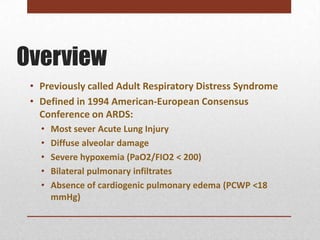
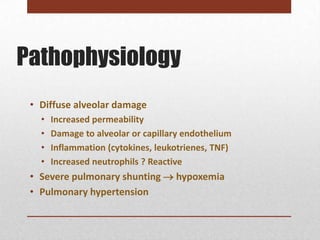
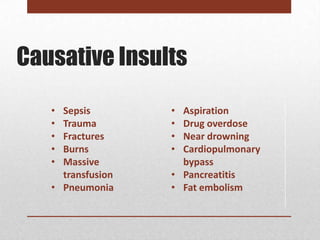
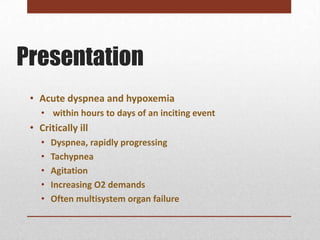
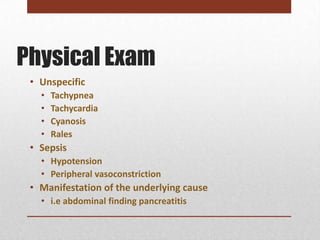
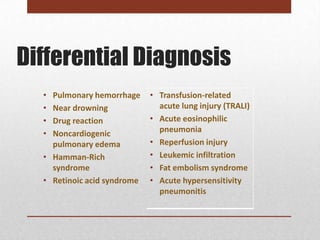
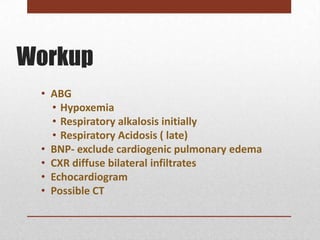
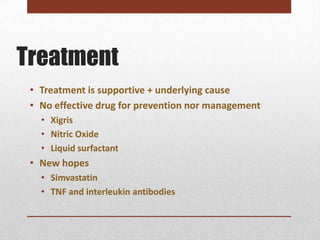
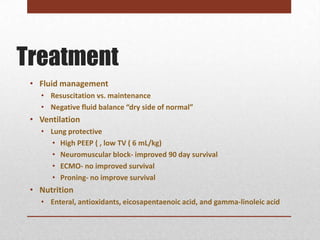
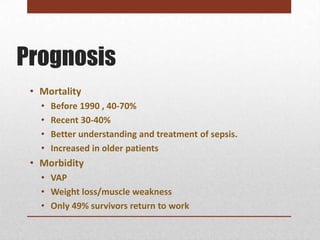
Acute Respiratory Distress Syndrome (ARDS) is a severe lung condition characterized by diffuse alveolar damage and severe hypoxemia. It is defined by acute onset, bilateral lung infiltrates seen on x-ray, and low oxygen levels with no cardiac cause. ARDS has many potential causes including sepsis, trauma, pneumonia, and near drowning. Treatment focuses on supportive care of the lungs and underlying condition. Mortality was historically high but is now around 30-40% with improved critical care, though long term outcomes are often impaired.