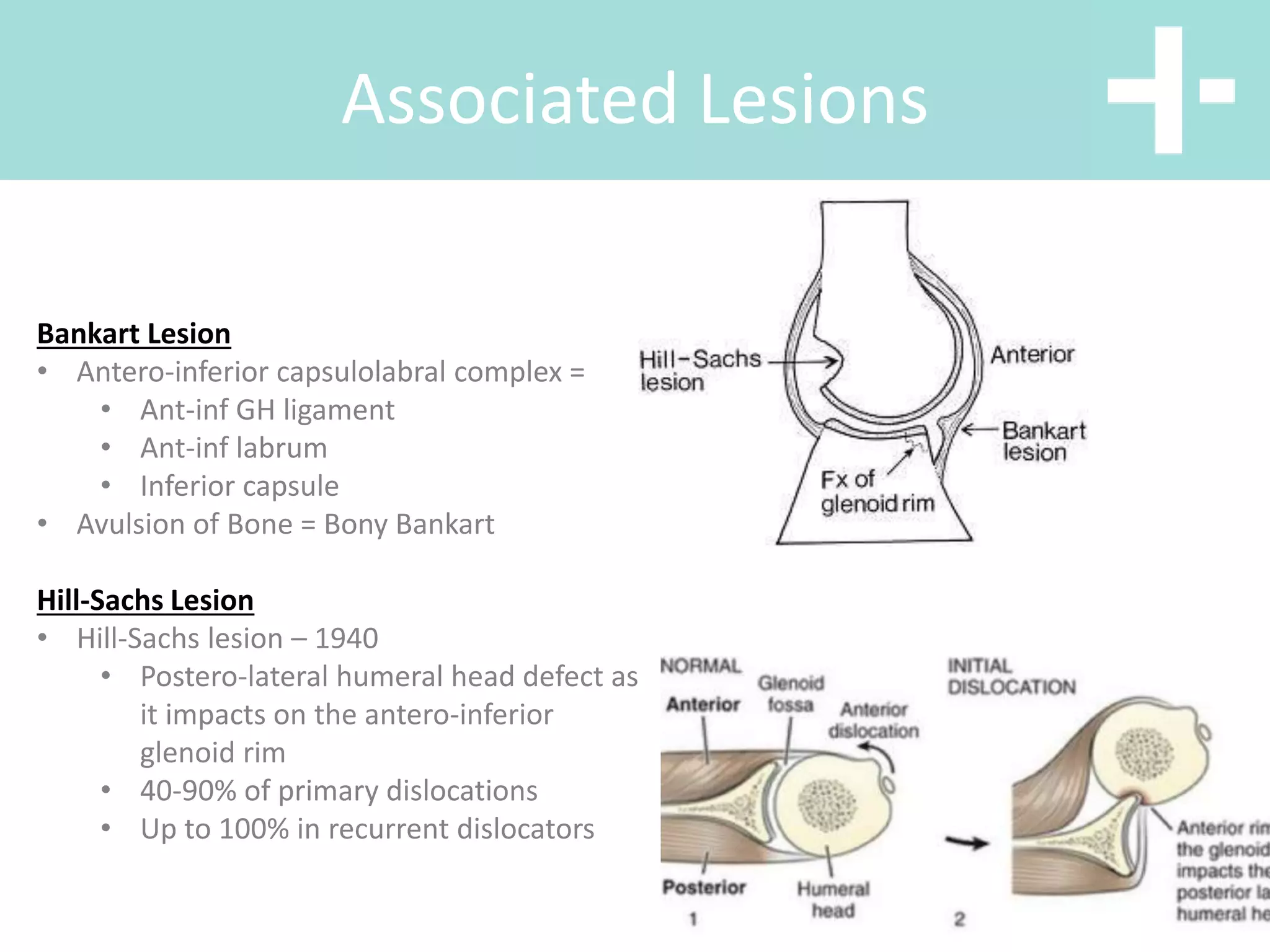
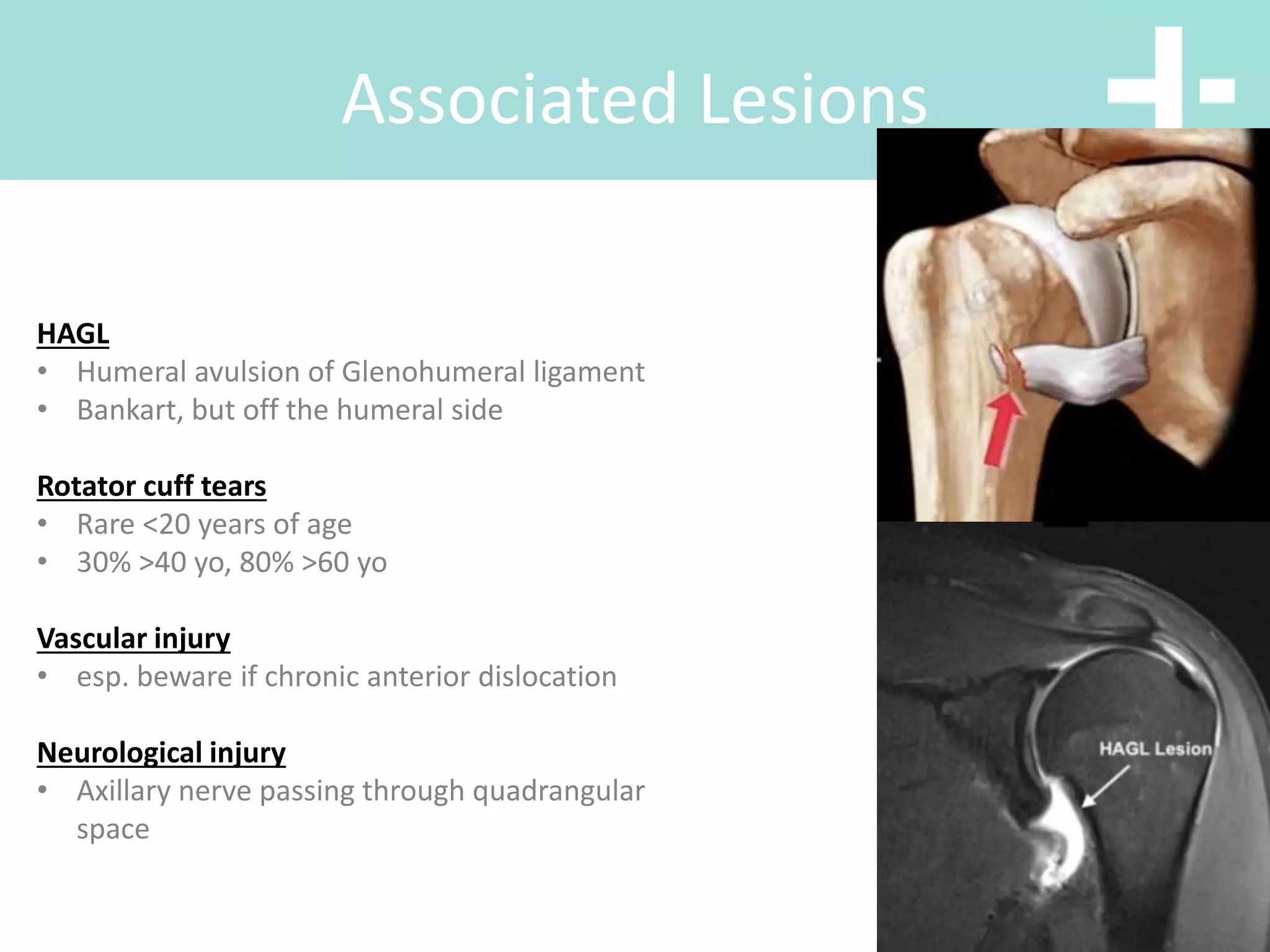
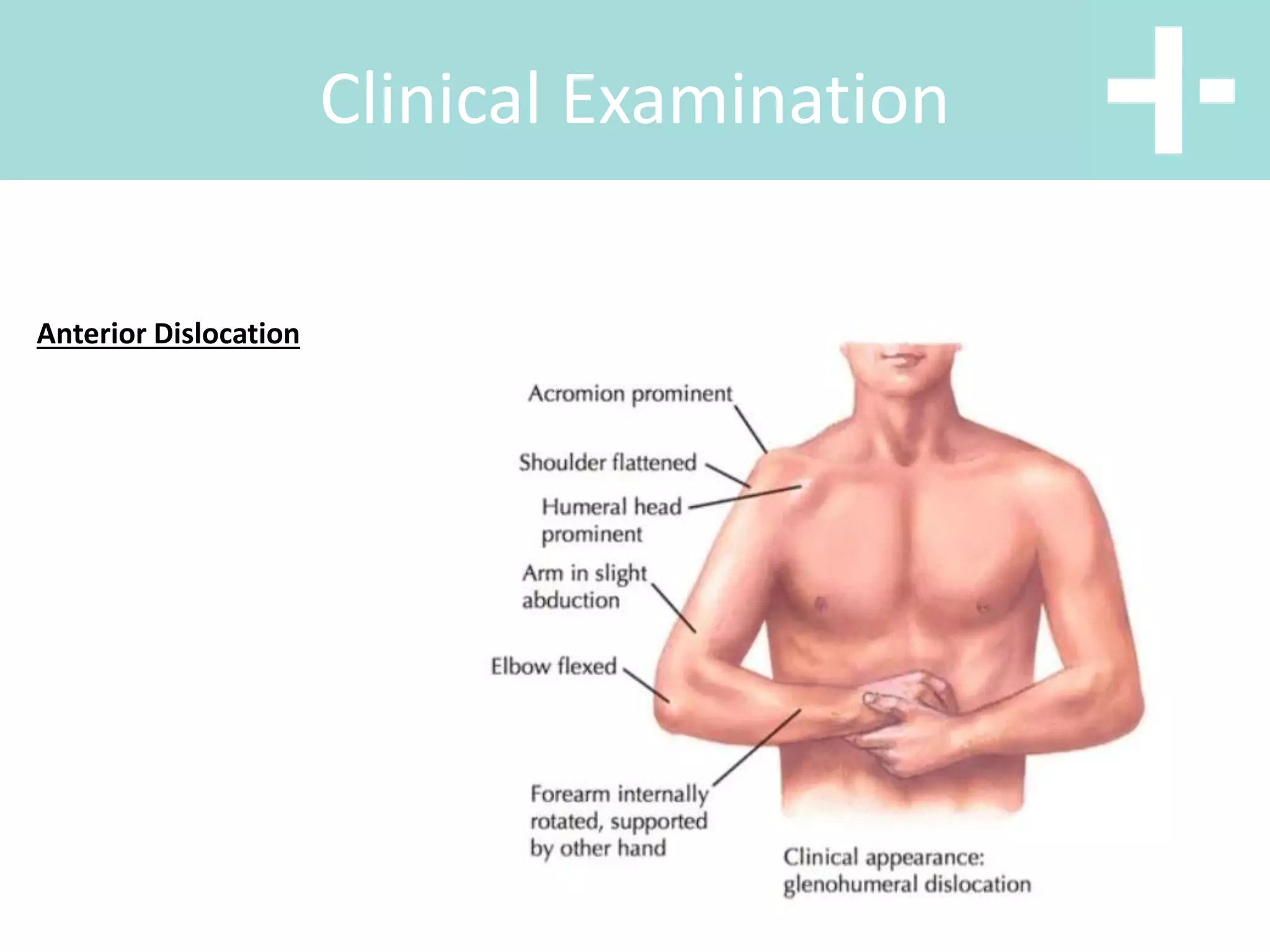
