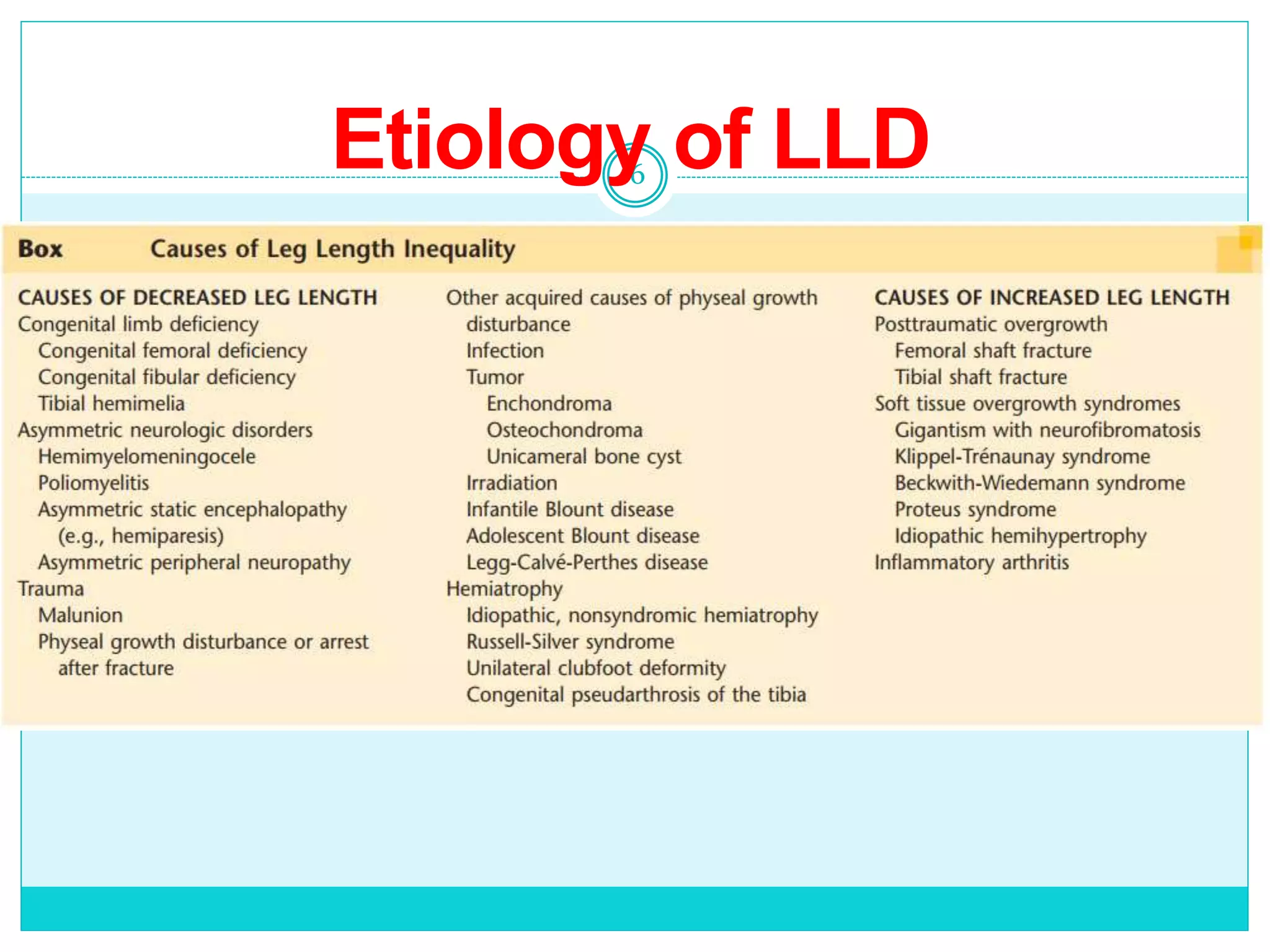
