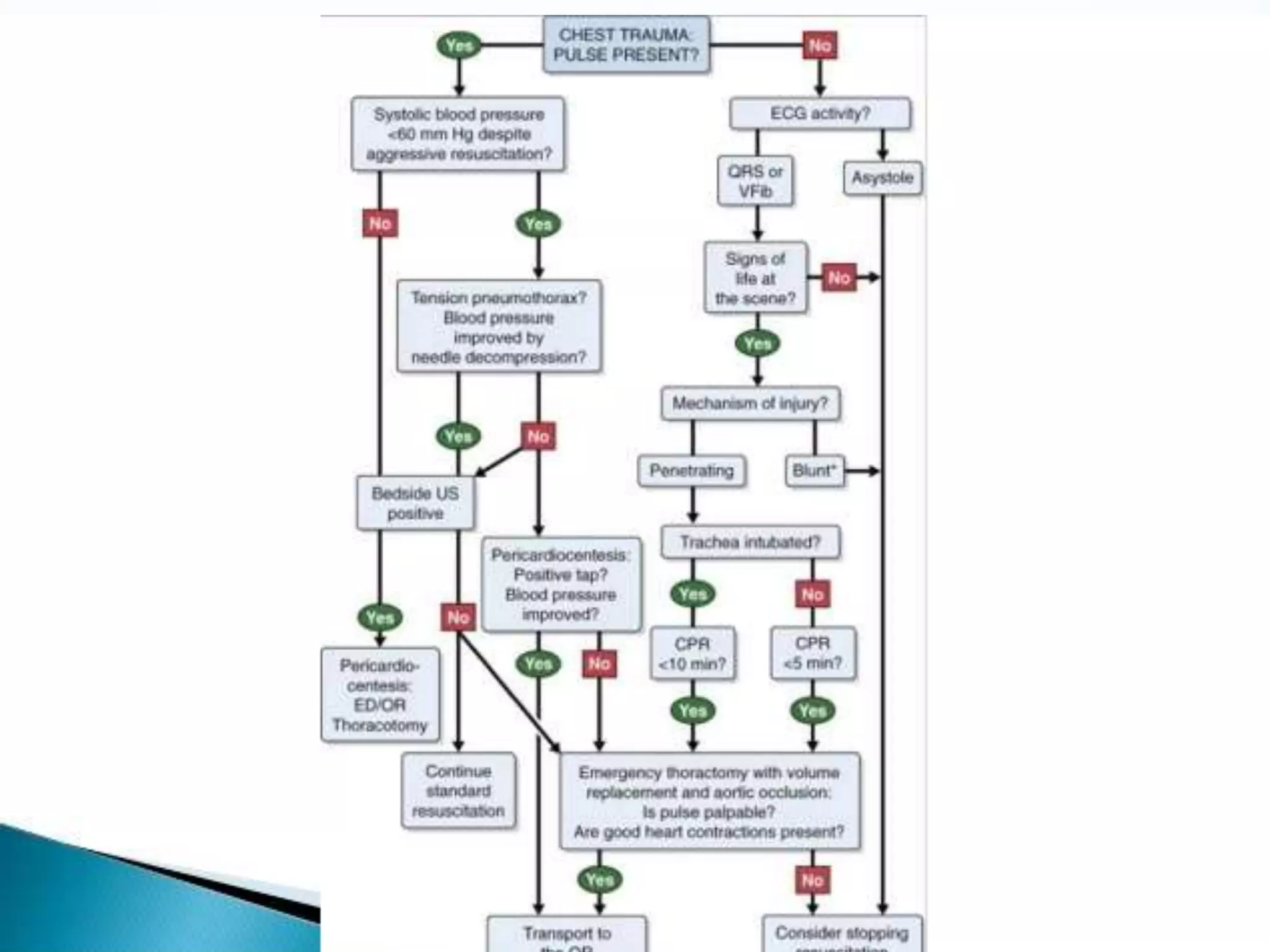
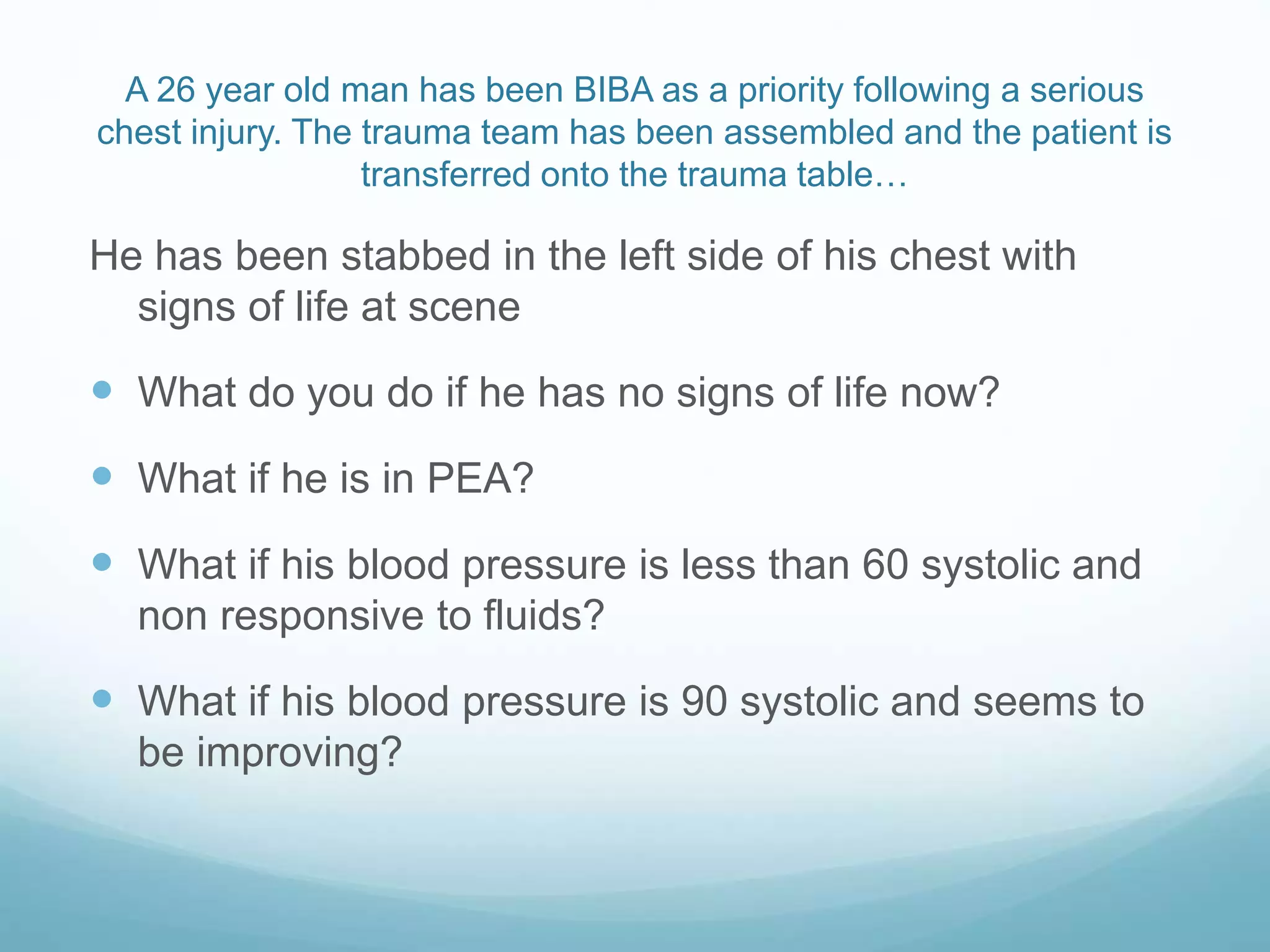
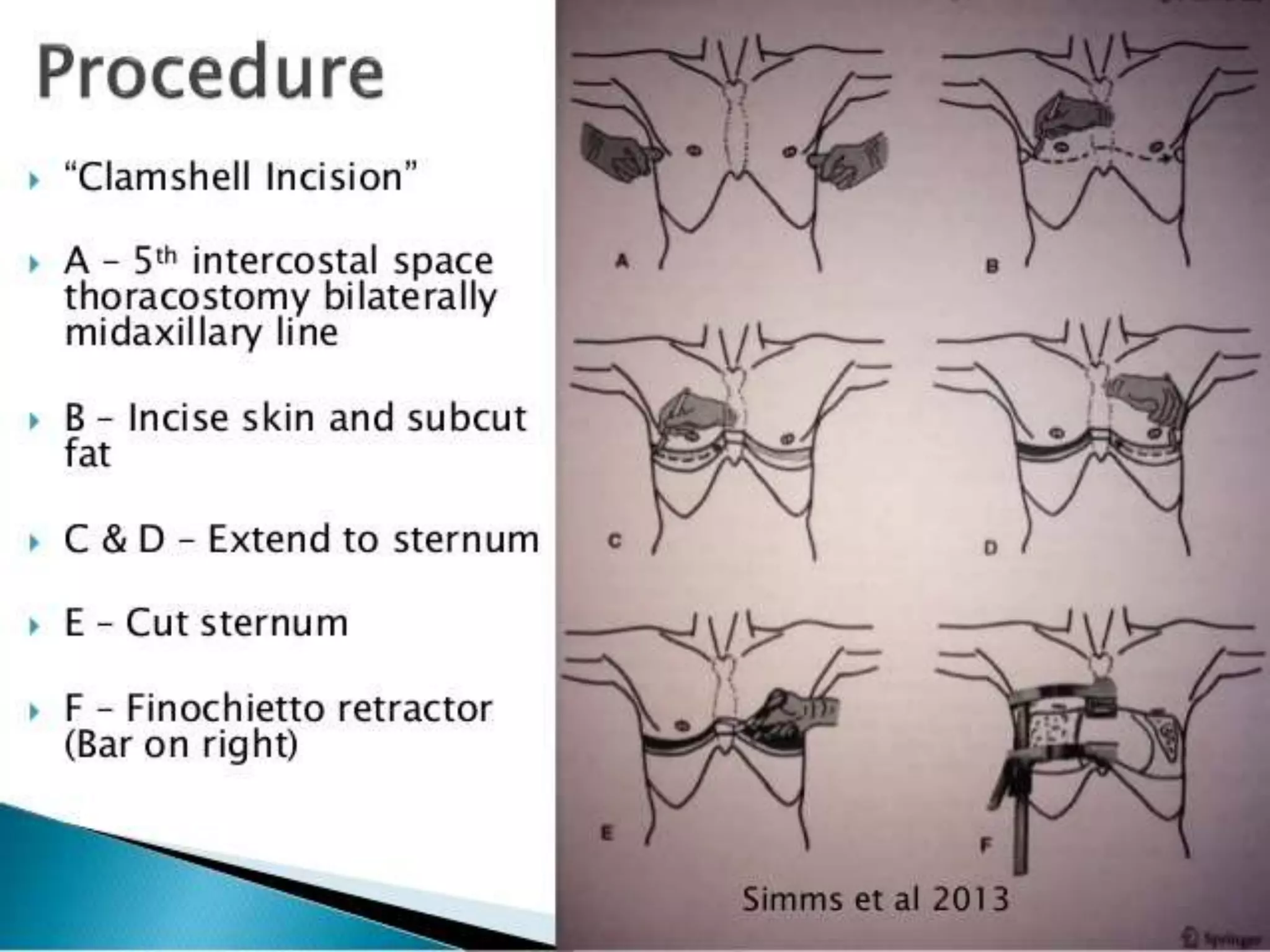
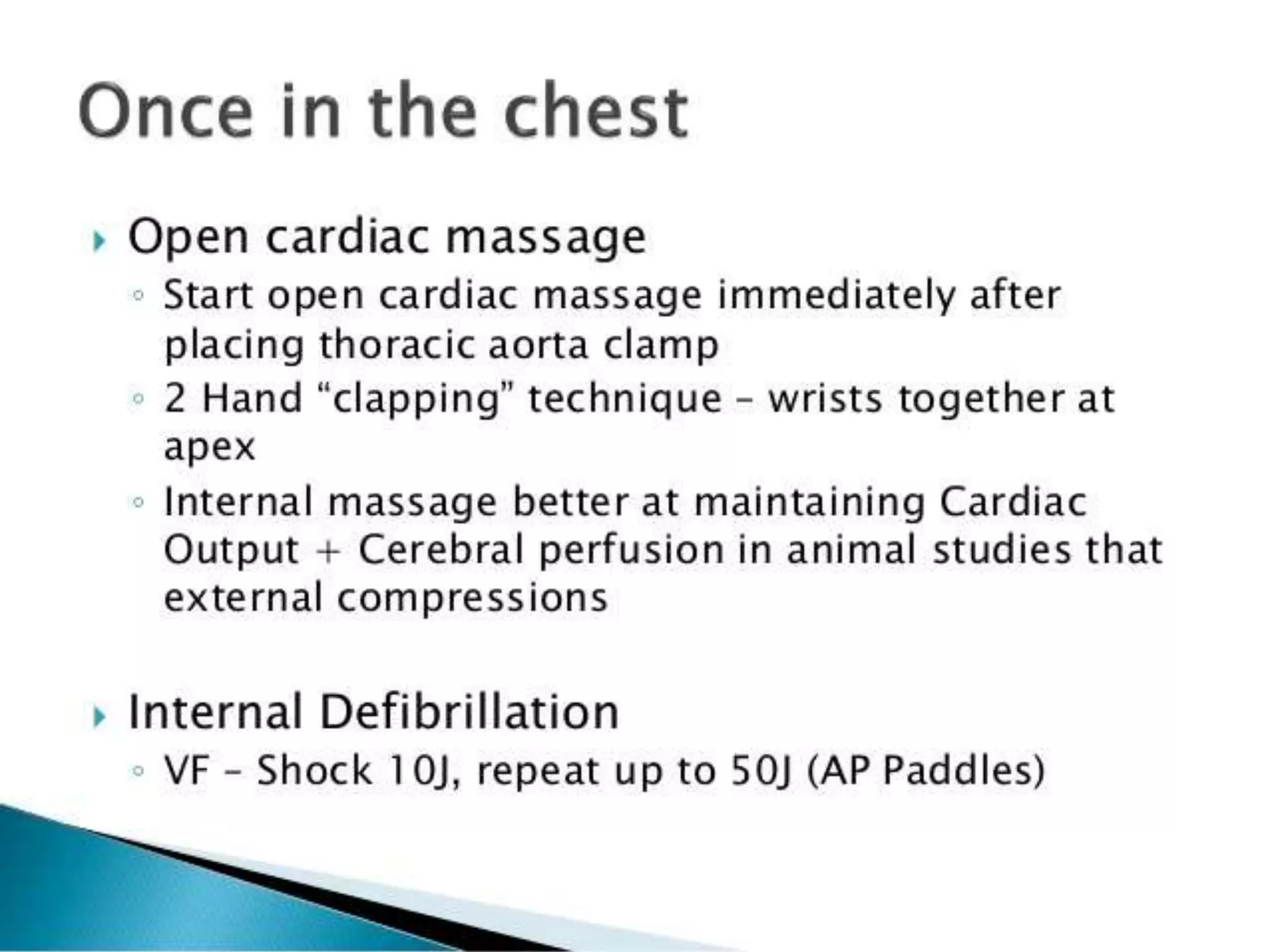