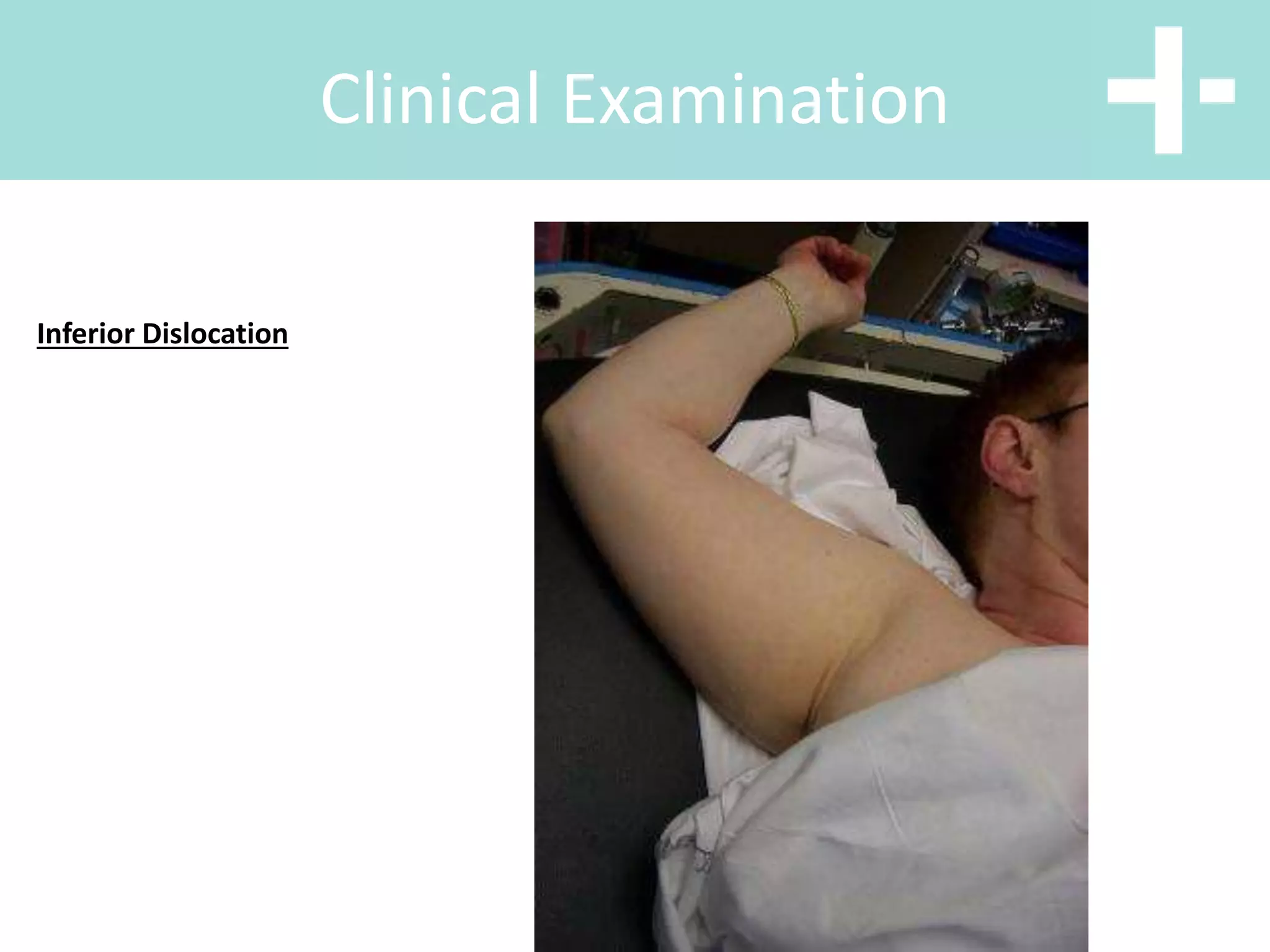
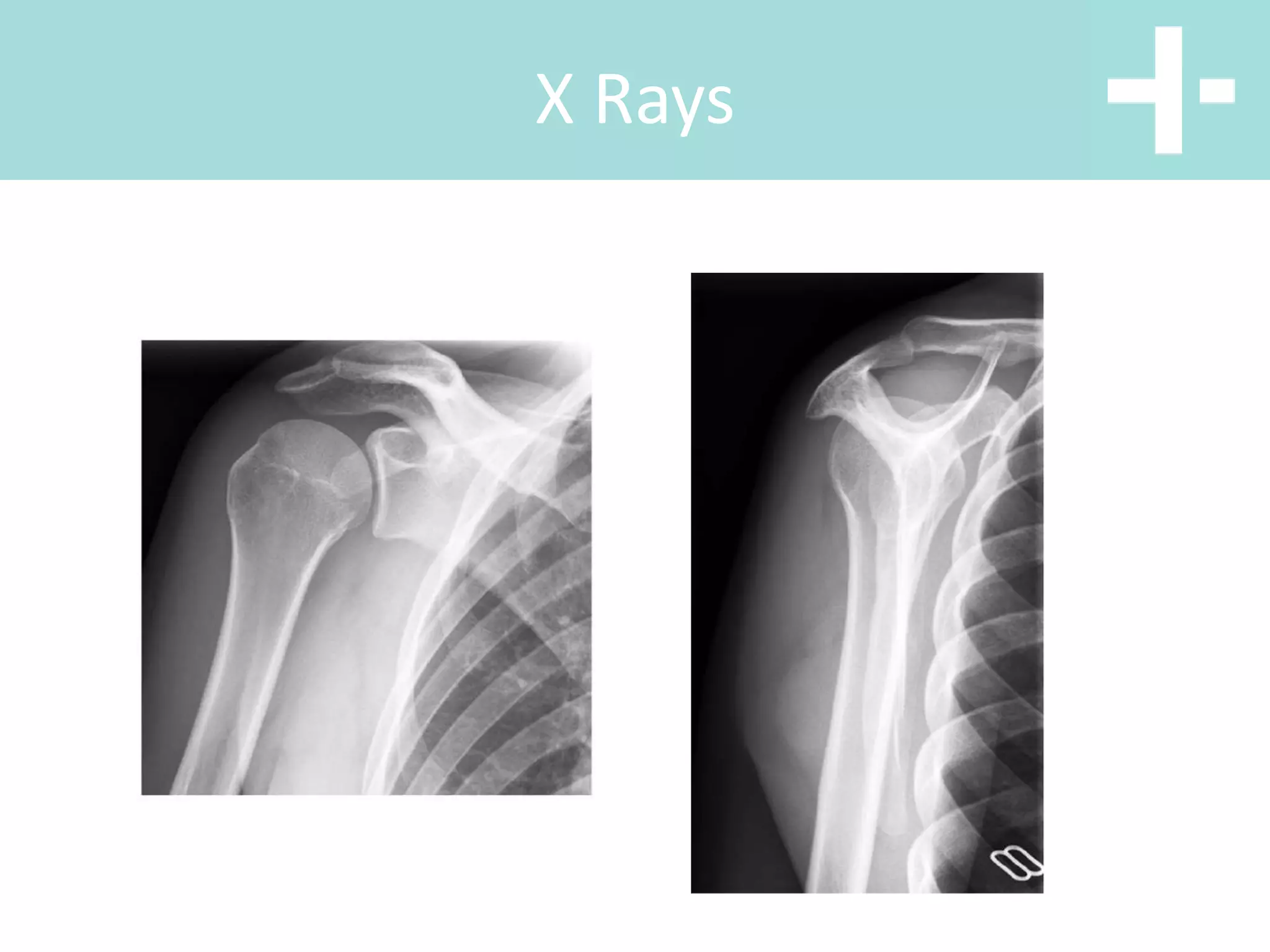
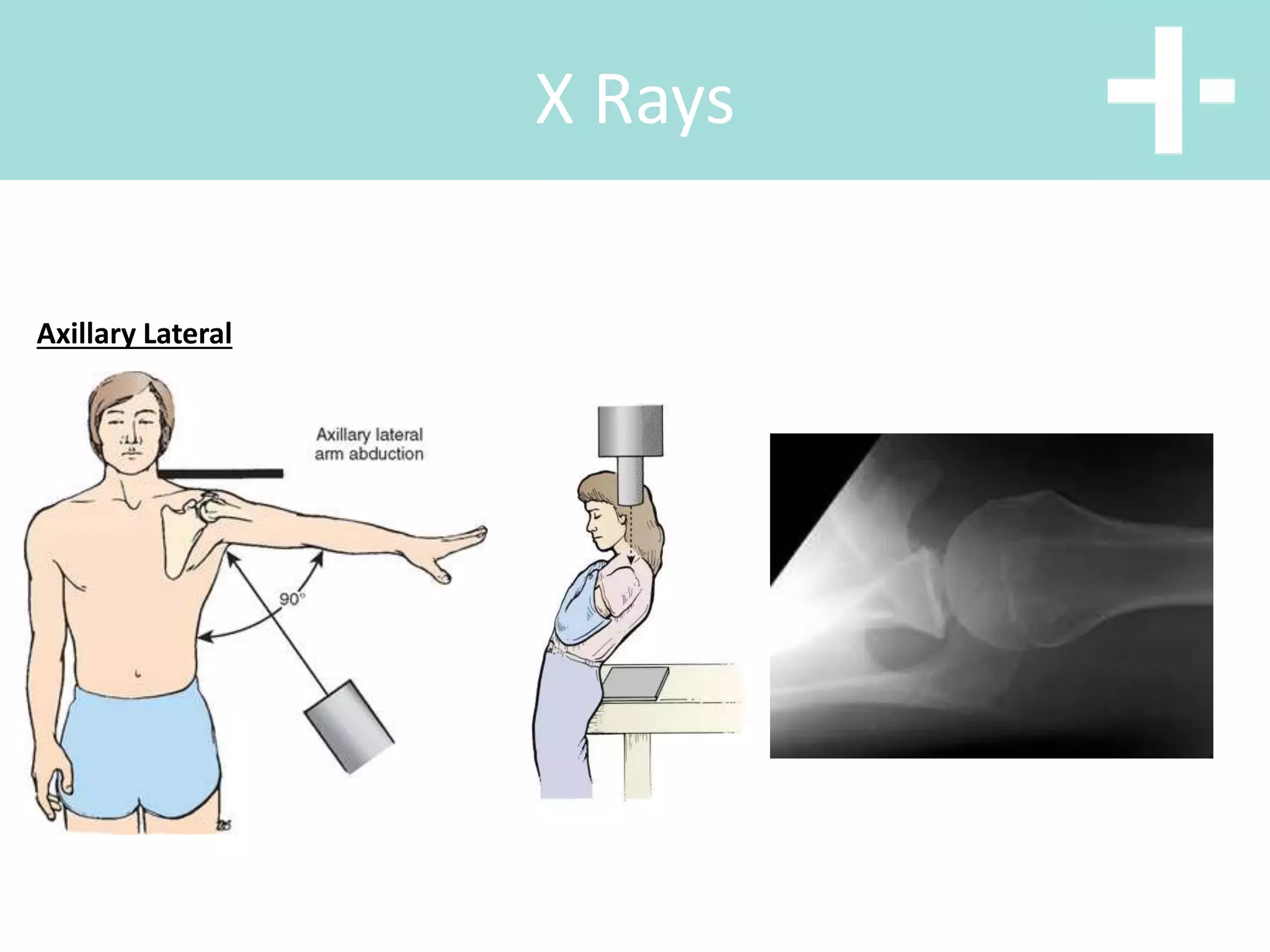
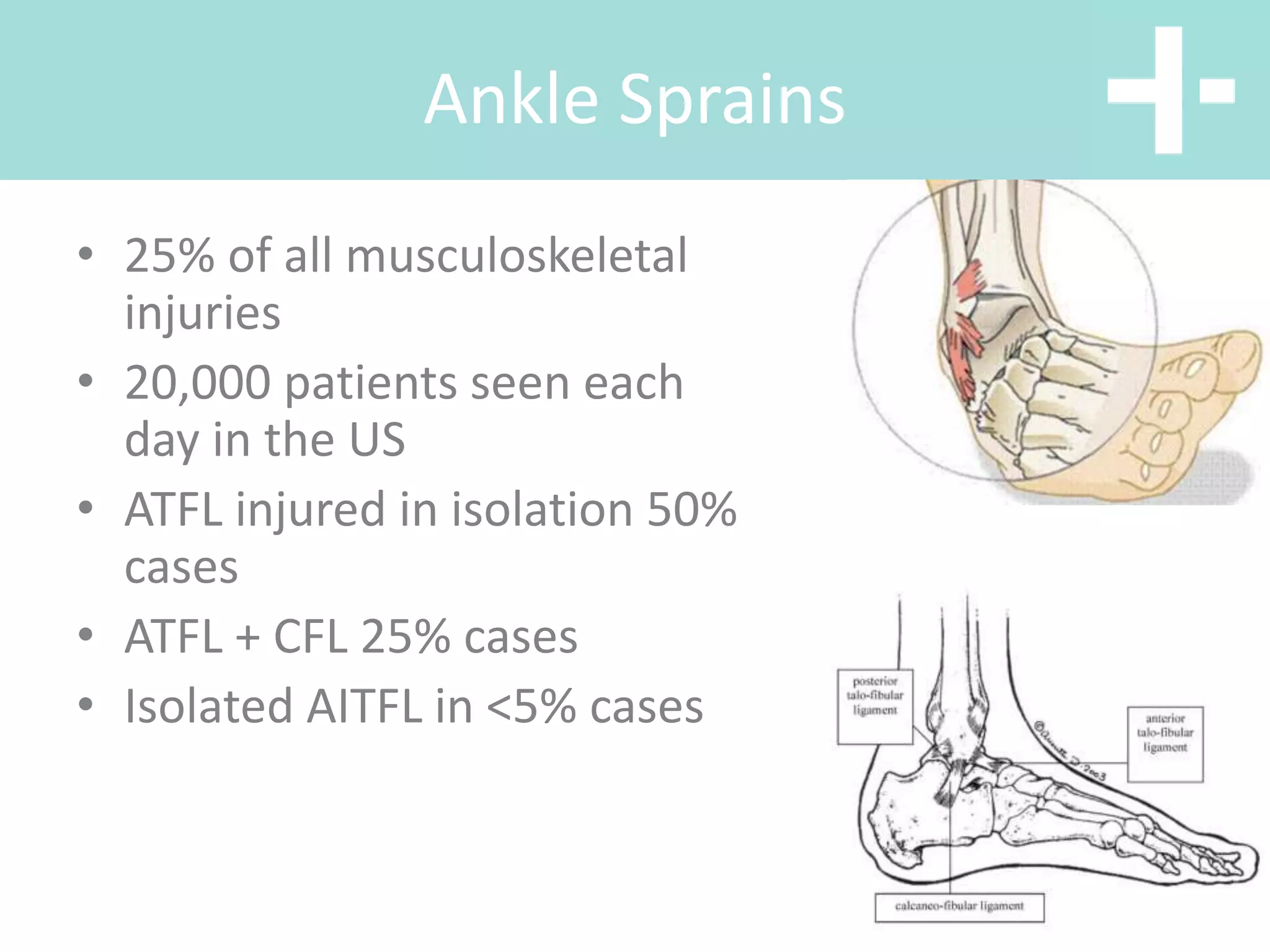
