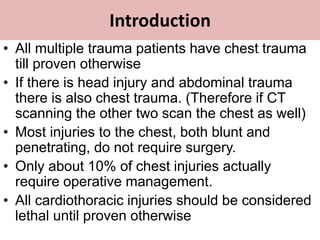
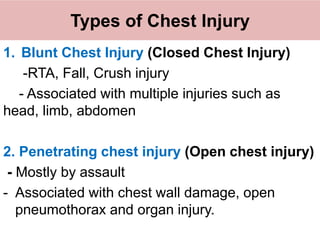
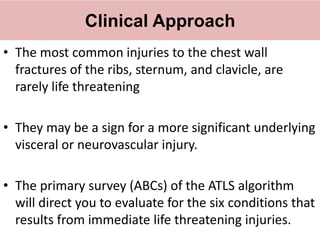
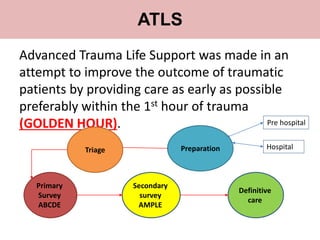
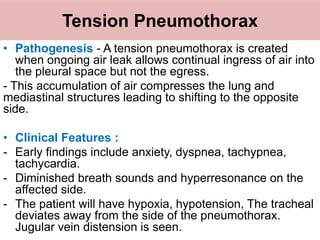
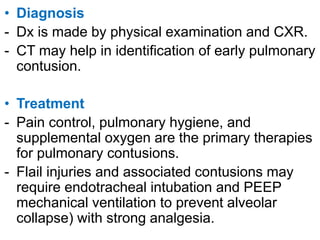
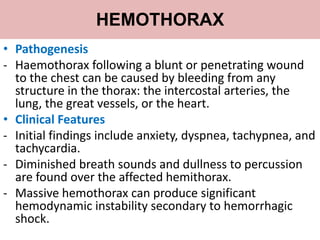
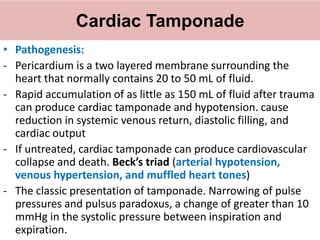
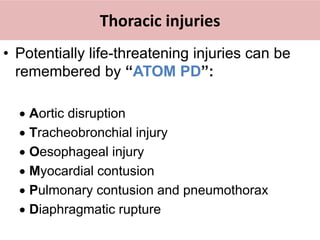
Chest trauma can involve injuries to the chest wall or internal organs. The primary survey focuses on life-threatening injuries like tension pneumothorax, massive hemothorax, or cardiac tamponade. Tension pneumothorax requires immediate needle decompression while massive hemothorax may require a chest tube or thoracotomy. Cardiac tamponade is treated with pericardiocentesis if due to blunt trauma or urgent surgery if from penetrating trauma. The secondary survey entails a full examination to identify injuries like lung contusions or aortic disruption that require further treatment or monitoring.