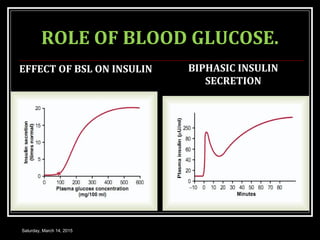
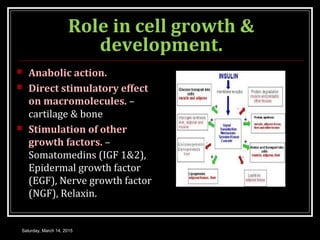
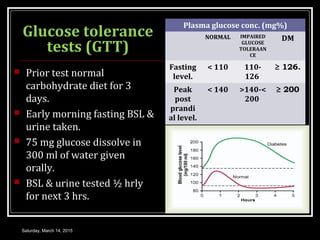
This document provides information about insulin, including its structure, biosynthesis, secretion, regulation, mechanisms of action, and role in conditions like diabetes mellitus. It discusses how insulin is synthesized and secreted by beta cells in the pancreas in response to blood glucose levels. Insulin acts to lower blood glucose and promote uptake and storage of glucose in liver, muscle and fat tissues. Diabetes results from insufficient insulin secretion or action leading to hyperglycemia.