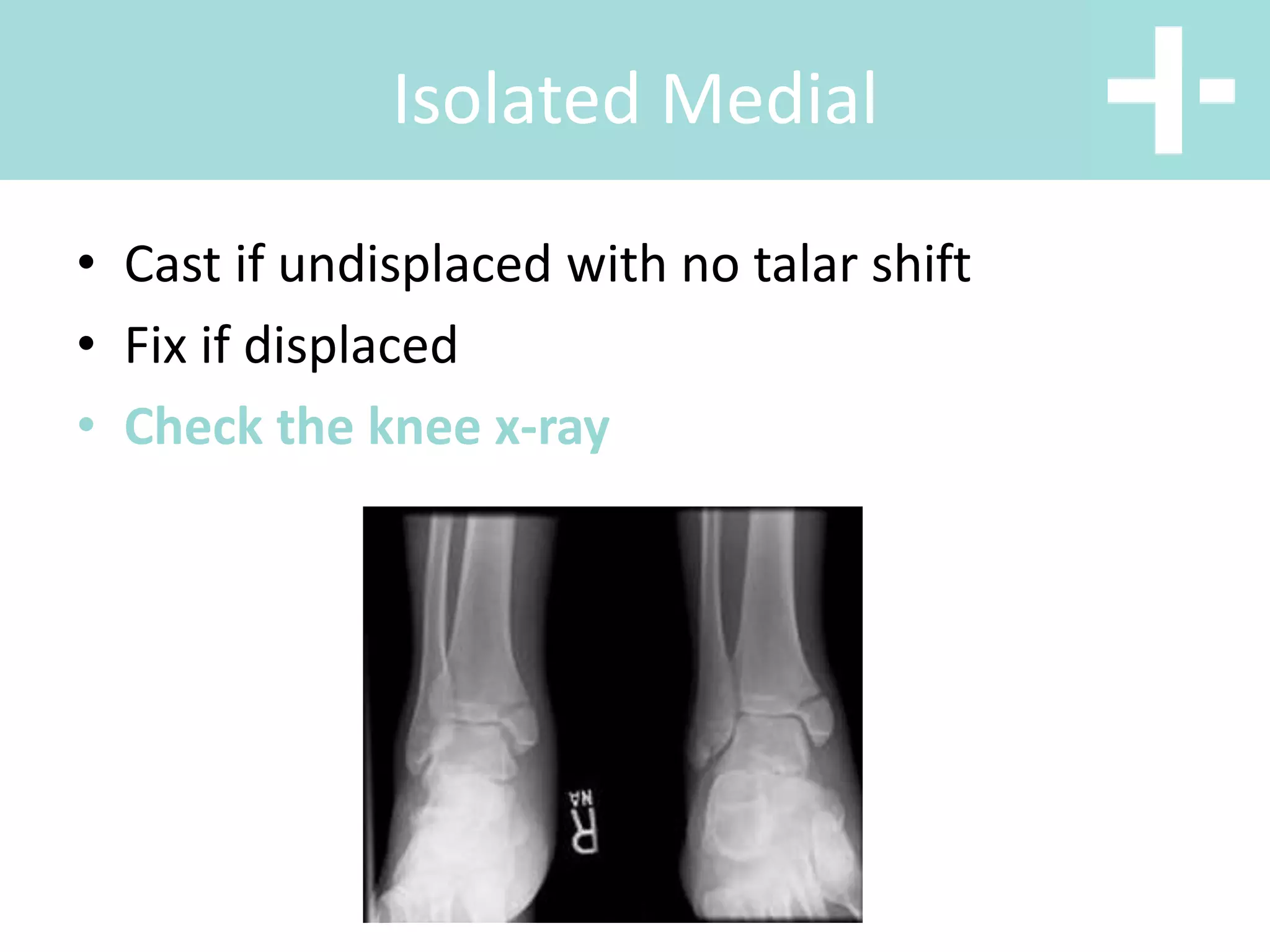
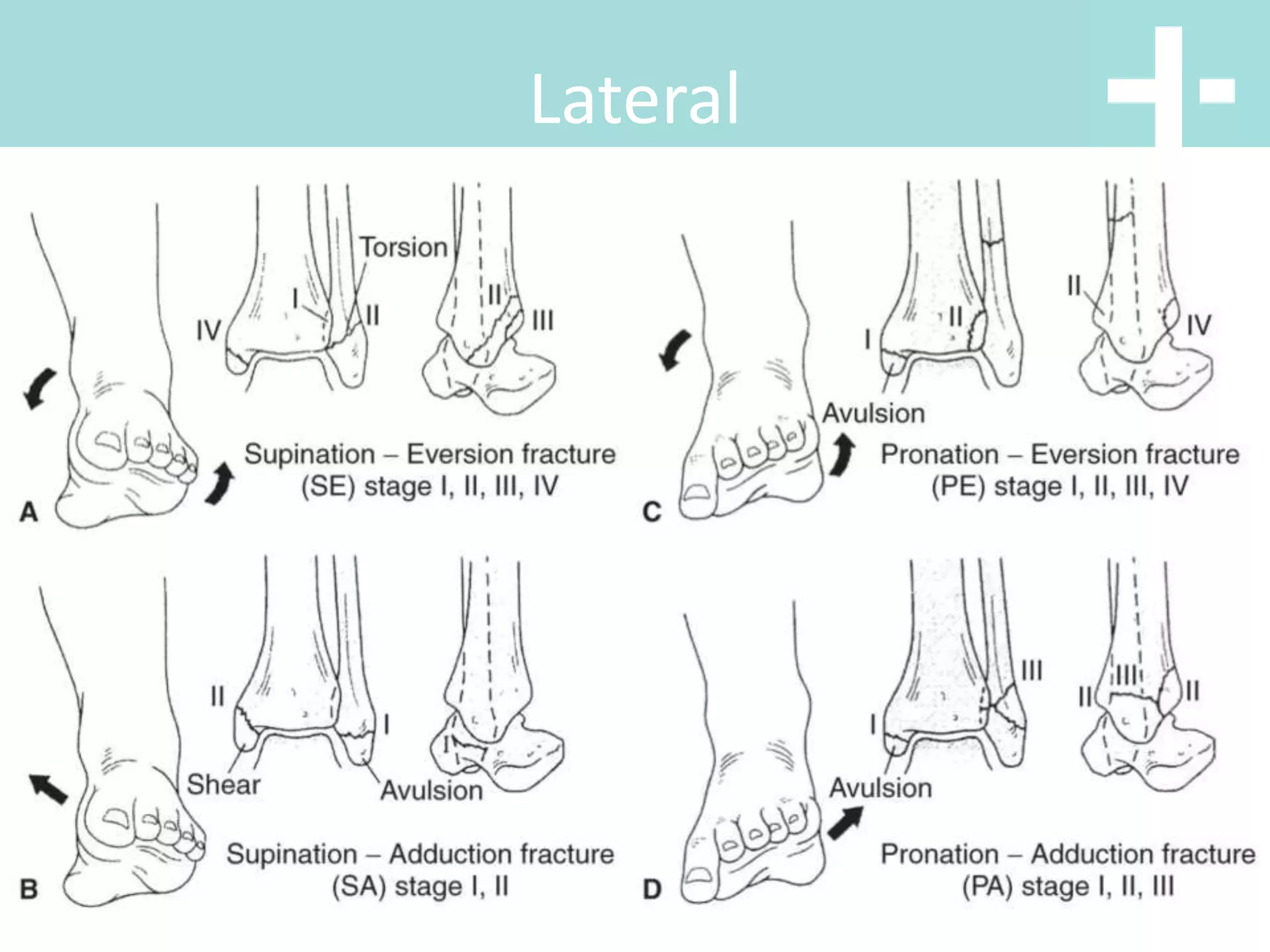
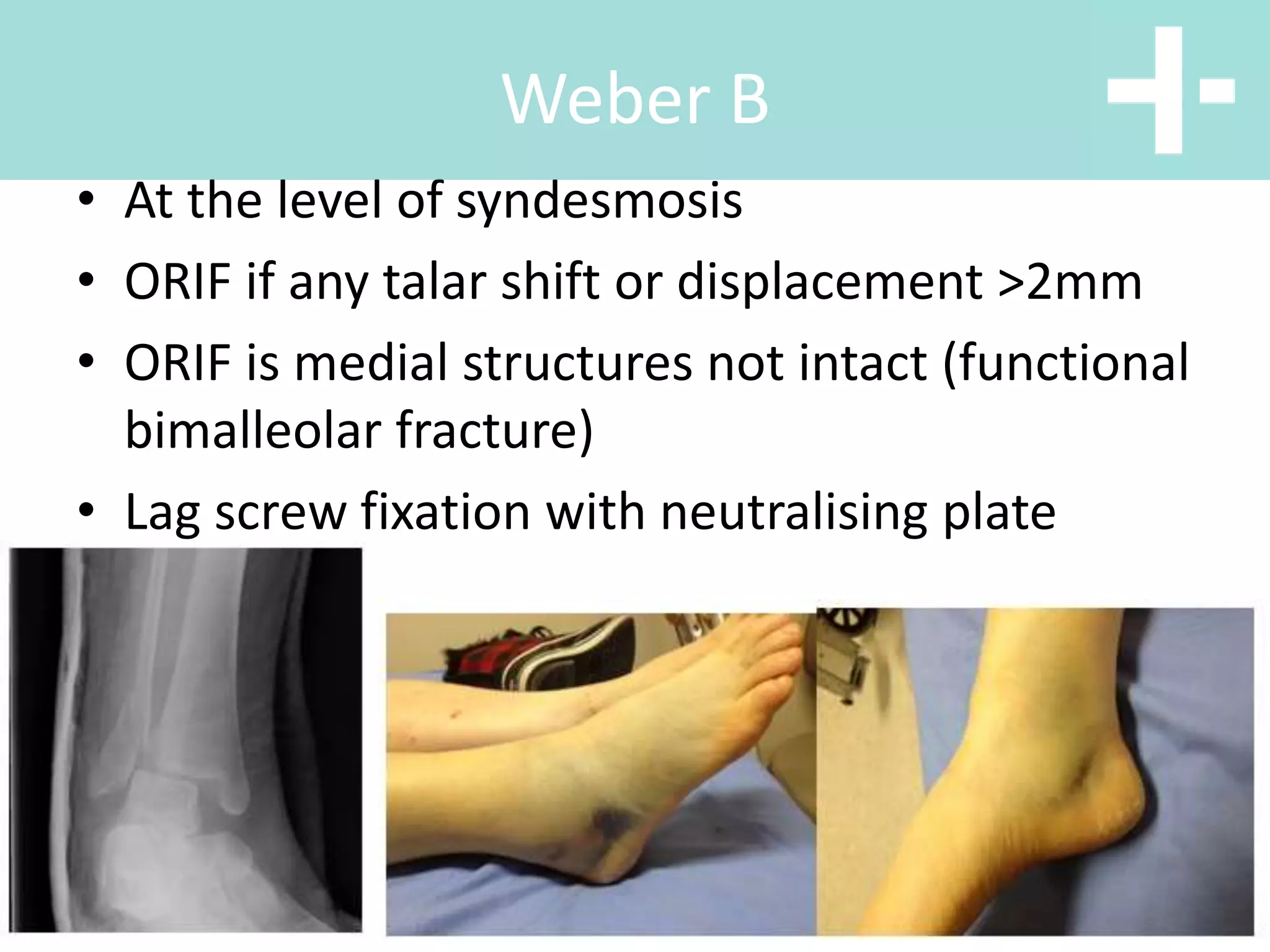