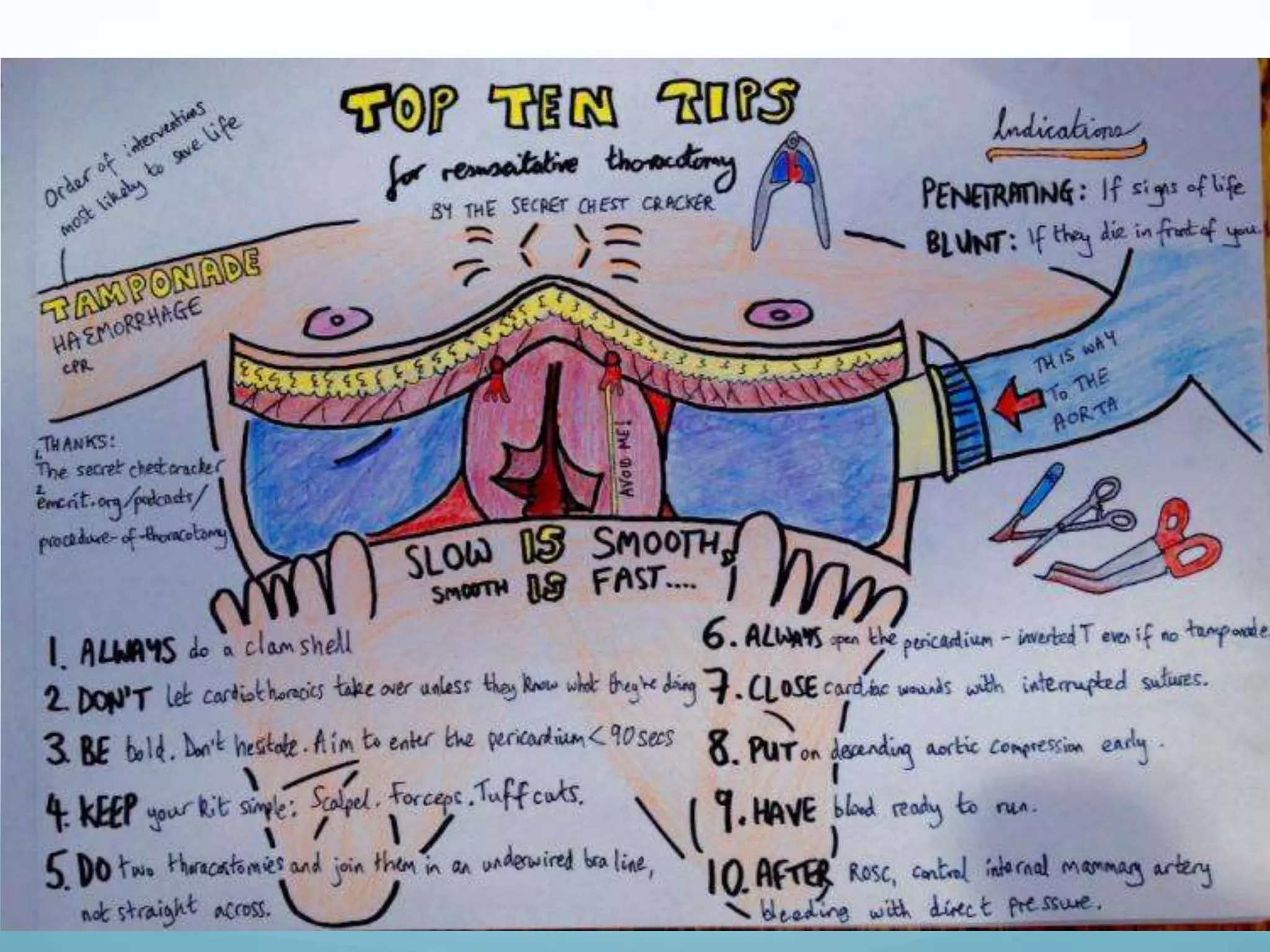

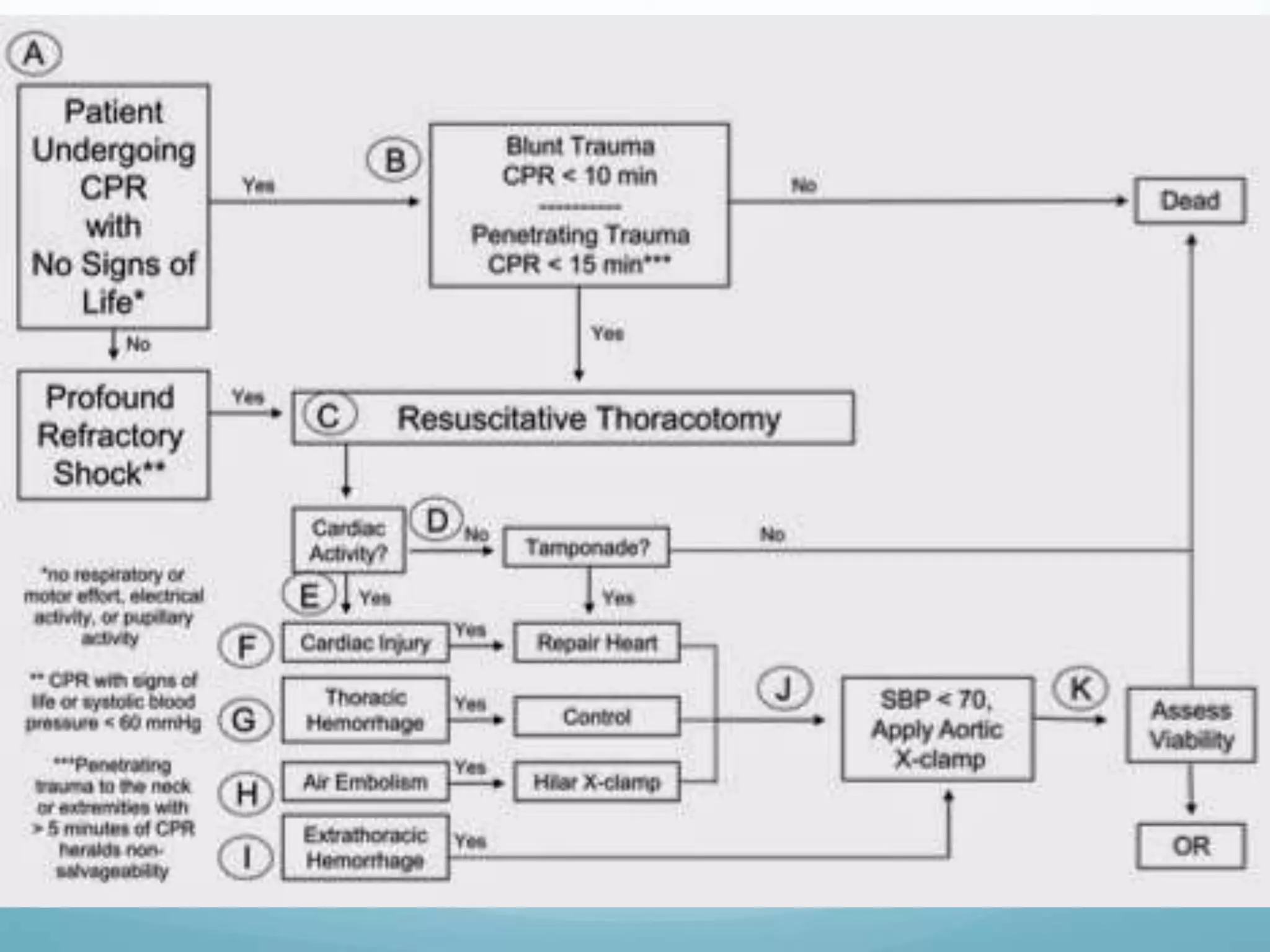
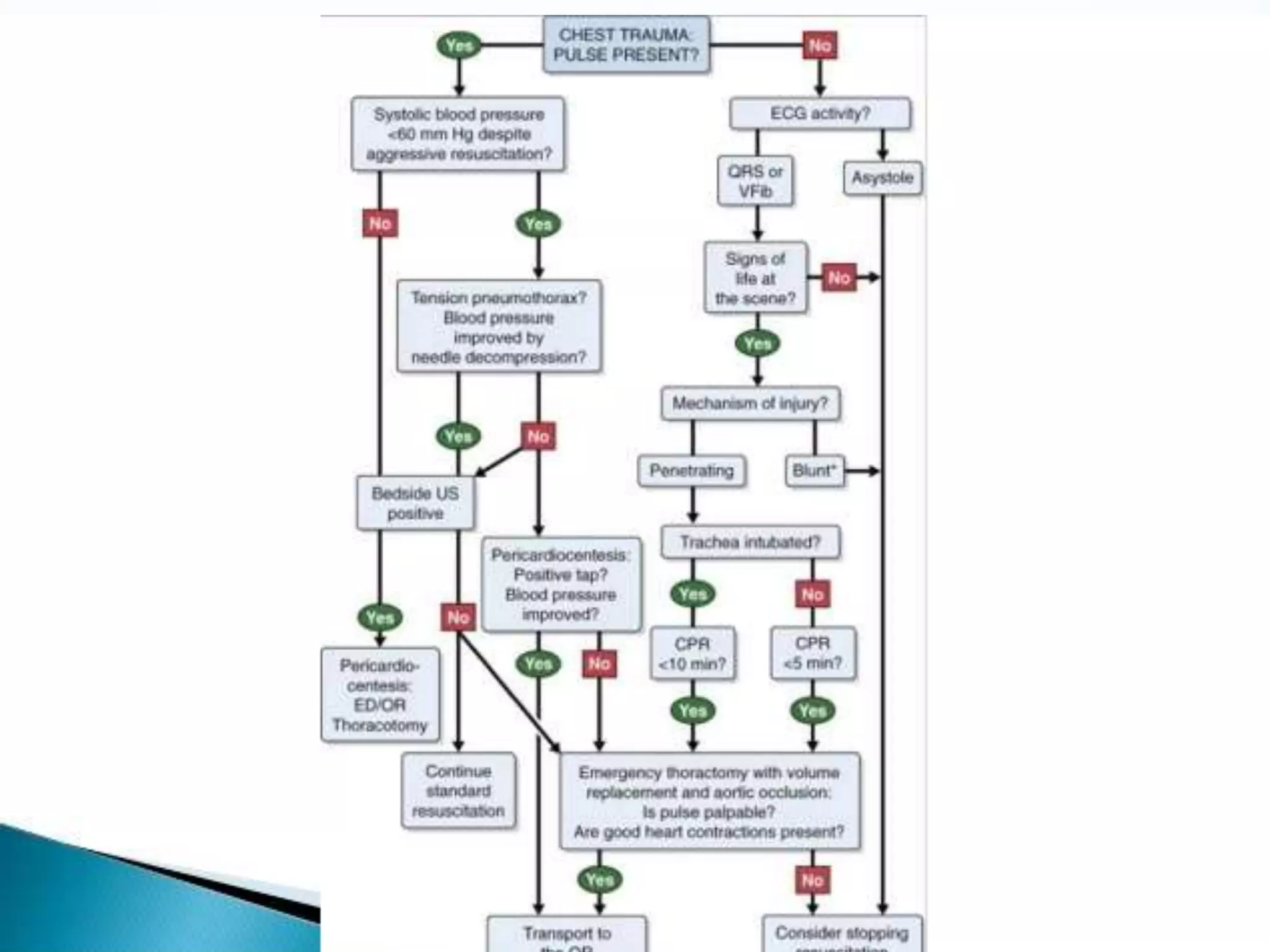
