This document provides an overview of pulmonary circulation. It discusses:
1) The functional anatomy of the three circulations in the lungs - pulmonary, bronchial, and lymphatic.
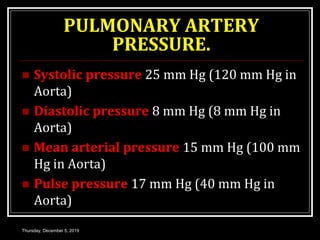
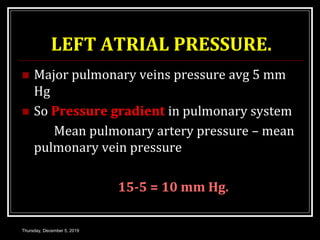
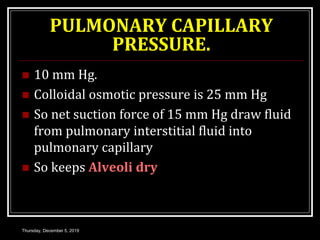
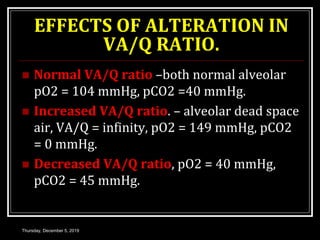
2) The characteristic features of pulmonary circulation including its low pressure, resistance, and high capacitance.
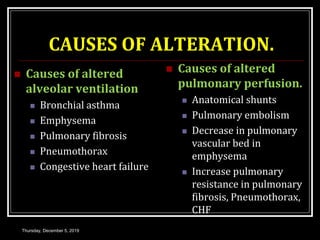
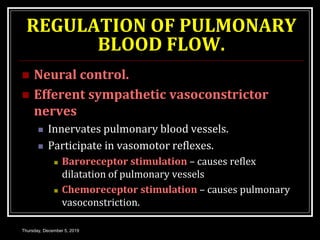
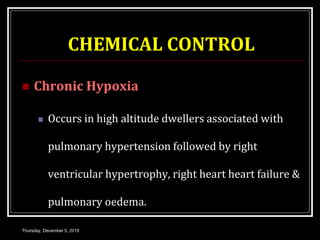
3) The regulation of pulmonary blood flow through neural and chemical control mechanisms like hypoxia and hypercapnia.
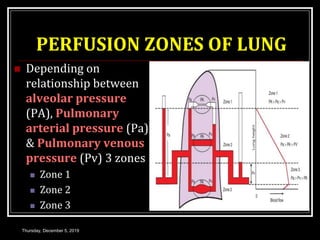
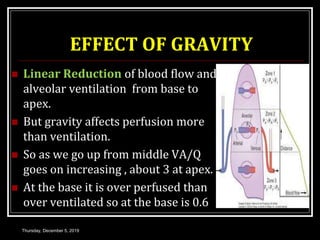
4) How factors like gravity and exercise can impact regional pulmonary blood flow and alveolar ventilation.