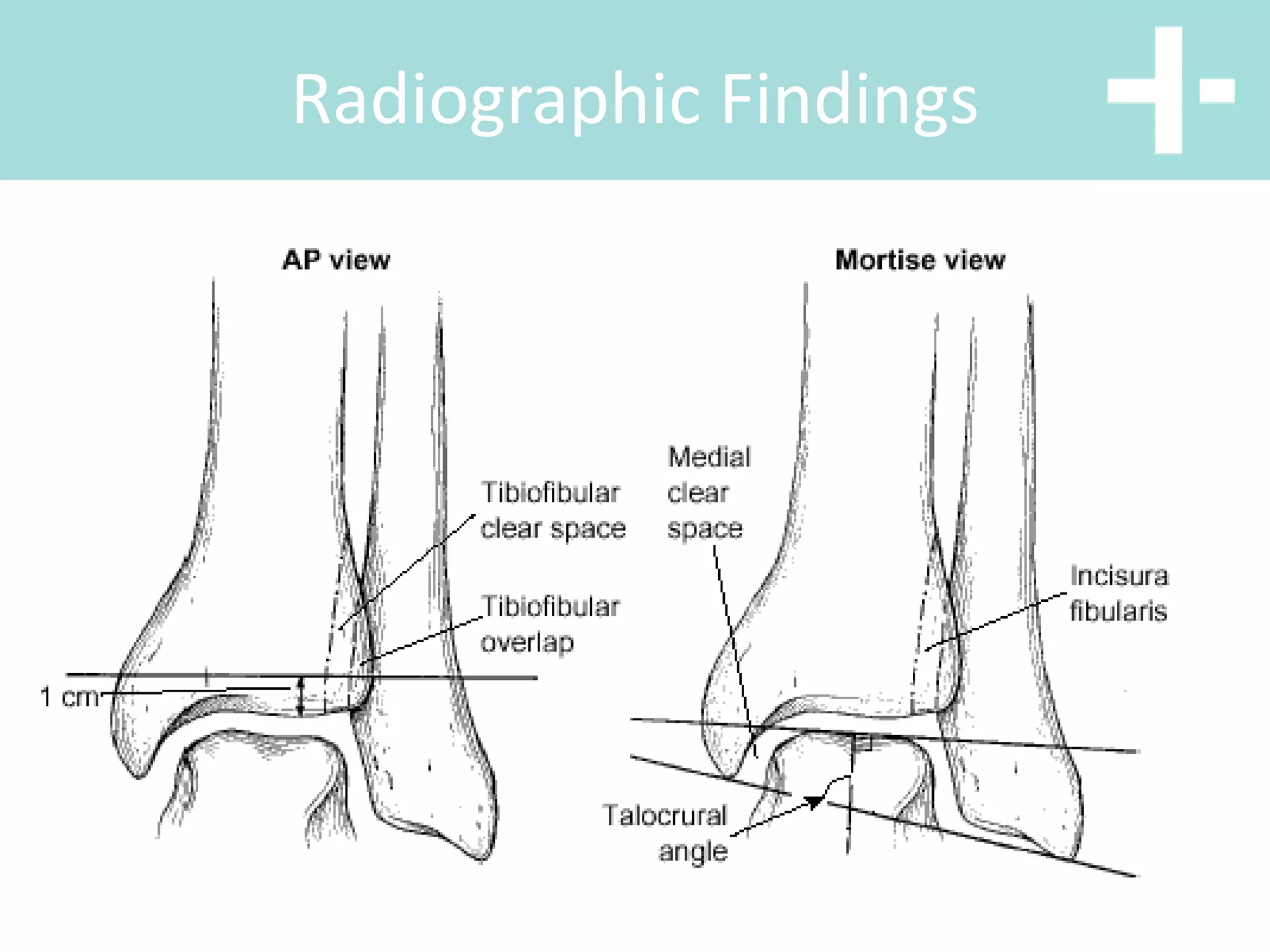
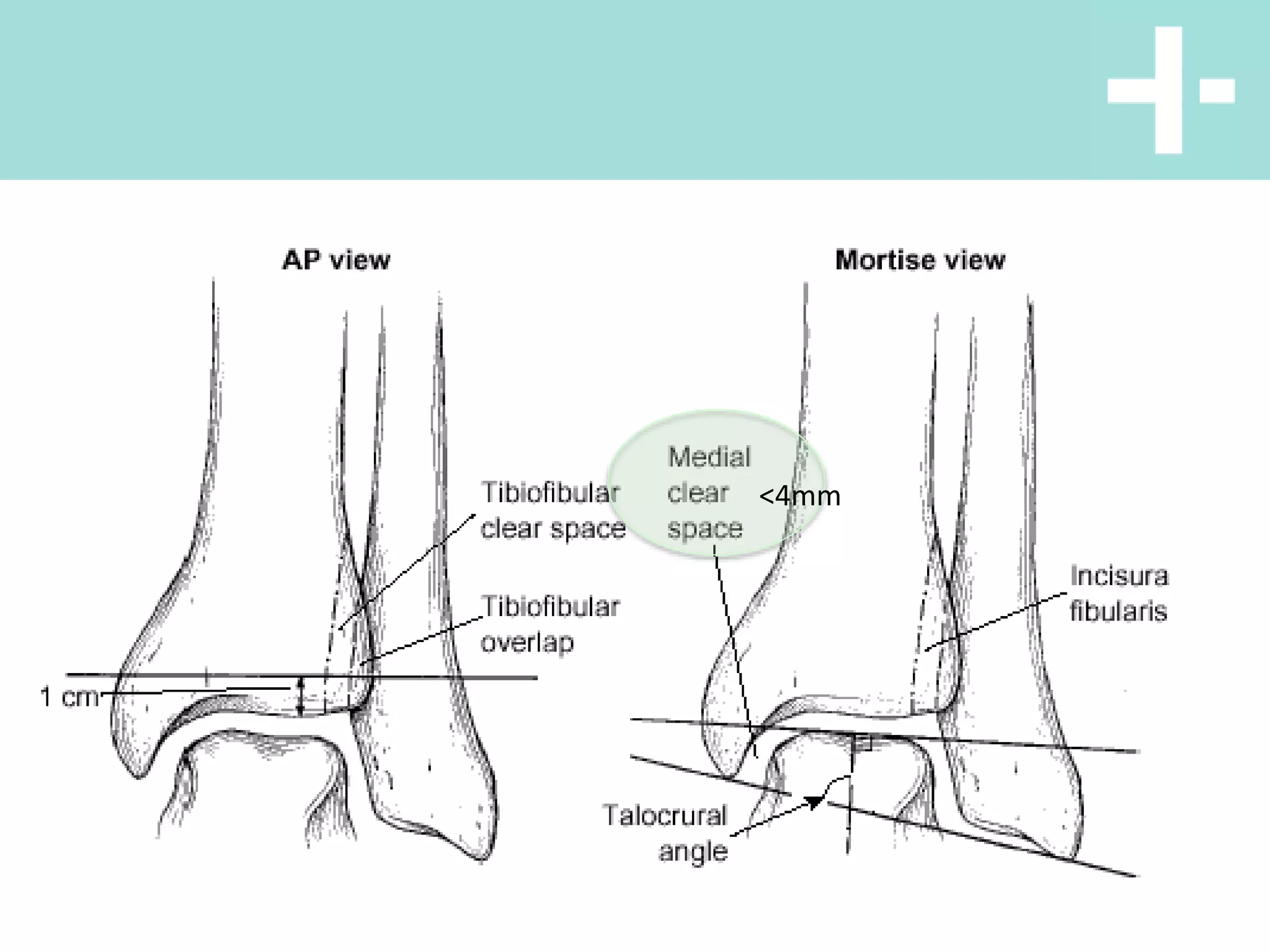
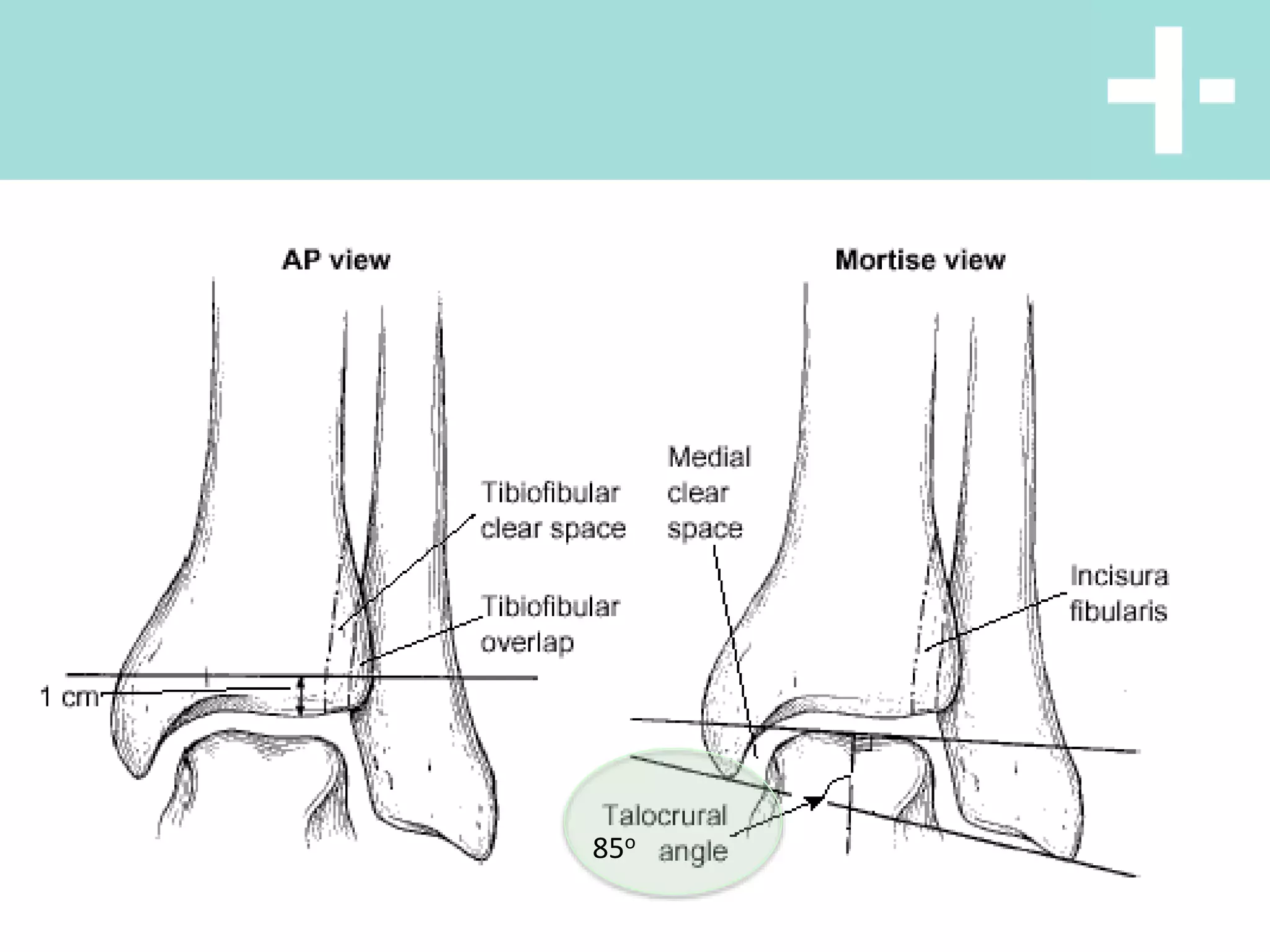
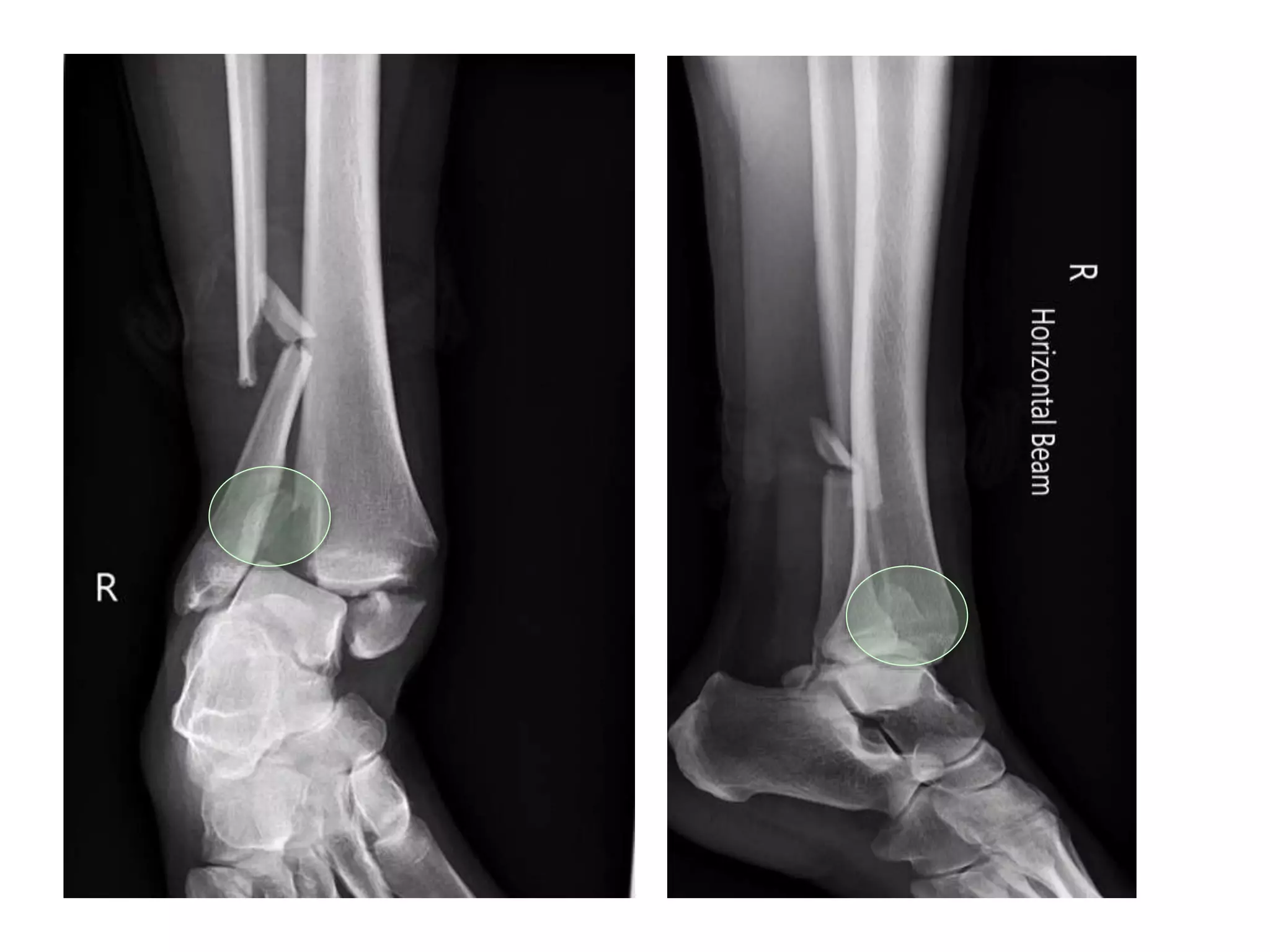