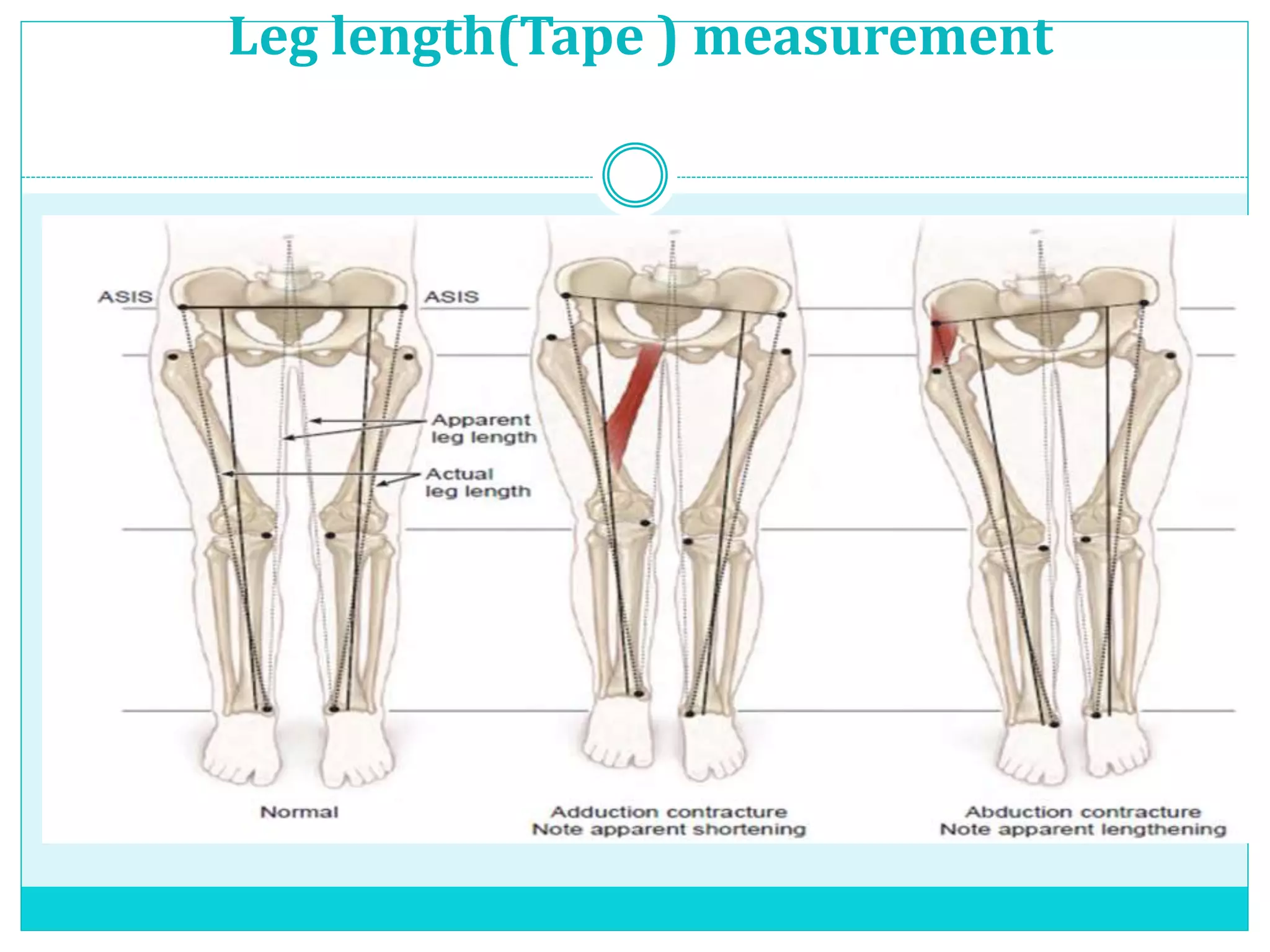
