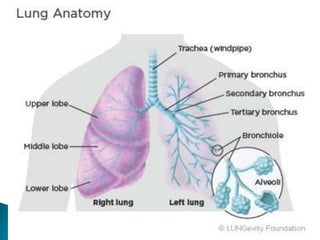
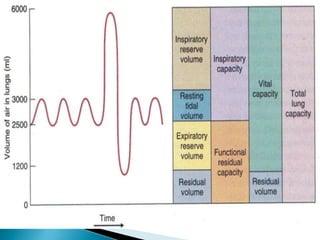
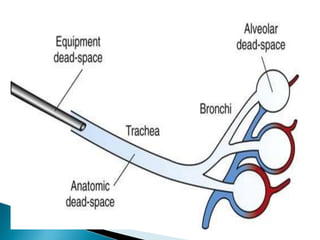
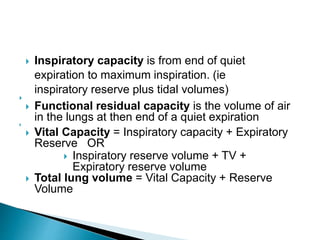
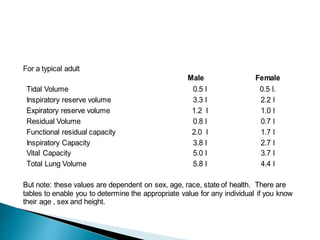
This document defines key terms related to gas exchange and ventilation in the lungs. It discusses functional residual capacity, residual volume, vital capacity, and inspiratory capacity. It defines serial and physiological dead space and how they are measured. It describes how to calculate alveolar ventilation rate given pulmonary ventilation rate, dead space volume, and respiratory rate. It explains the processes of ventilation, perfusion, and the ventilation/perfusion ratio in the lungs.