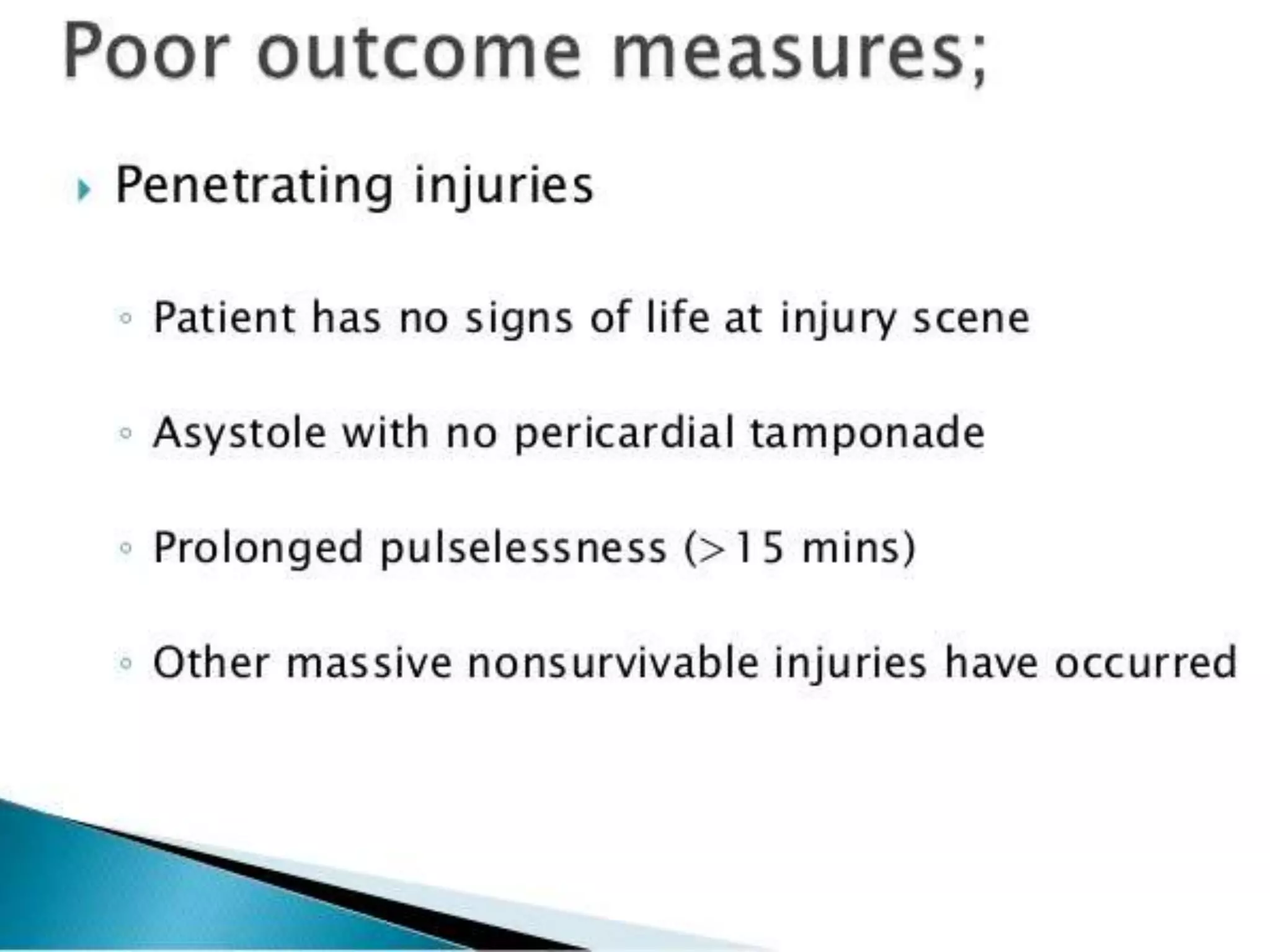
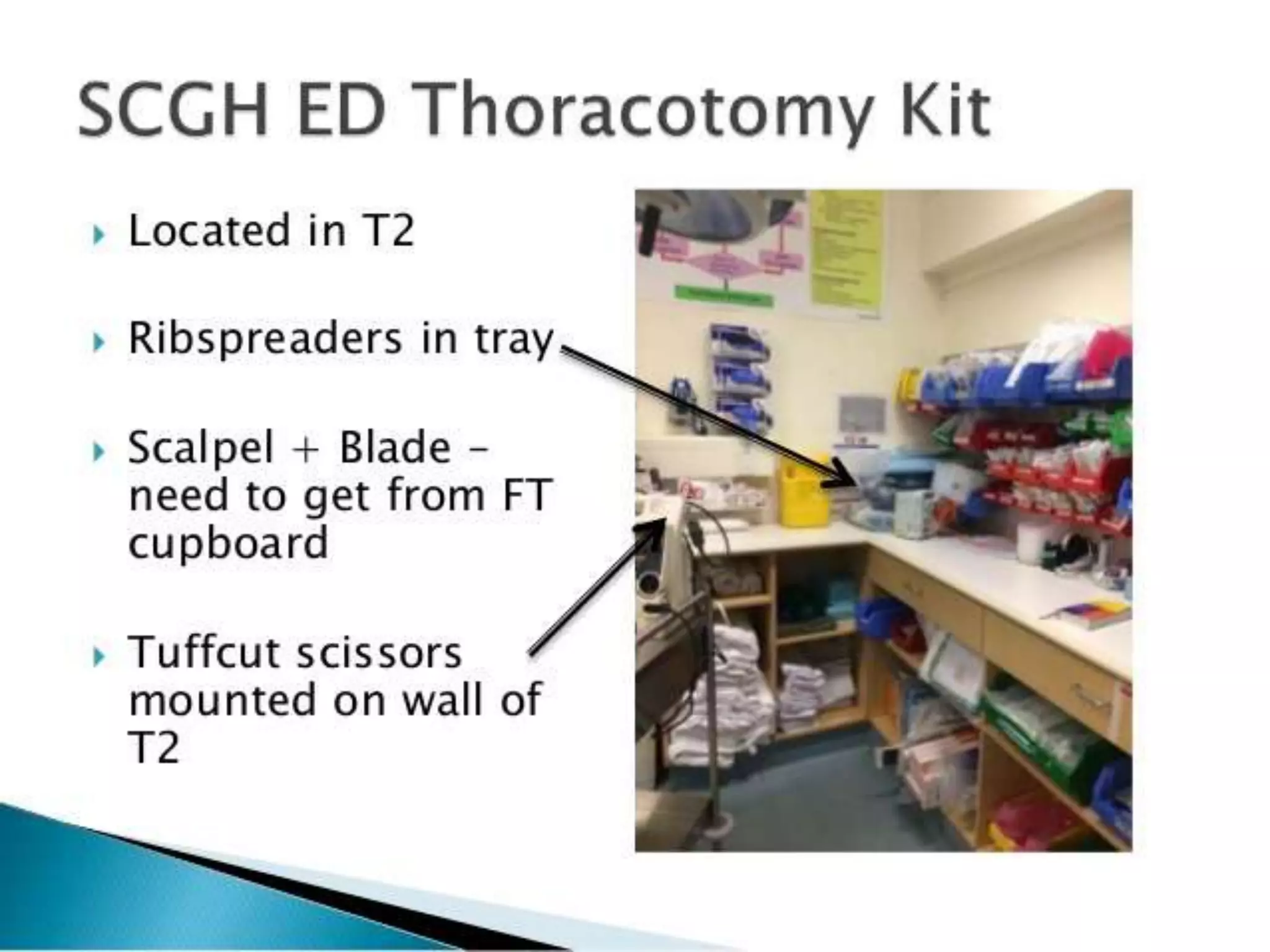
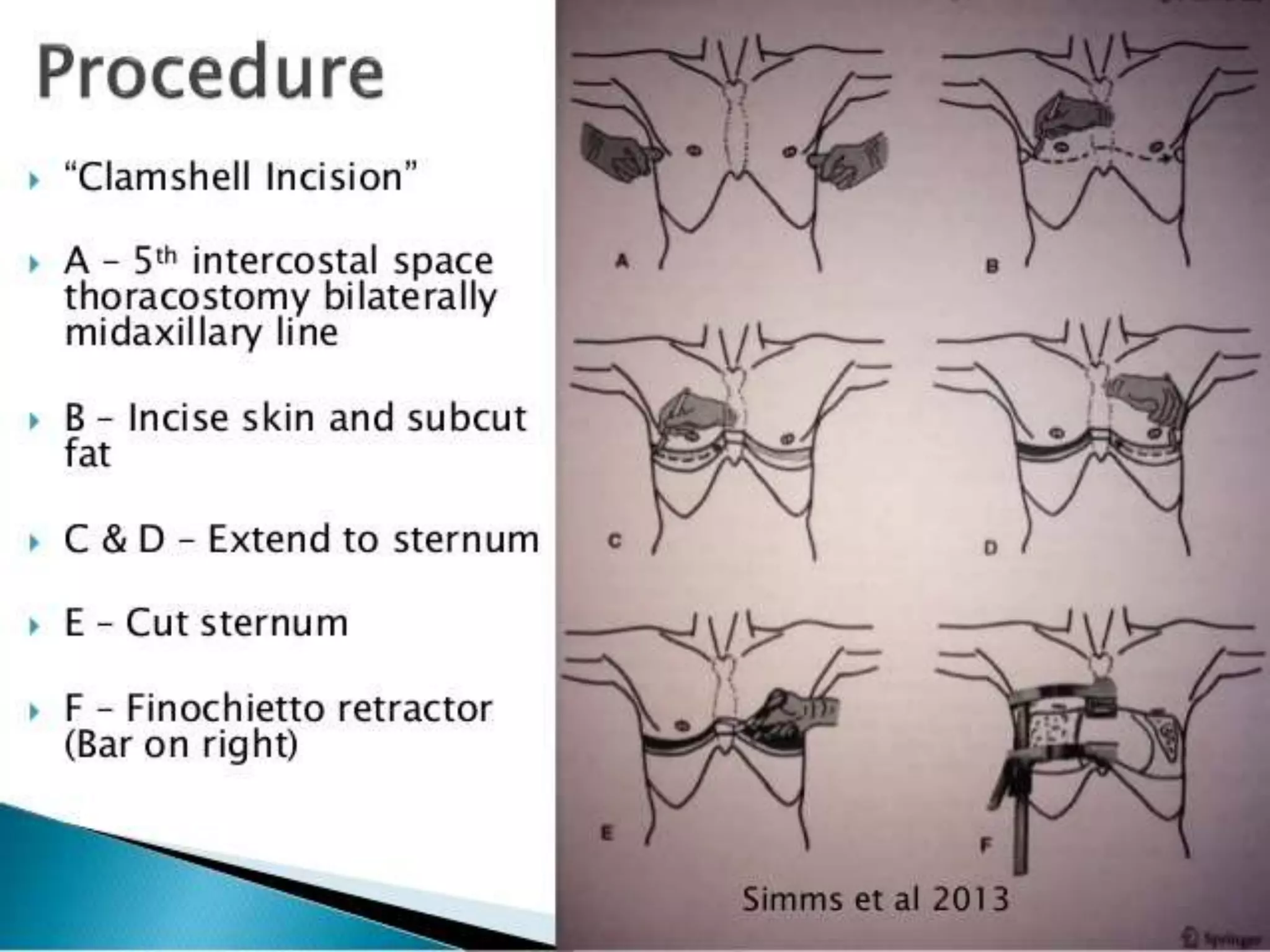
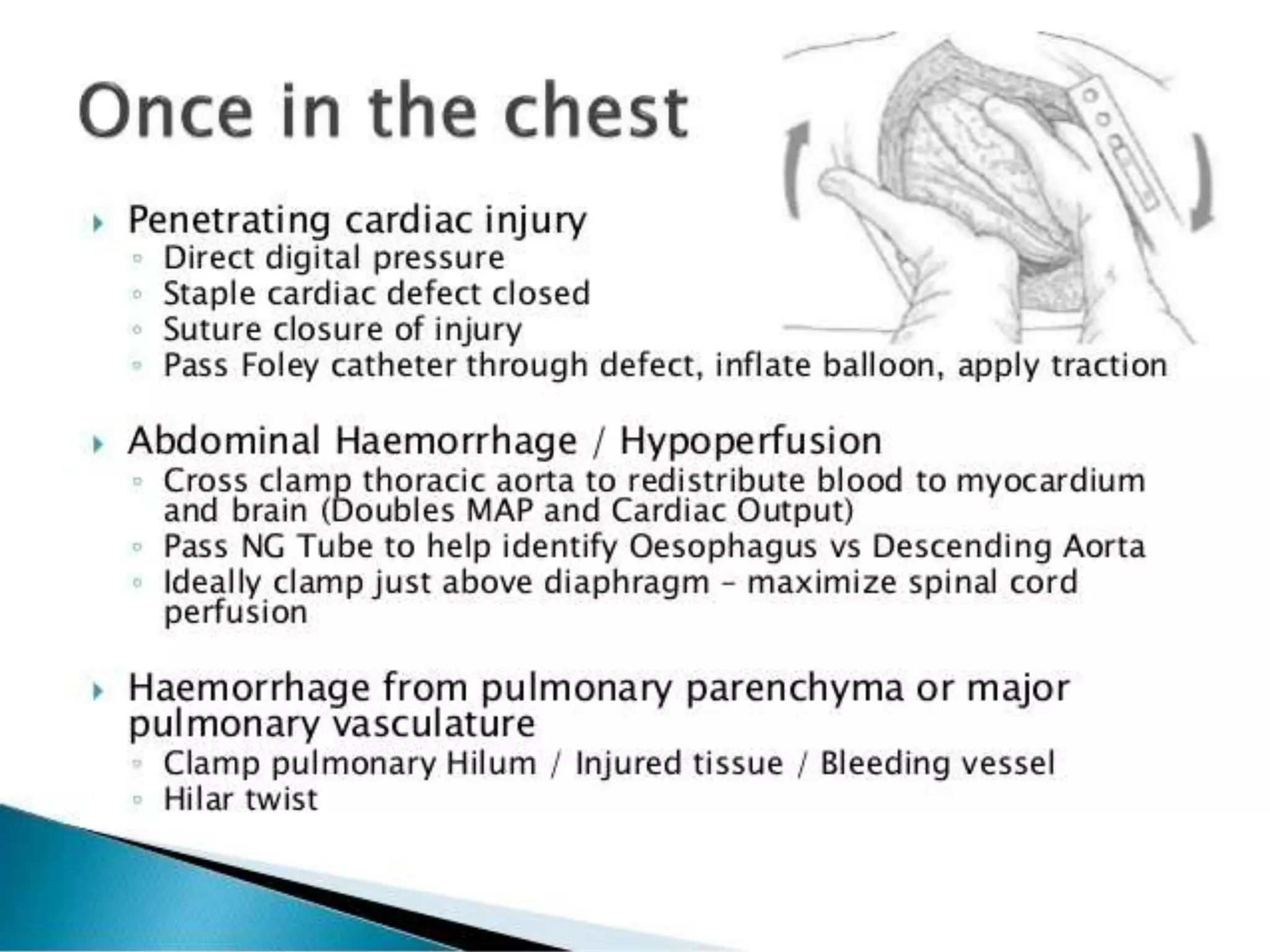
