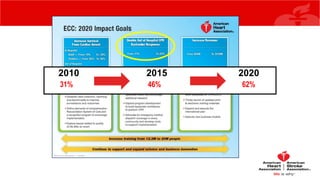
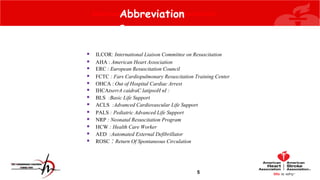
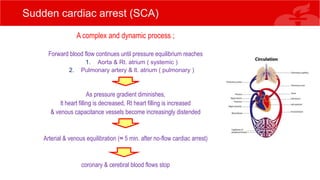
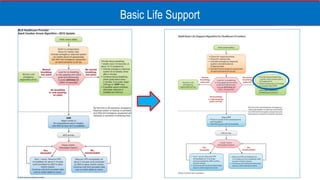
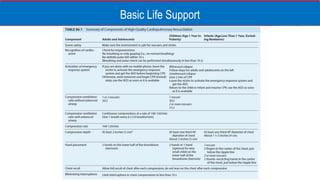
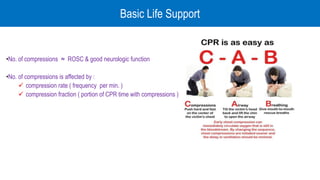
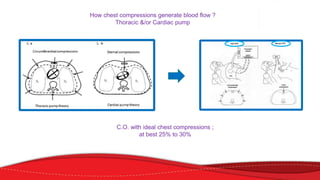
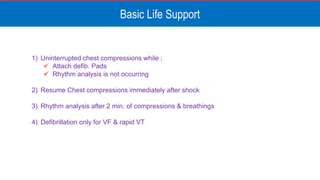
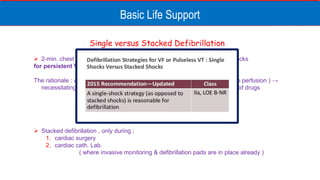
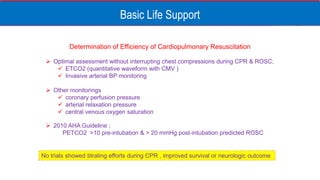
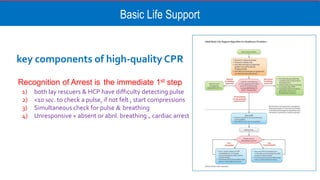
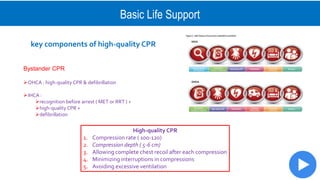
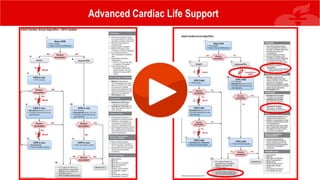
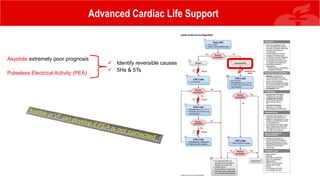
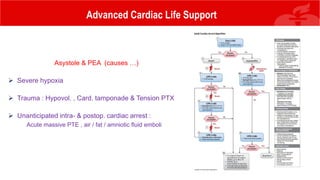
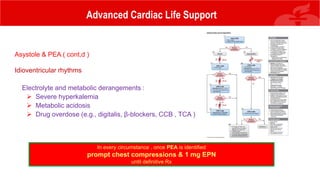
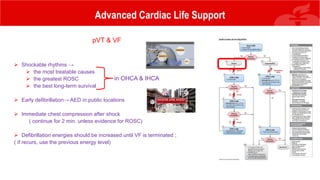
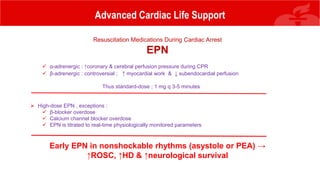
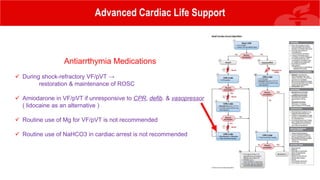
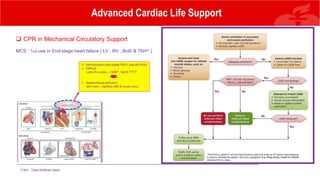
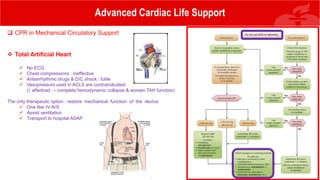
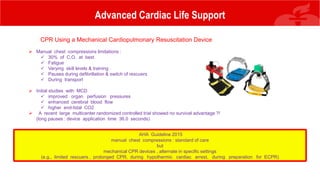
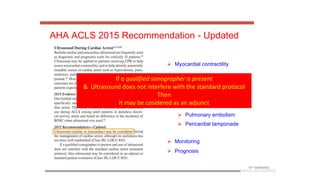
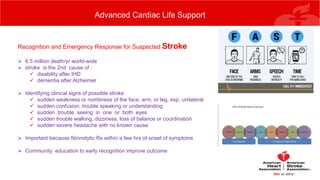
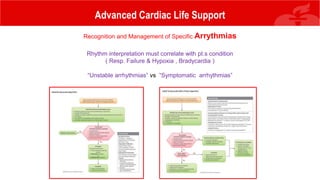
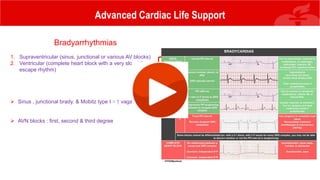
