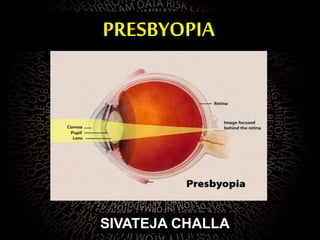
Presbyopia is the loss of eye's ability to focus on near objects with age due to a hardening of the lens. It typically begins around age 40-45 when the eye's natural lens loses elasticity. Symptoms include difficulty seeing objects close up, which is worse in low light. Presbyopia is treated with reading glasses, bifocals, or progressive lenses to add magnification for near vision. Multifocal contact lenses and refractive surgery are also options. The condition is normal and inevitable with aging and affects over 1 billion people worldwide.