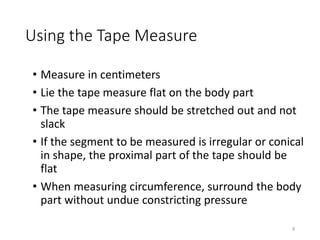
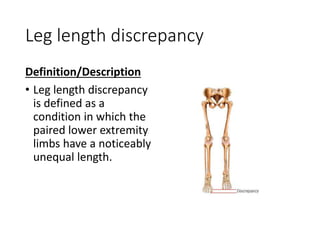
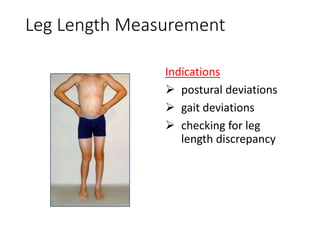
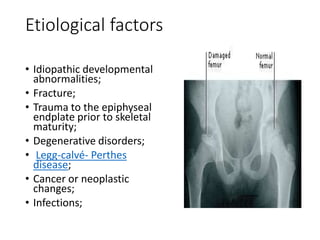
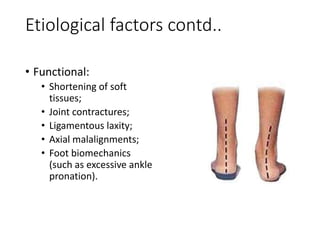
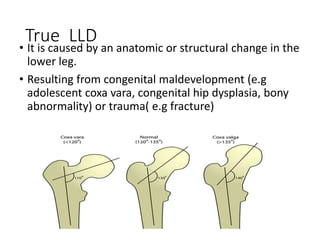
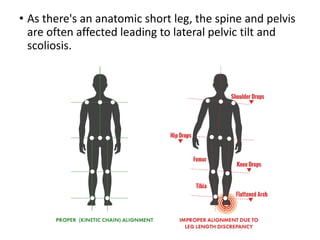
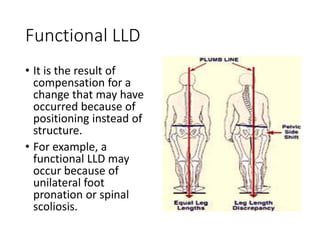
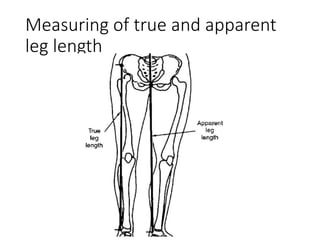
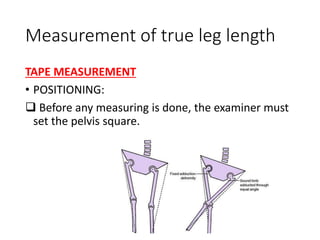
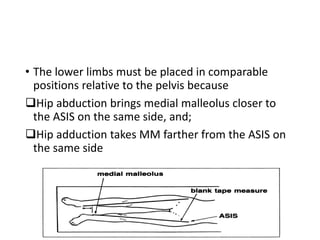
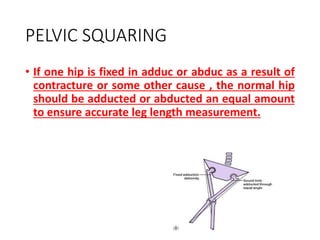
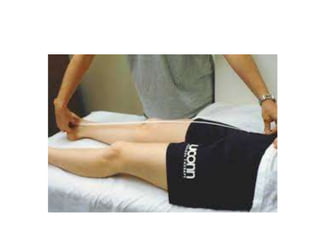
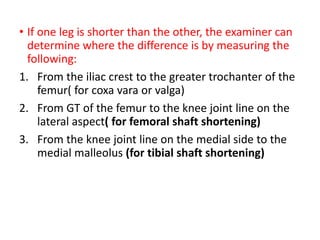
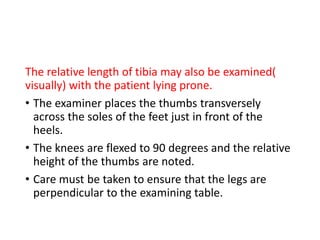
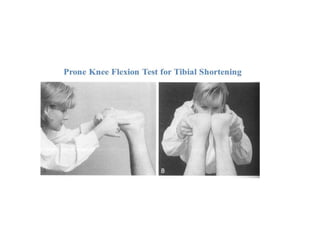
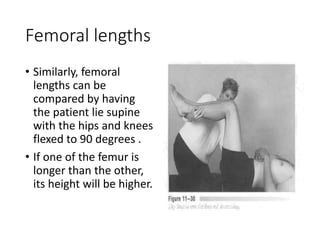
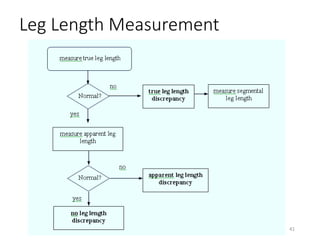
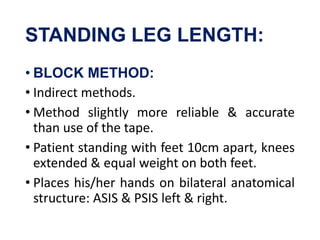
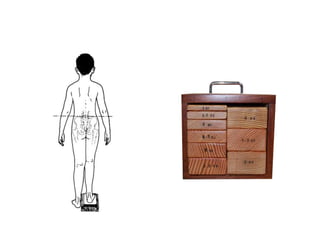
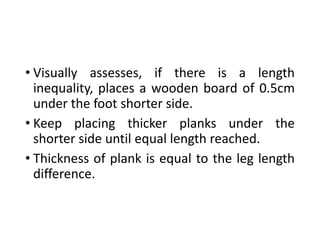
