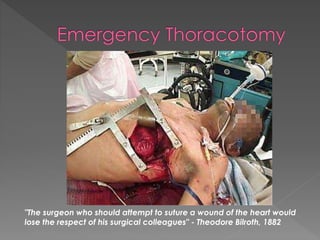
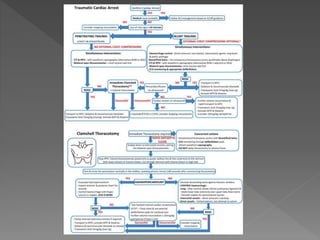
The document discusses the management of traumatic cardiac arrest. Key points include:
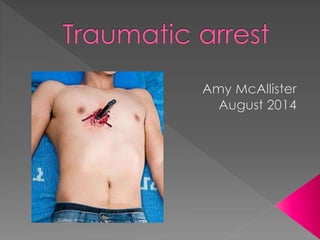
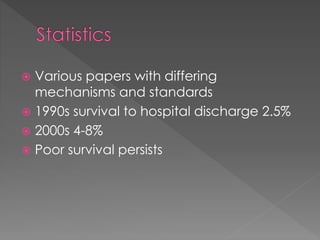
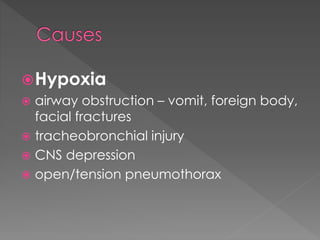
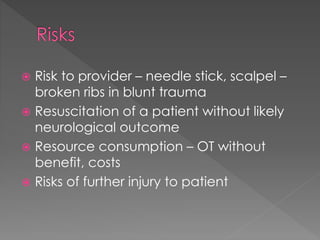
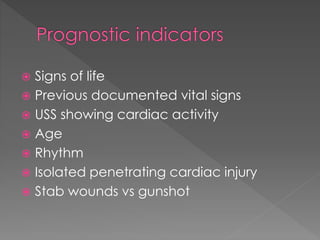
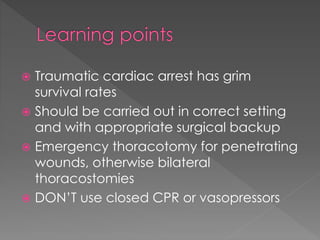
- Traumatic cardiac arrest has a very poor prognosis, usually caused by penetrating or blunt chest injuries.
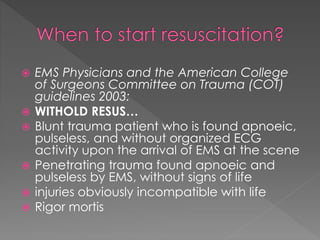
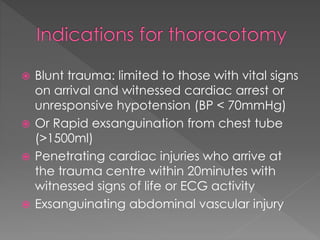
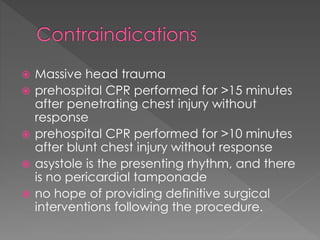
- For blunt trauma patients, emergency thoracotomy is only recommended if they had witnessed cardiac arrest or hypotension on arrival.
- For penetrating chest injuries, emergency thoracotomy within 20 minutes of injury may be considered if signs of life were witnessed or if ECG activity is present.
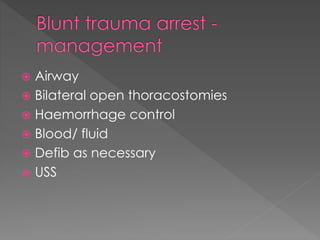
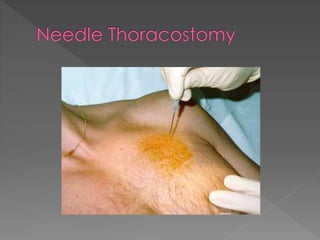
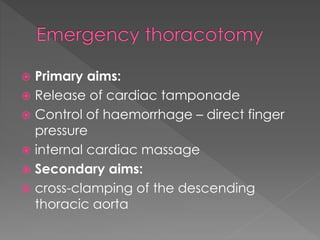
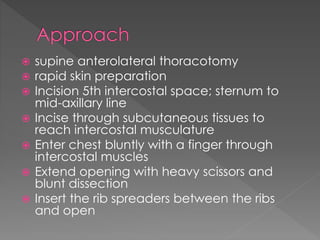
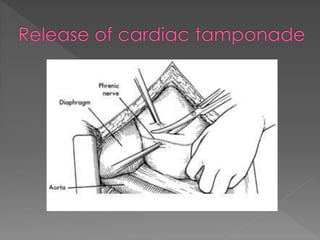
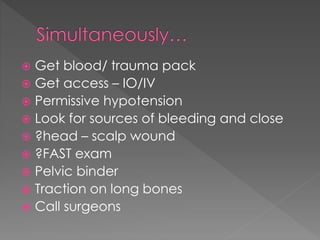
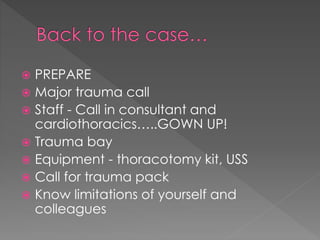
- Initial management involves bilateral thoracostomies to relieve tamponade, control bleeding, and provide fluids and medications. Emergency thoracotomy may be attempted in select cases but survival rates are extremely low.