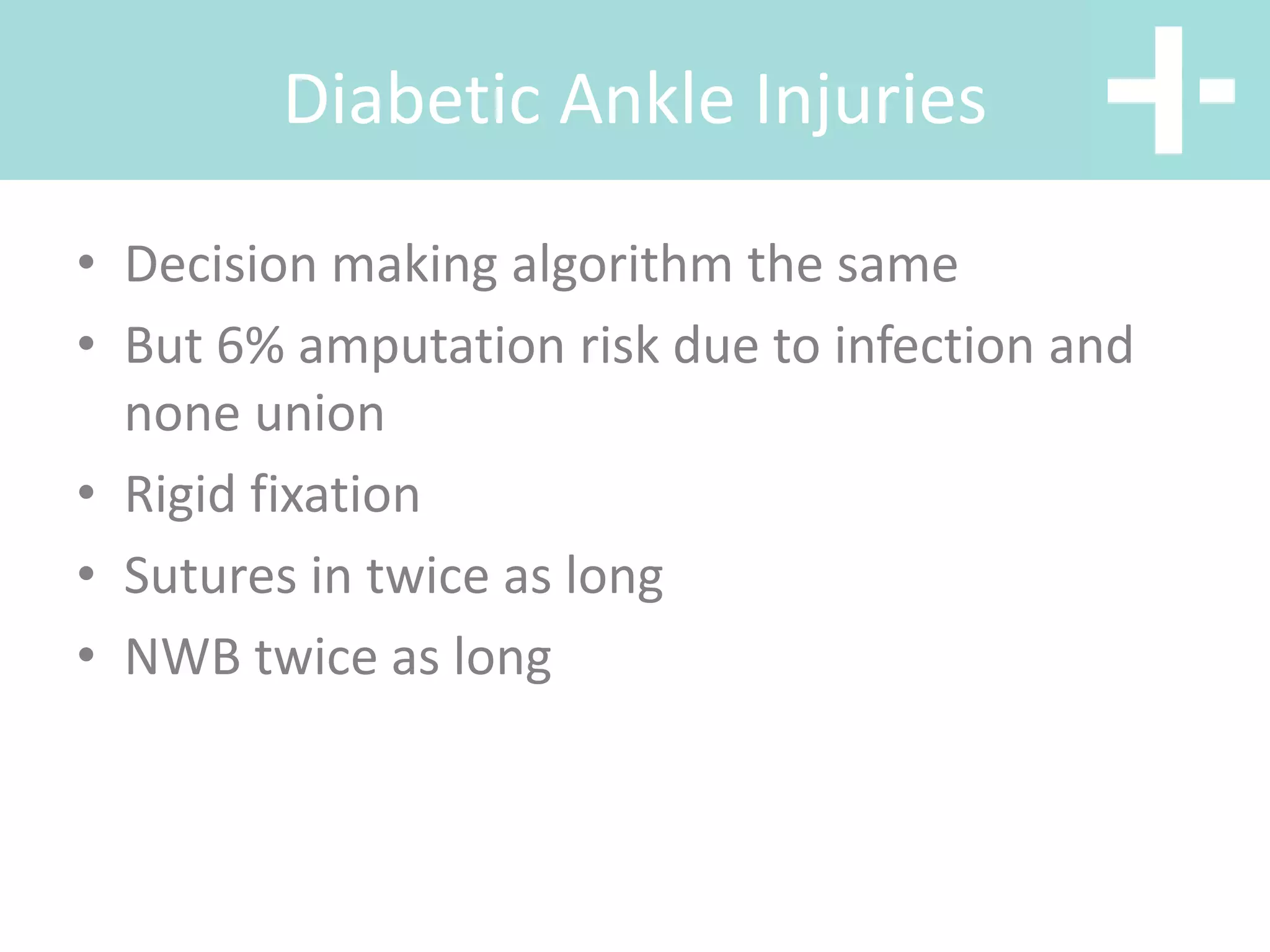
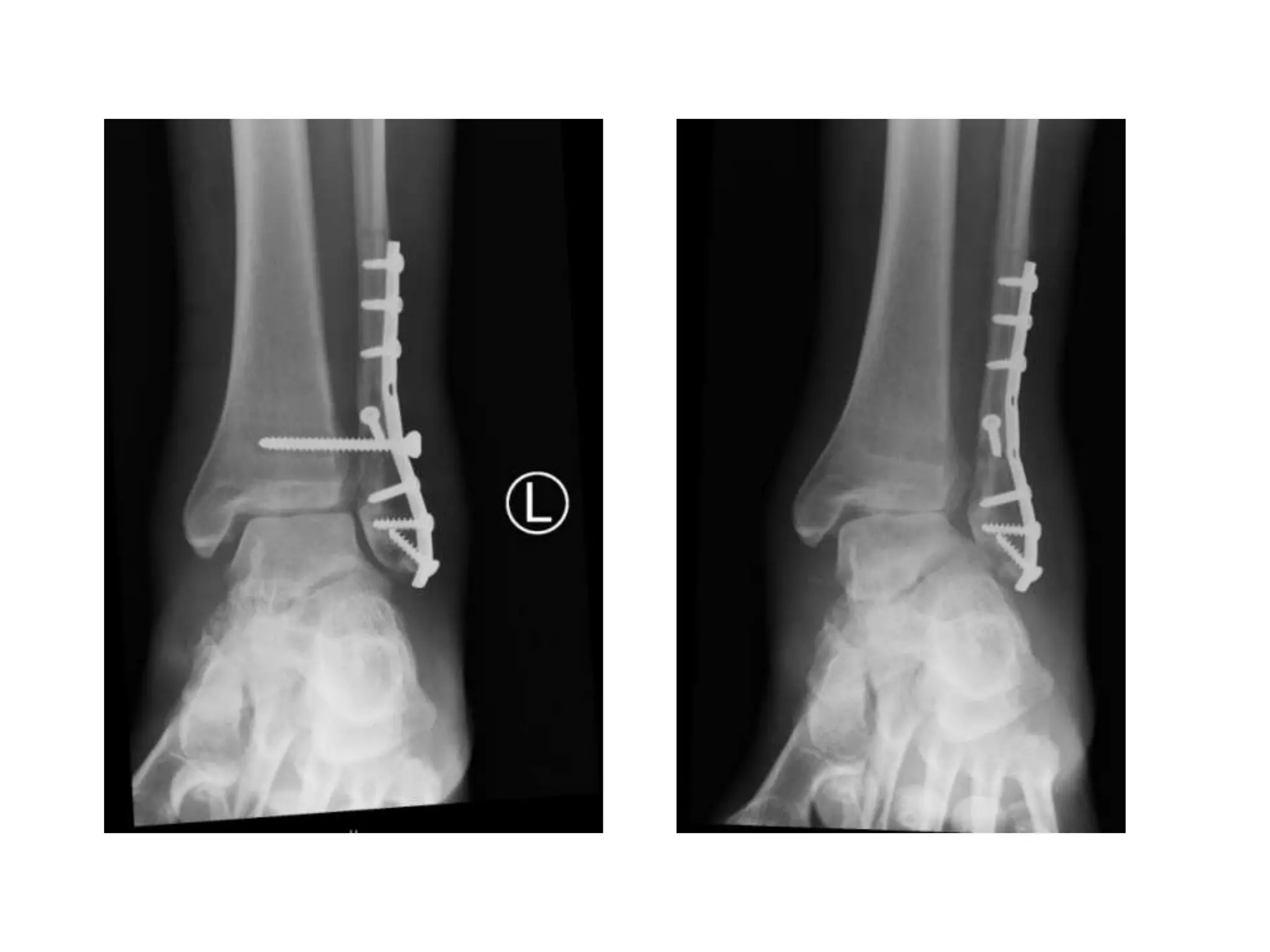
This document discusses shoulder and ankle injuries. Regarding shoulders, it describes the anatomy and stabilizers of the shoulder joint. It discusses classifications for shoulder instability and common associated lesions like Bankart and Hill-Sachs lesions. For ankles, it outlines the prevalence and classifications of ankle sprains and fractures. It provides guidance on clinical examination, imaging and management considerations for various ankle injuries.