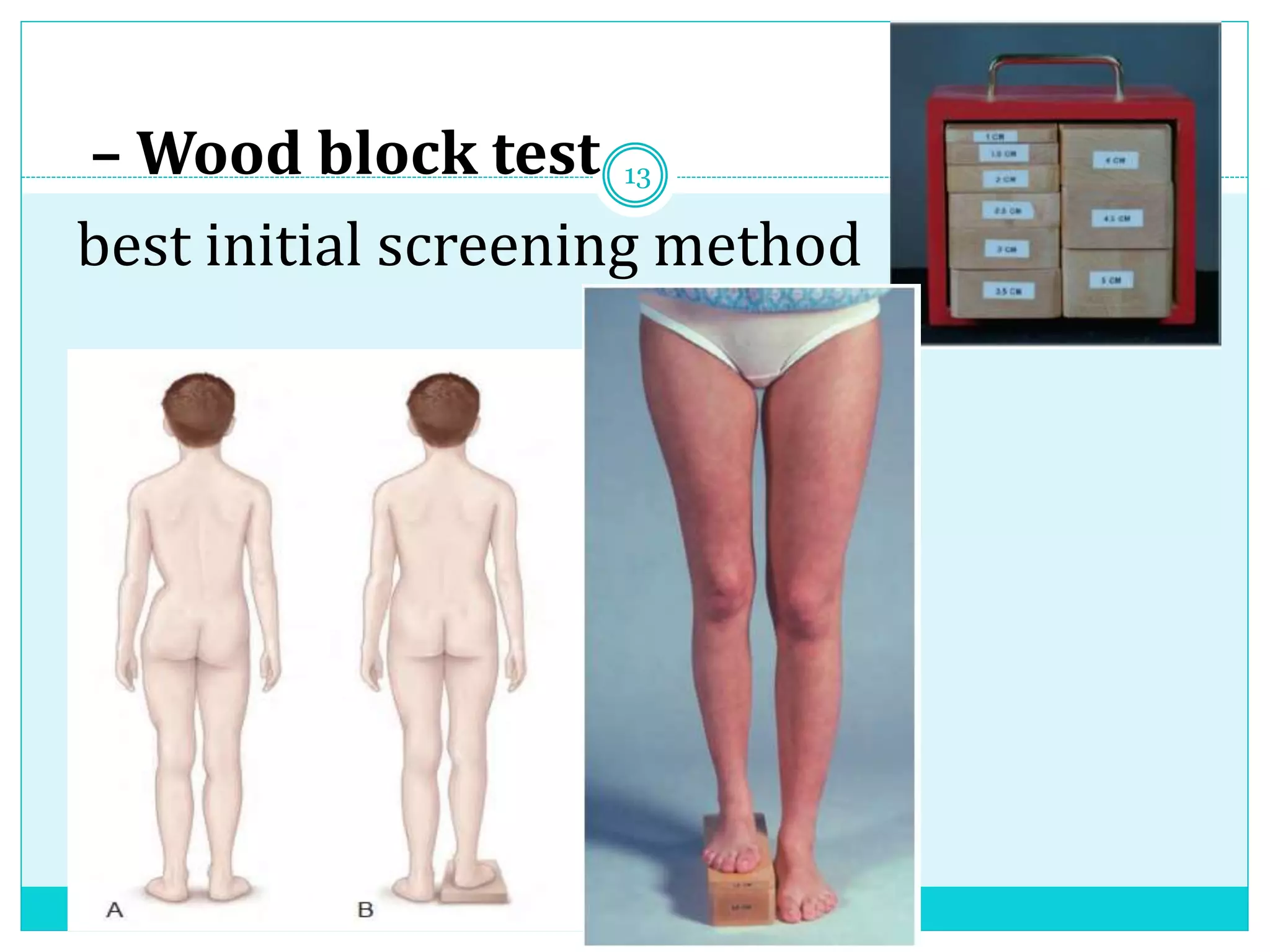
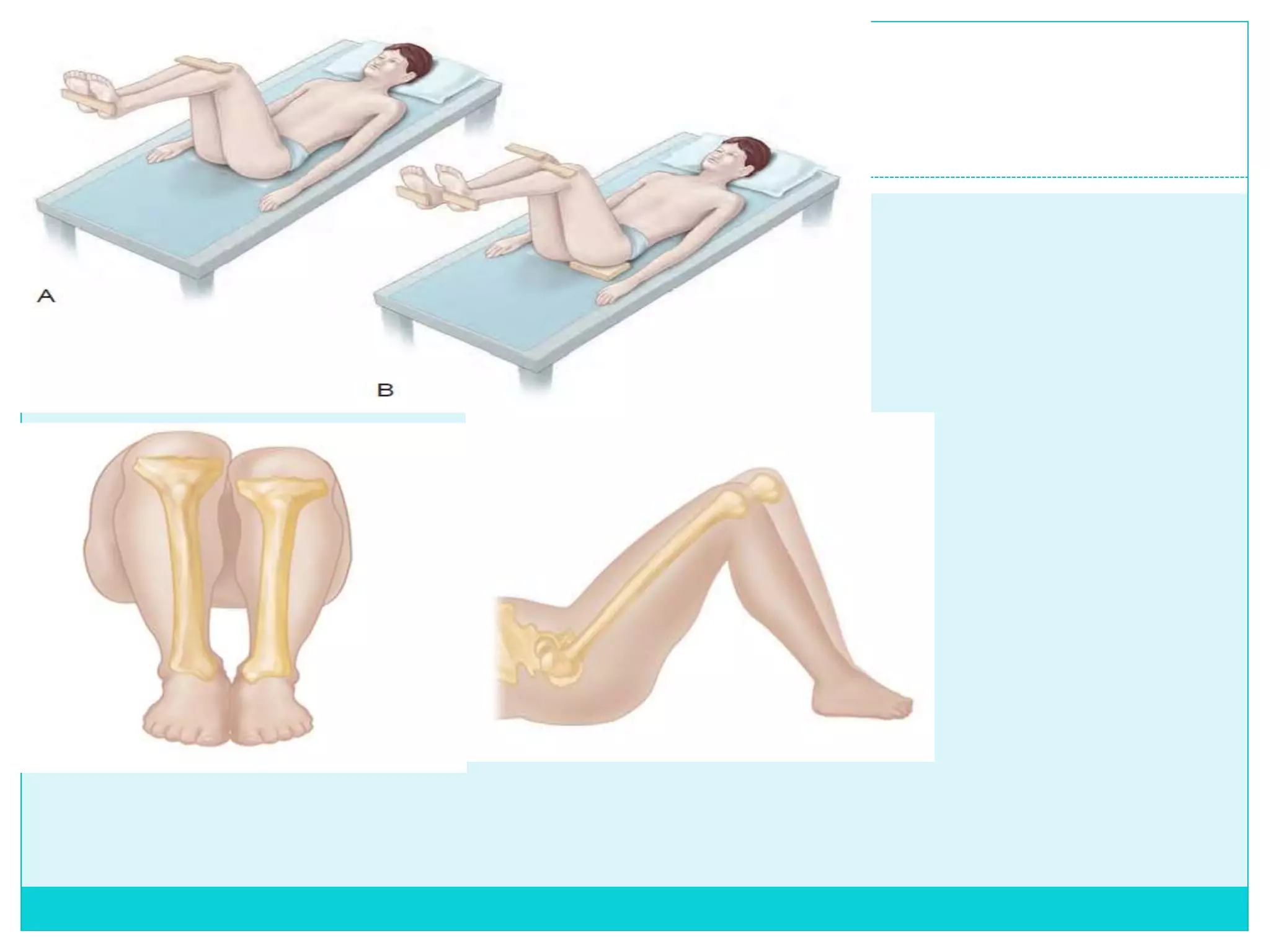
