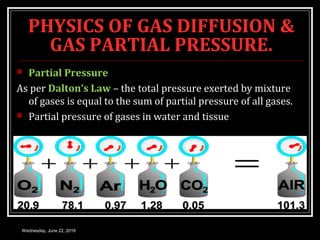
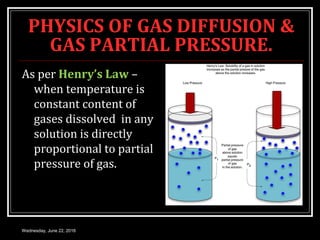
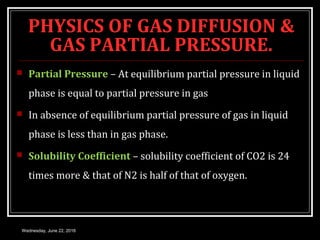
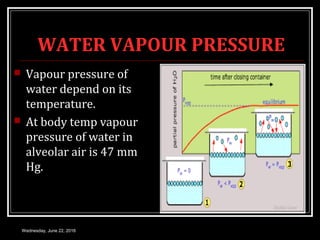
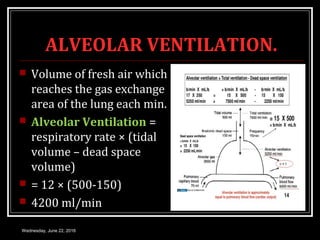
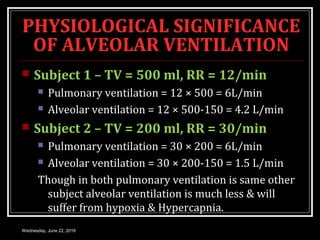
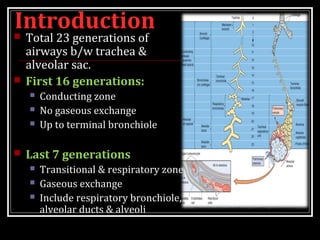
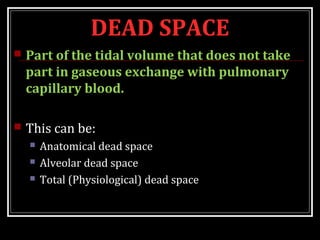
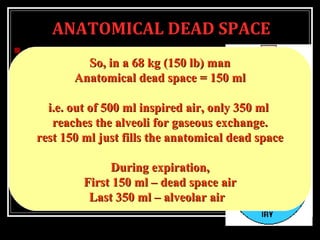
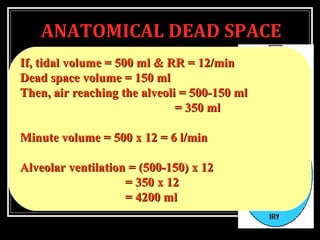
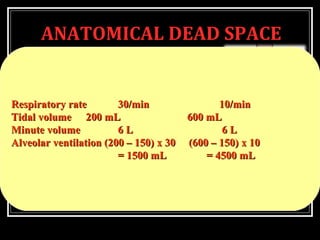
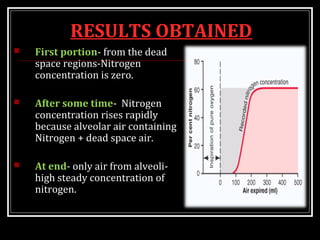
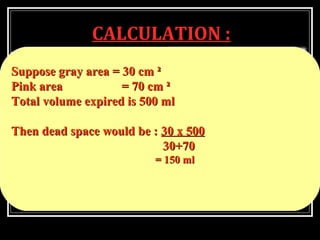
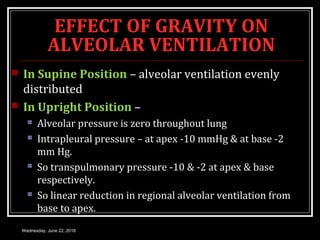
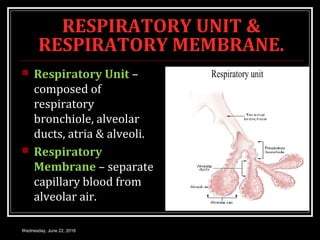
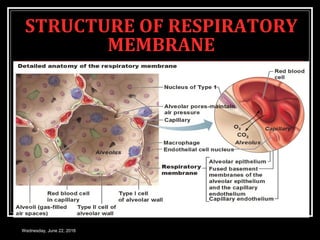
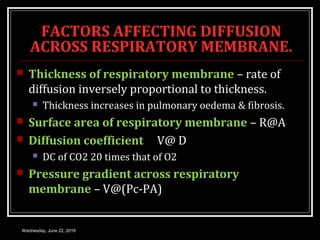
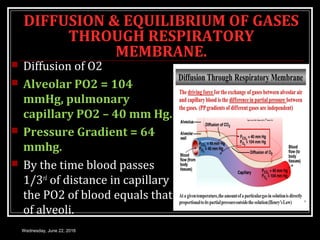
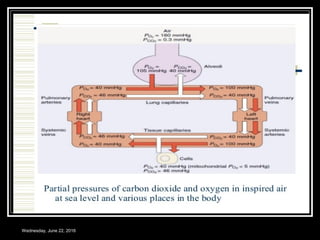
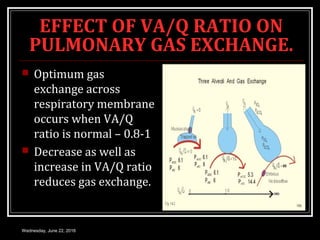
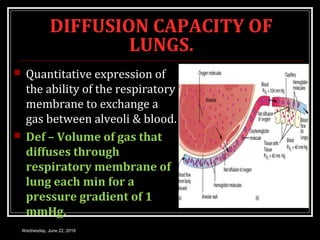
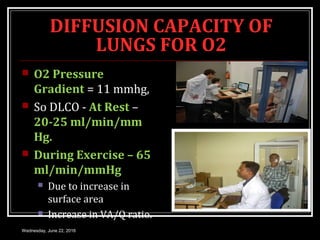
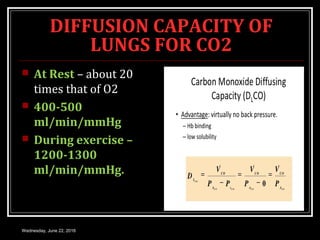
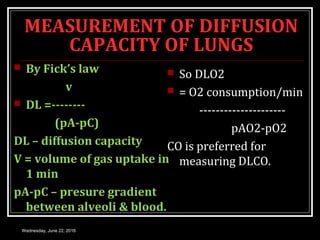
This document provides an overview of pulmonary diffusion and related concepts. It begins with objectives around gas diffusion, alveolar ventilation, and the ventilation-perfusion ratio. The introduction discusses external respiration, pulmonary ventilation, diffusion, and gas transport. Key topics covered include the physics of gas diffusion and partial pressure, alveolar ventilation, dead space, and the diffusion of gases through the respiratory membrane. Clinical significance of various concepts is also discussed.