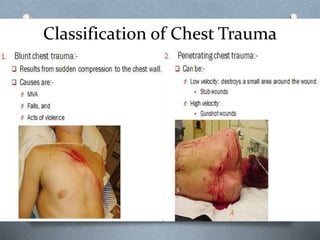
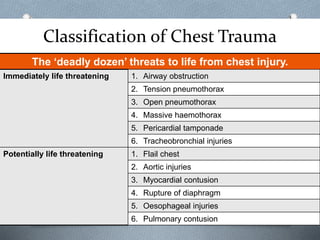
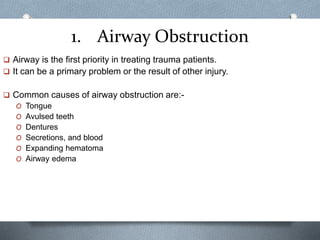
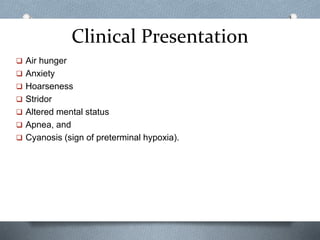
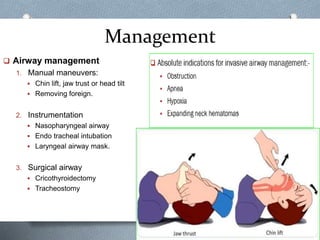
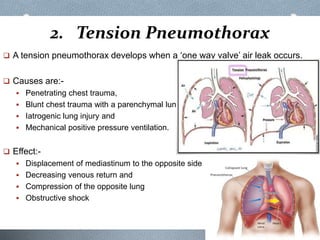
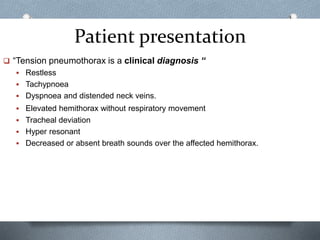
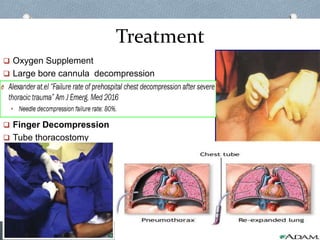
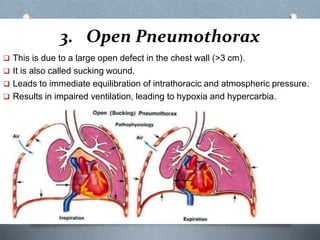
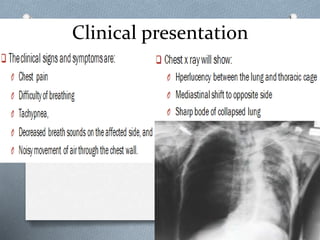
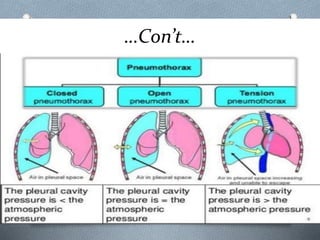
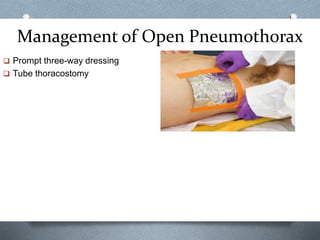
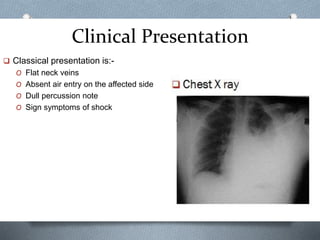
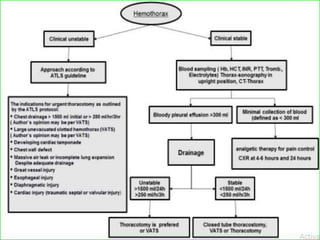
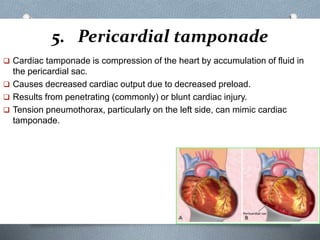
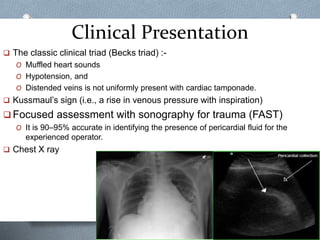
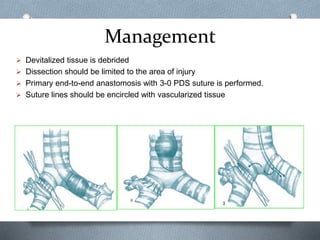
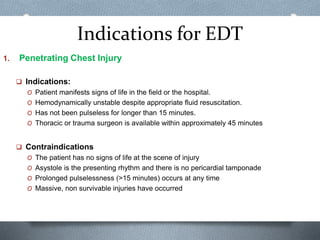
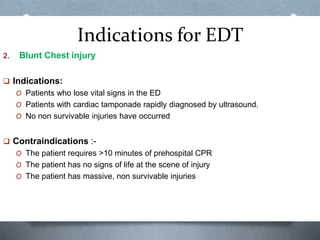
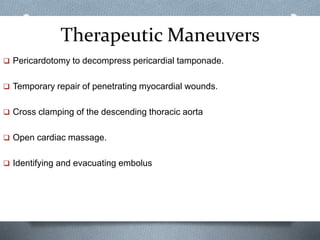
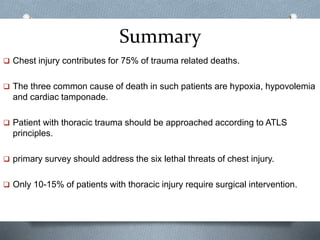
The document provides an overview of immediately life-threatening chest injuries. It classifies chest injuries as either immediately life-threatening or potentially life-threatening. The six immediately life-threatening conditions discussed in detail are airway obstruction, tension pneumothorax, open pneumothorax, massive hemothorax, pericardial tamponade, and tracheobronchial injuries. For each condition, the document outlines clinical presentation and emergency management strategies. It also discusses emergency department thoracotomy and provides indications and contraindications for its use.