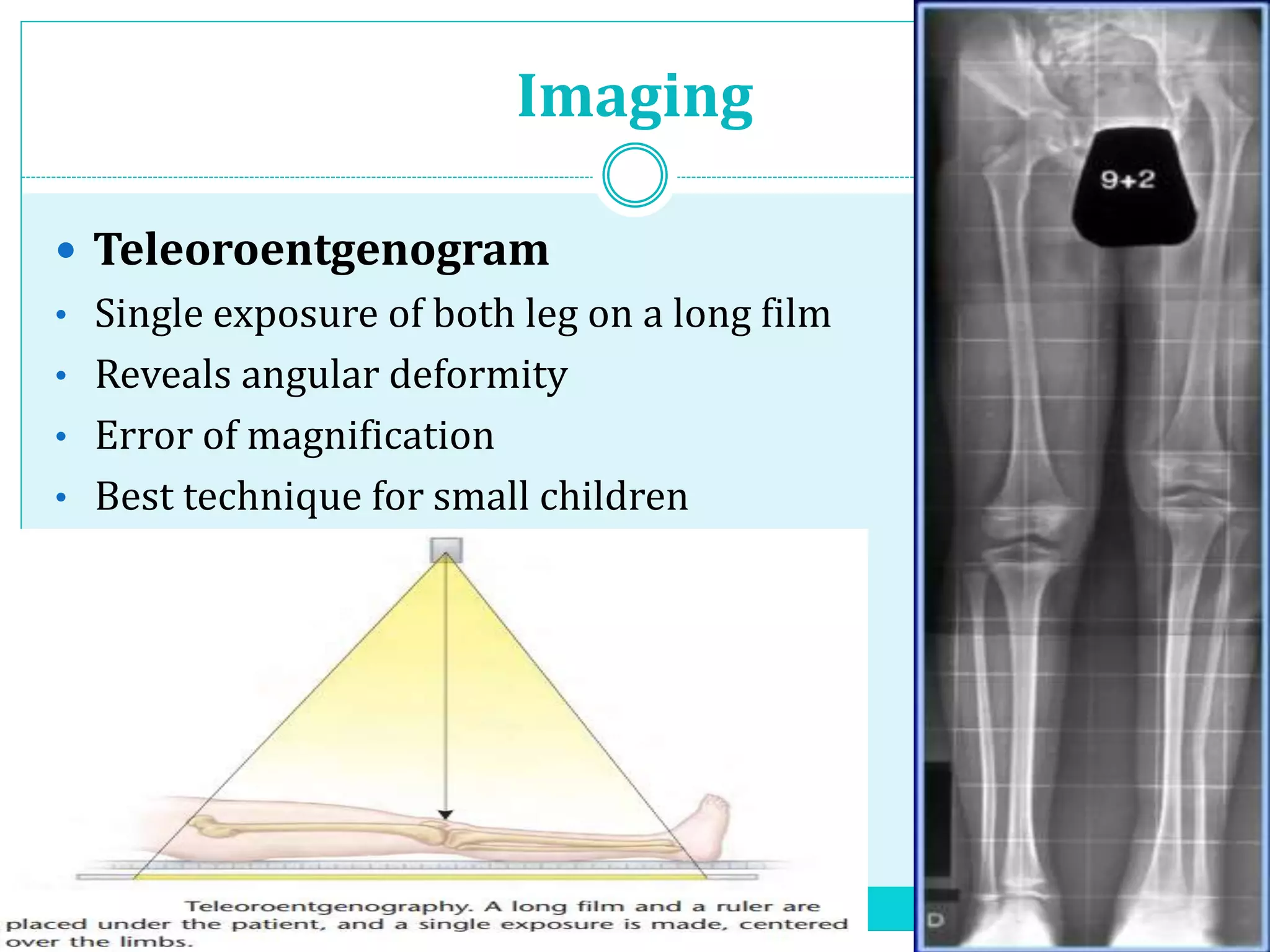