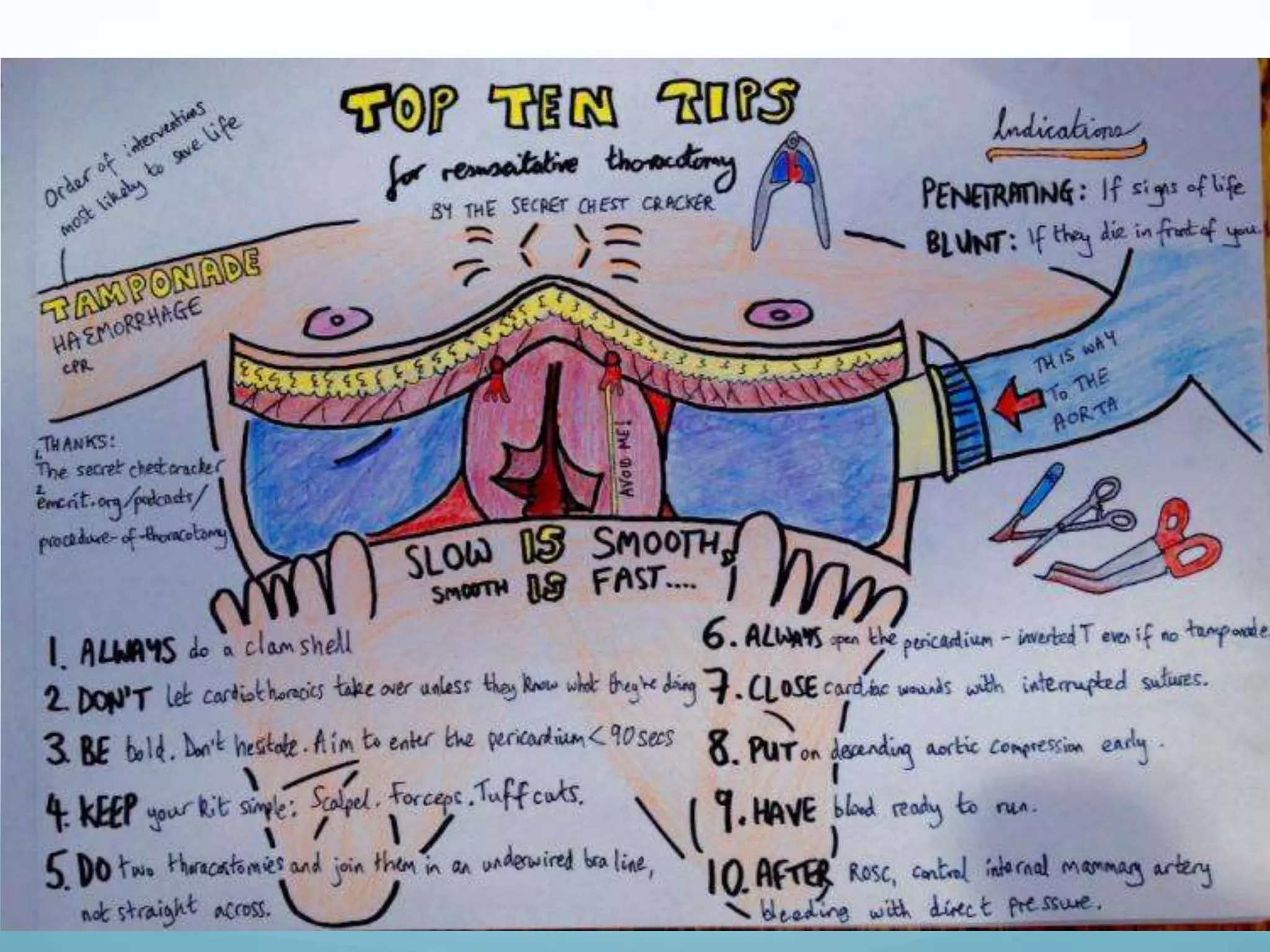
This document discusses emergency department thoracotomy (ED thoracotomy). It describes the procedures as: 1) Releasing pericardial tamponade to improve cardiac output and control cardiac hemorrhaging. 2) Controlling intrathoracic vascular or cardiac hemorrhaging to improve cardiac output and myocardial perfusion. 3) Controlling massive air embolism or bronchopleural fistula to resolve myocardial ischemia and improve contractility and prevent neurological injury. 4) Performing open cardiac massage to improve resuscitative cardiac output and coronary perfusion, especially with limited ventricular filling pressures. 5) Occluding the descending aorta to redistribute limited blood volume to the myocardium and brain