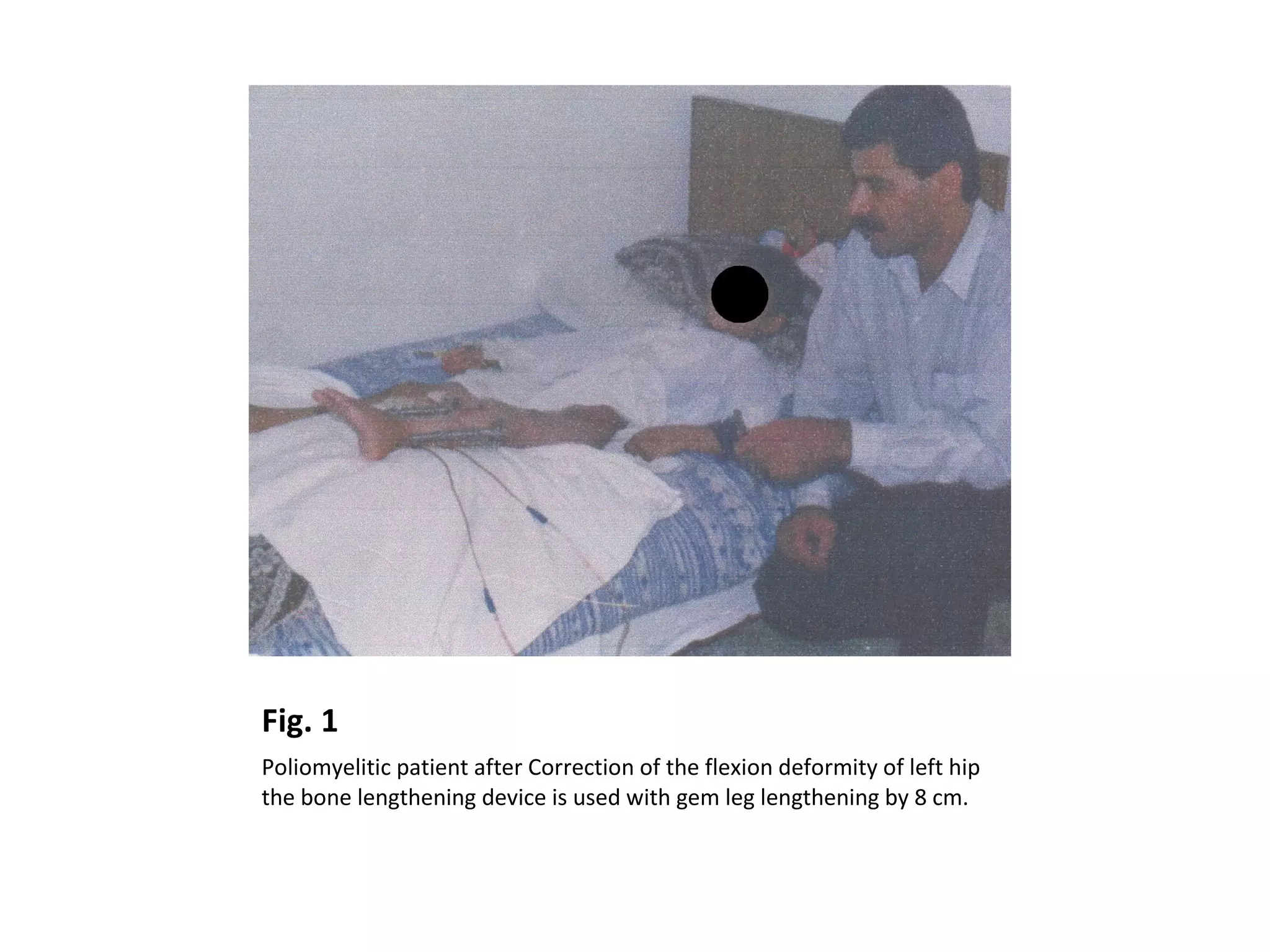
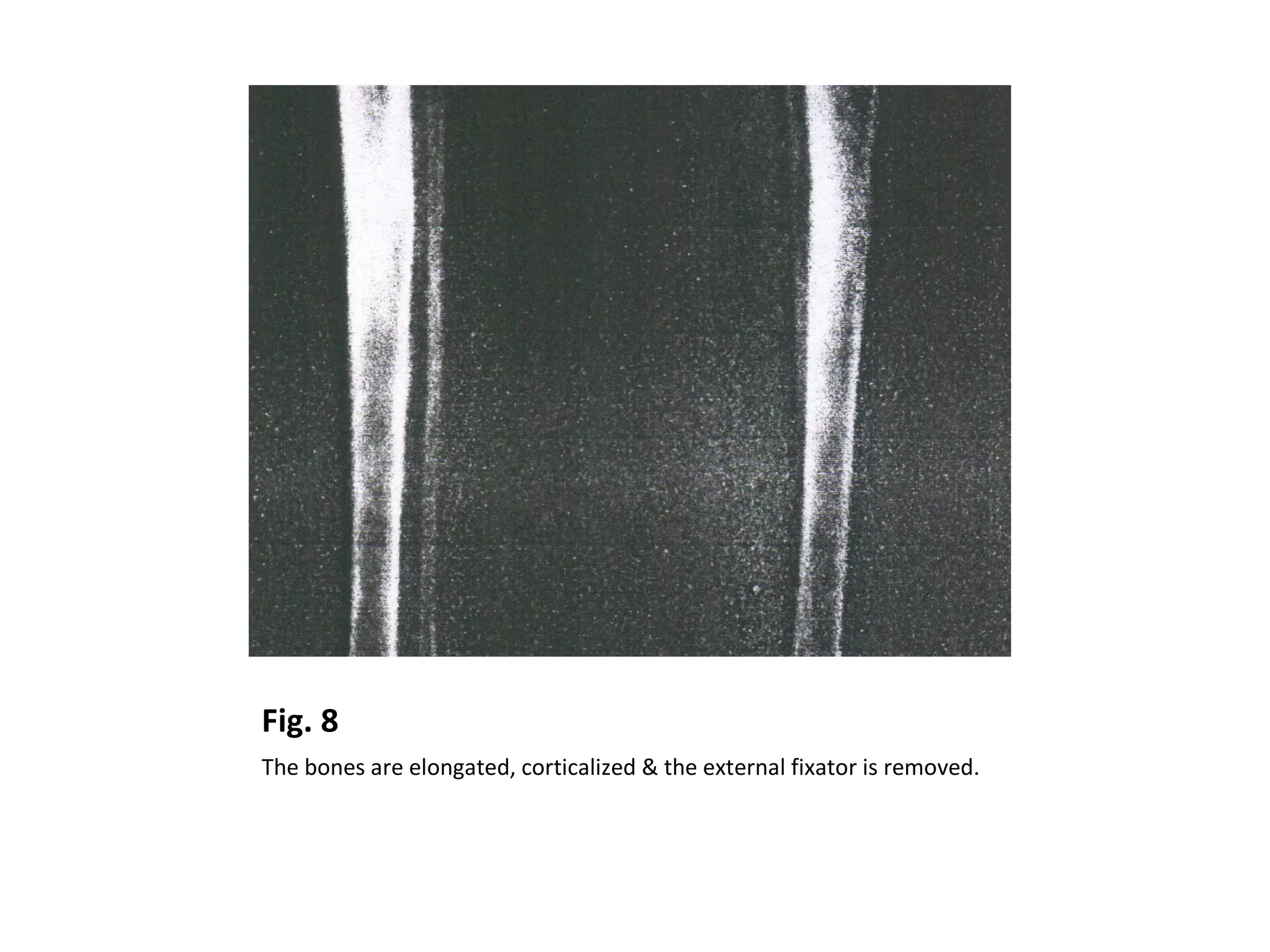
Limb length discrepancy can cause both cosmetic and functional issues such as an awkward gait and increased energy expenditure. It is commonly caused by trauma, infections, tumors, or conditions like polio or cerebral palsy that affect bone growth asymmetry. Treatment options include shoe lifts for small discrepancies (under 2.5 cm), halting further growth in the longer limb via epiphysiodesis, shortening the long leg, or lengthening the short leg. Limb lengthening techniques have advanced from early methods using nails or plates to more modern circular external fixators allowing gradual lengthening over months. Complications can include pin infections, need for additional surgery, and stiffness, but with optimal stabilization, new bone forms through