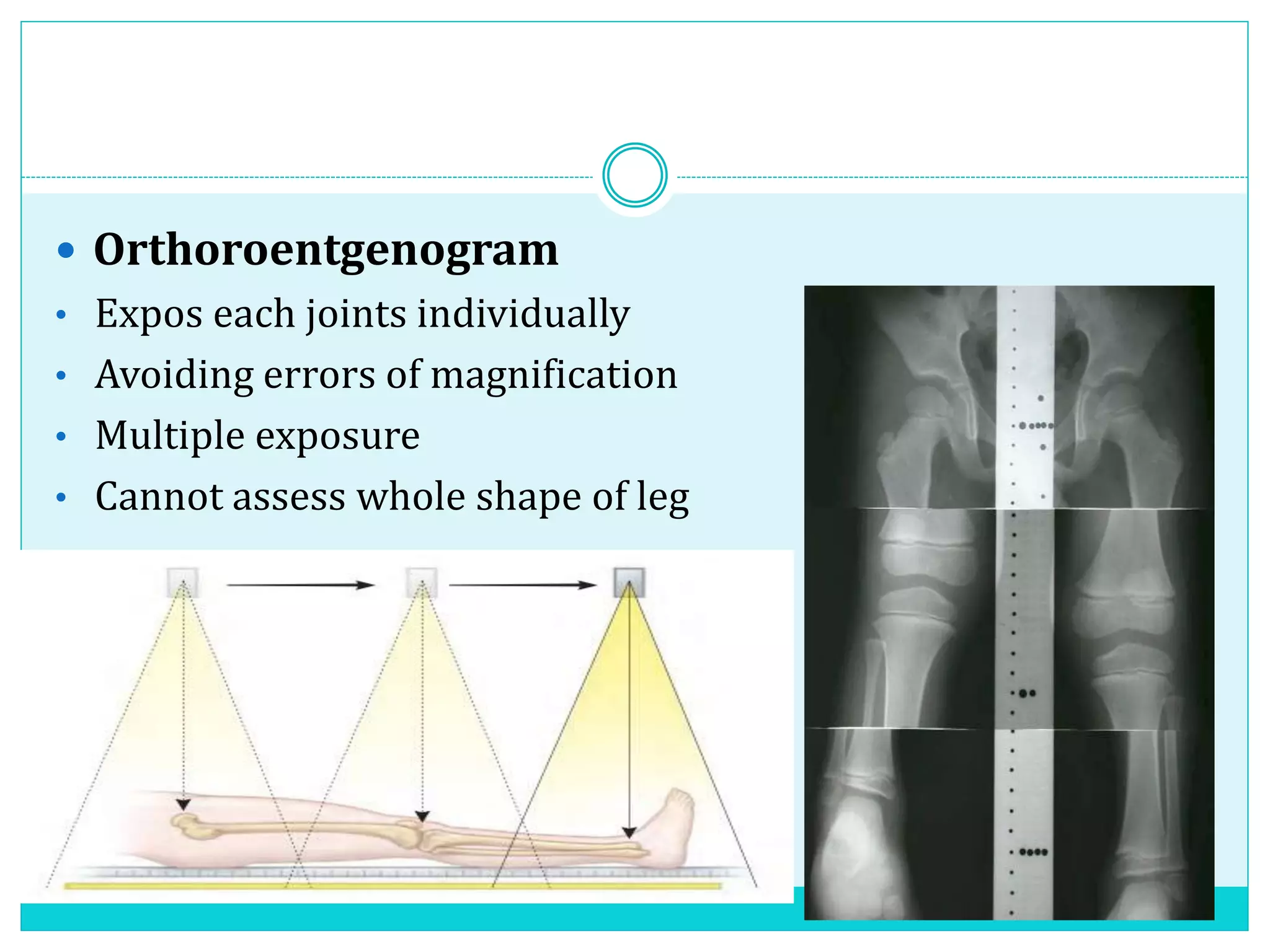