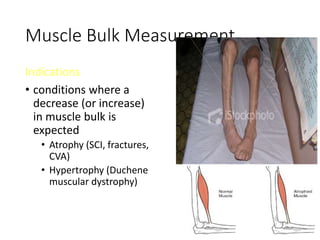
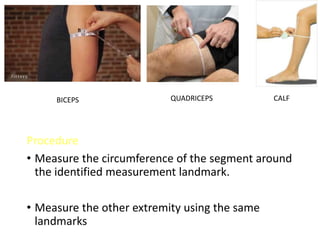
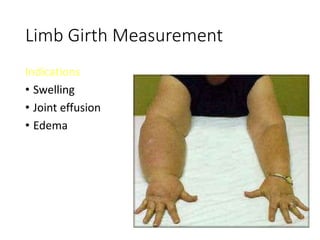
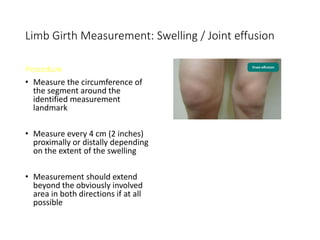
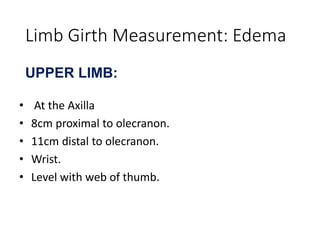
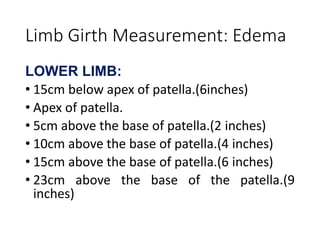
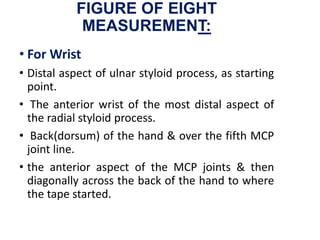
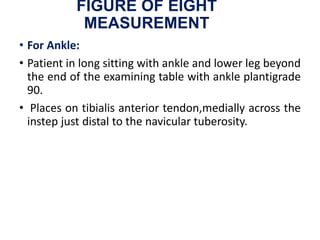
This document discusses various evaluation methods used in physical therapy, including anthropometry and limb length and girth measurements. It defines anthropometry as the scientific study of human body measurements and proportions. Limb length discrepancies, including true and apparent leg length discrepancies, are addressed. Proper techniques for measuring limb lengths, segments, and girth using a tape measure are outlined. The document provides detailed instructions on positioning, landmarks, and measuring various upper and lower body parts.