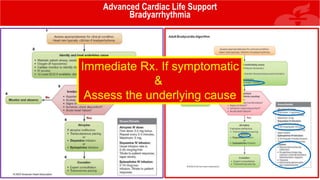
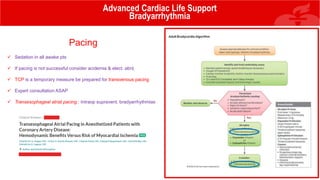
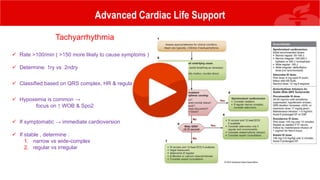
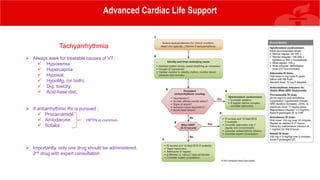
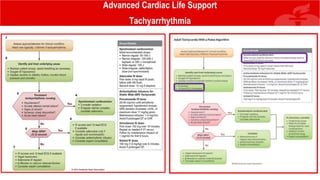
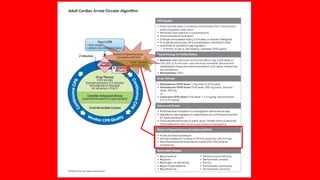
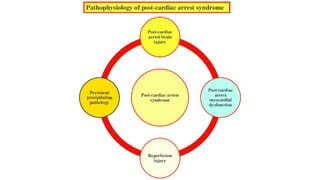
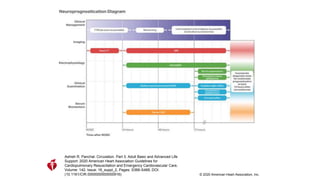
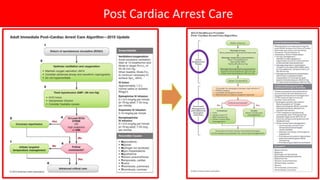
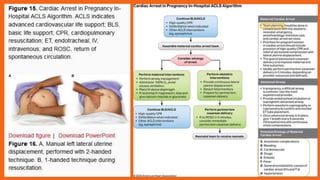
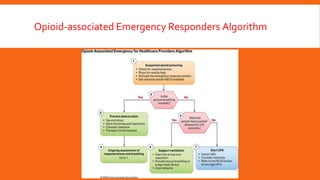
The document discusses the principles and practices of cardiopulmonary resuscitation (CPR) with an emphasis on the perspective from anesthesia, highlighting the importance of understanding cardiac arrest physiology, optimizing organ perfusion, and following established guidelines. It presents a comprehensive overview of basic and advanced life support techniques, the use of defibrillation, airway management, pharmacological interventions during cardiac emergencies, and post-arrest care. The document concludes with recommendations for effective CPR execution and the management of arrhythmias tailored to specific clinical conditions.