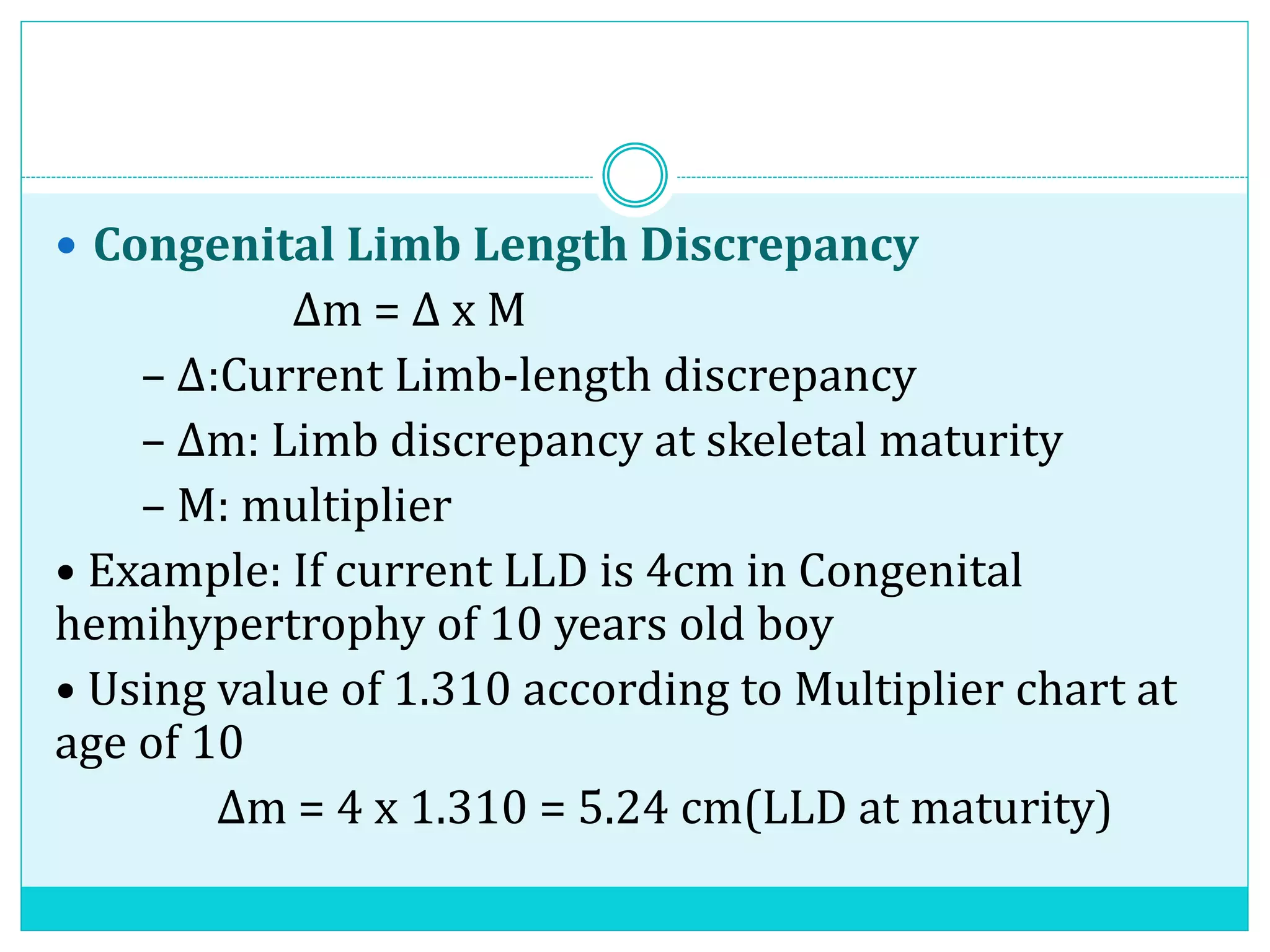
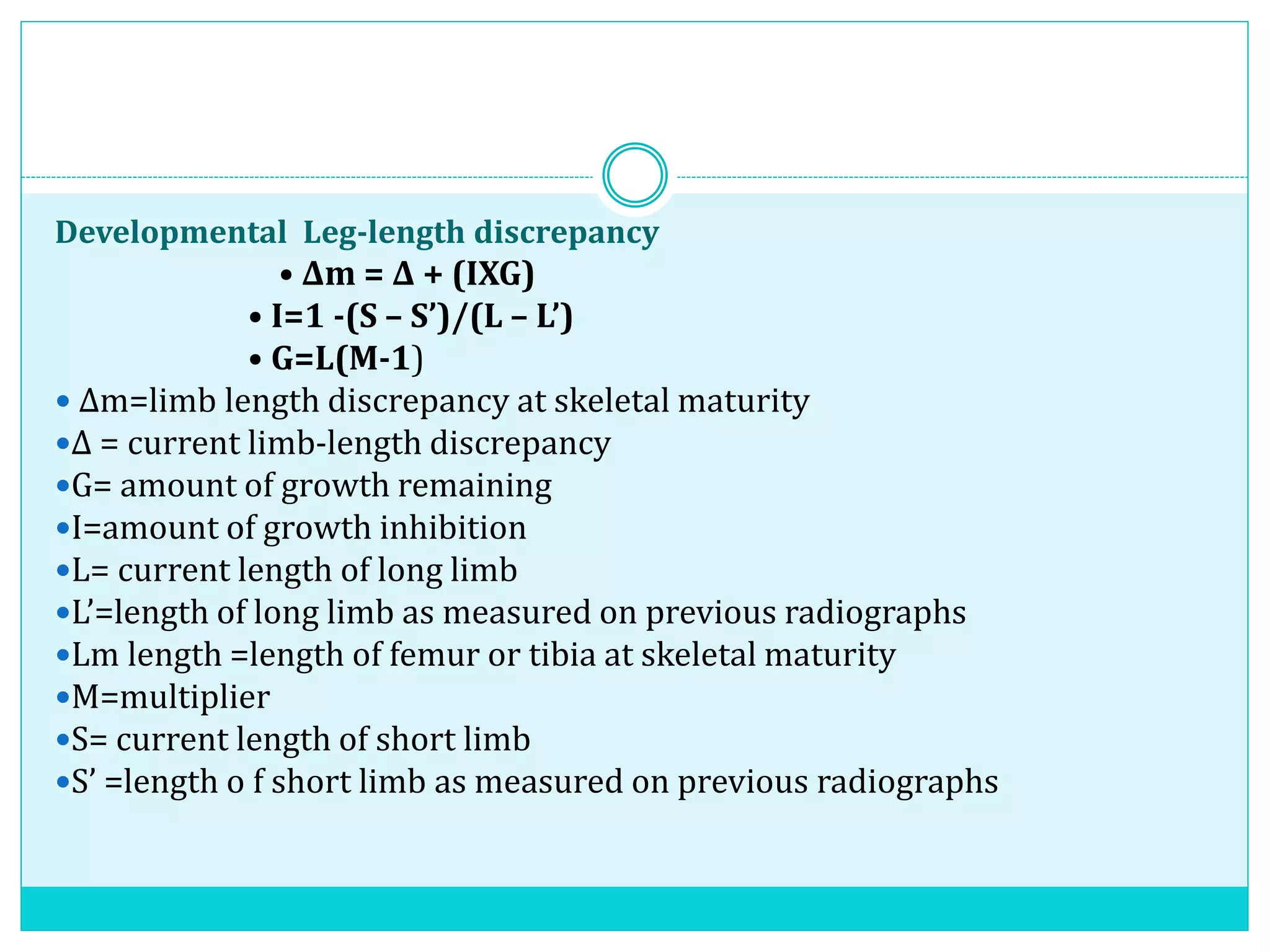
