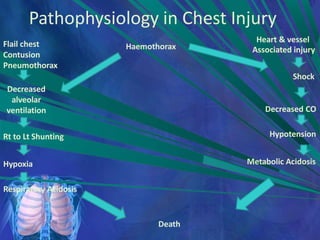
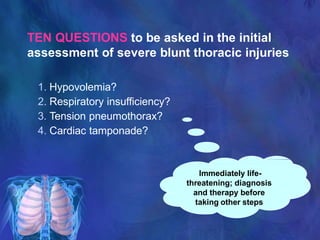
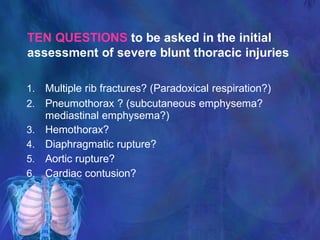
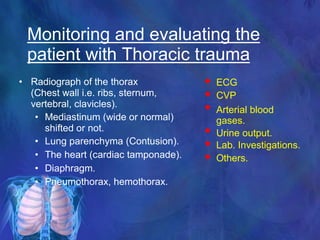
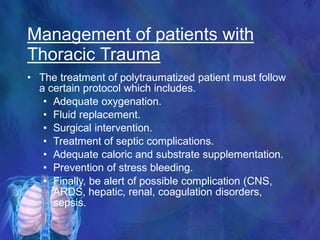
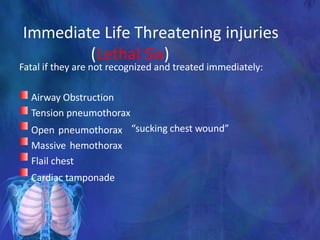
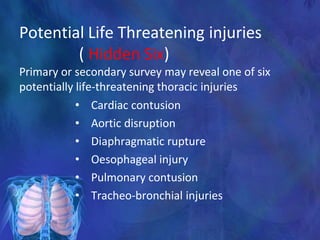
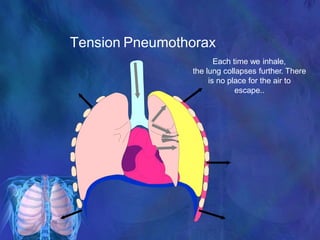
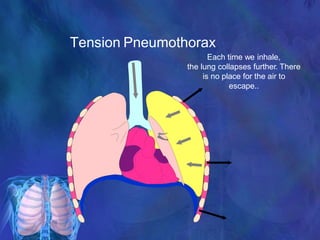
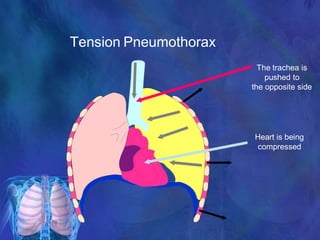
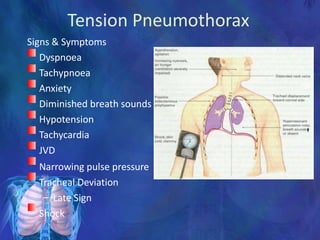
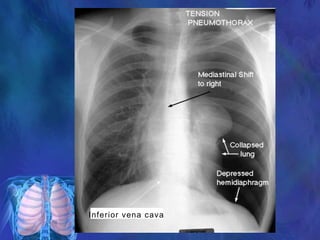
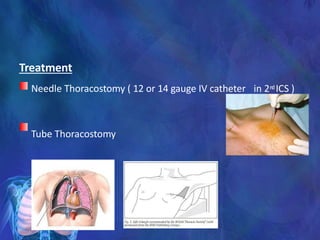
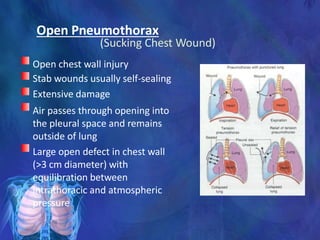
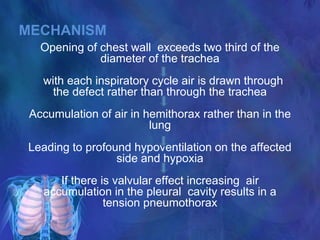
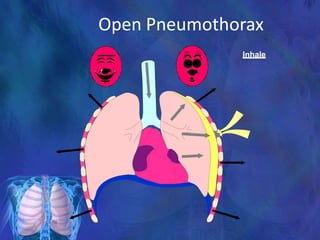
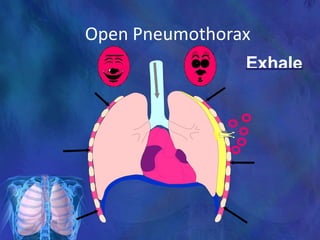
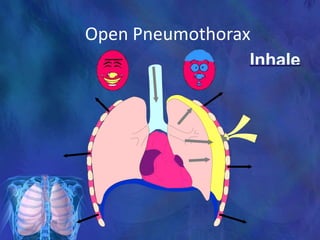
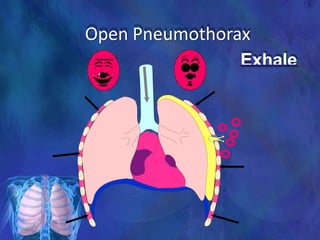
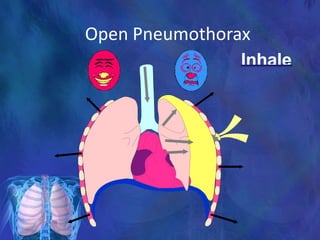