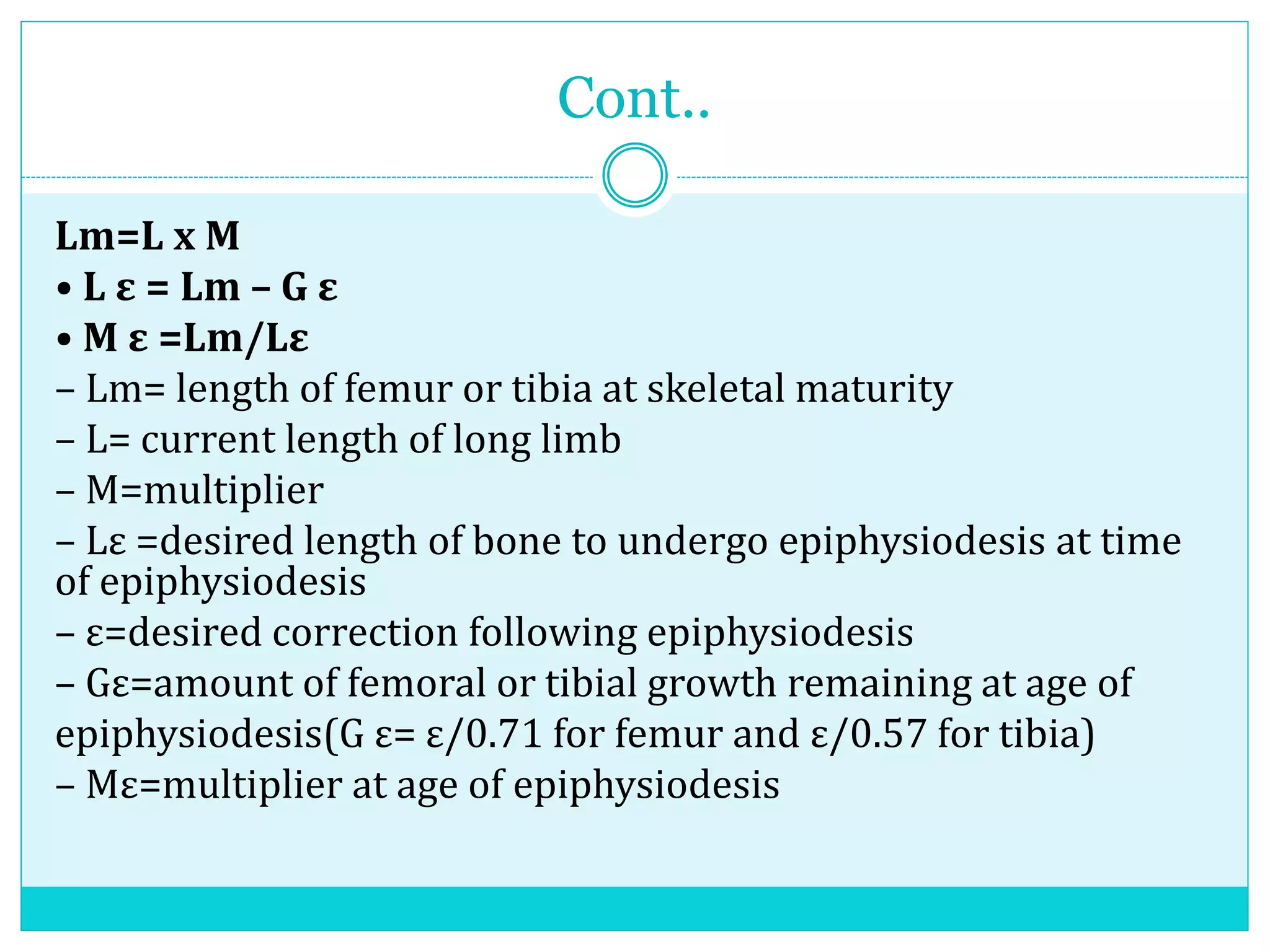