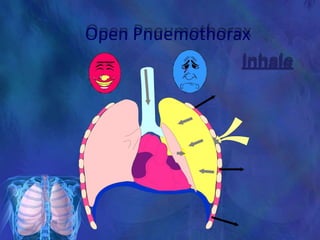
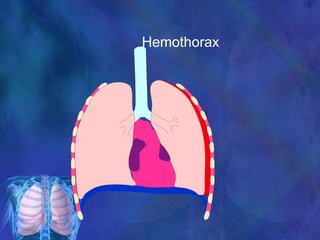
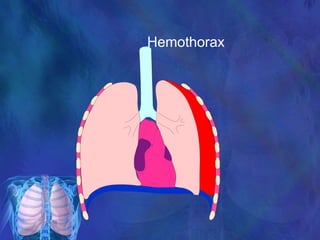
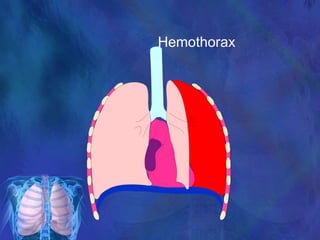
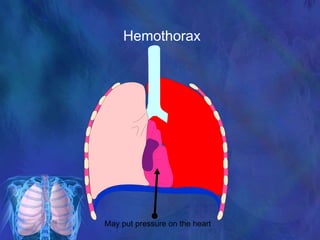
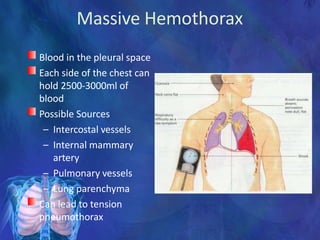
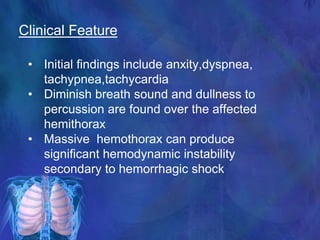
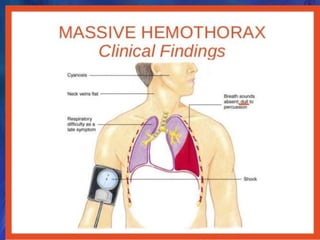
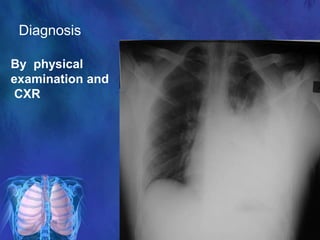
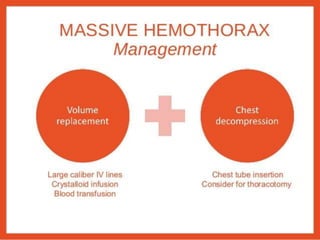
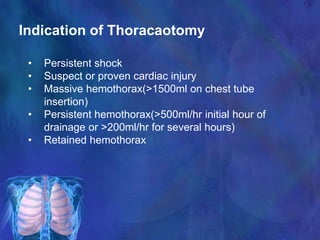
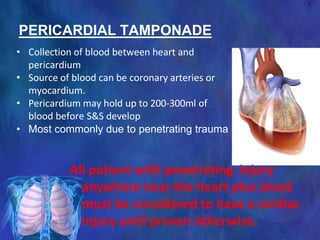
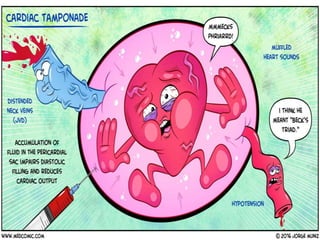
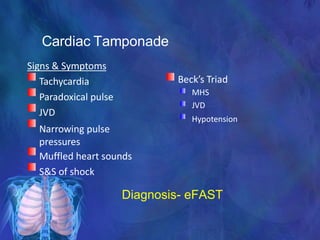
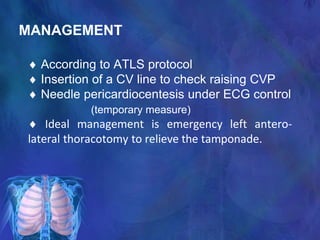
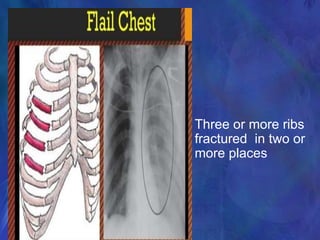
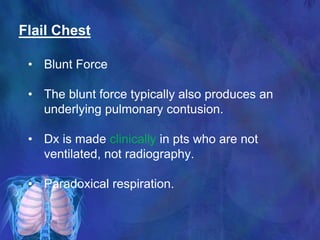
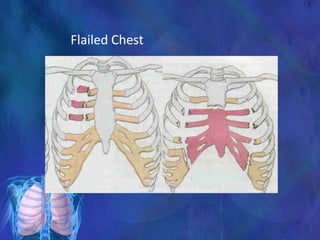
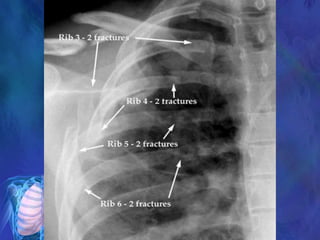
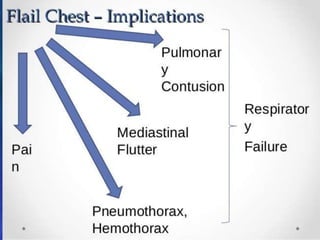
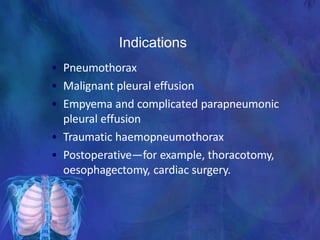
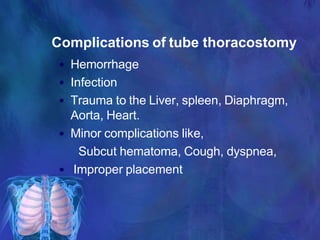
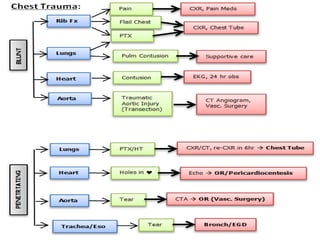
This document provides an overview of chest trauma and its management. It discusses that chest trauma accounts for 25% of all trauma deaths and is the second leading cause of trauma deaths after head injuries. It then covers the epidemiology, types, causes, pathophysiology and initial assessment of chest injuries. It describes important life-threatening injuries to assess for such as tension pneumothorax, massive hemothorax, flail chest and cardiac tamponade. It outlines the questions to ask and signs to look for when initially evaluating a patient with chest trauma. It also discusses monitoring the patient, management approaches, and complications to watch out for with chest trauma patients.