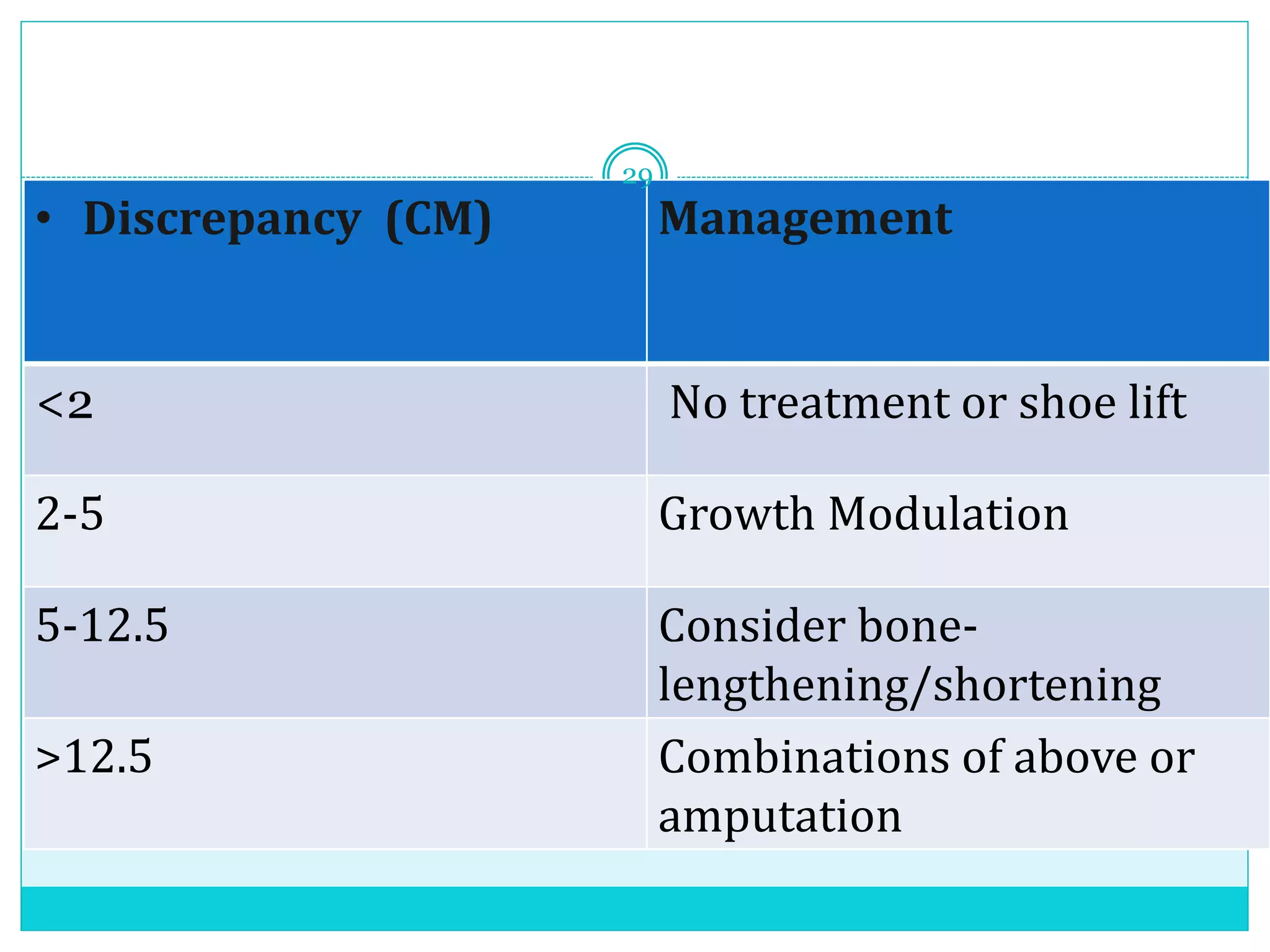
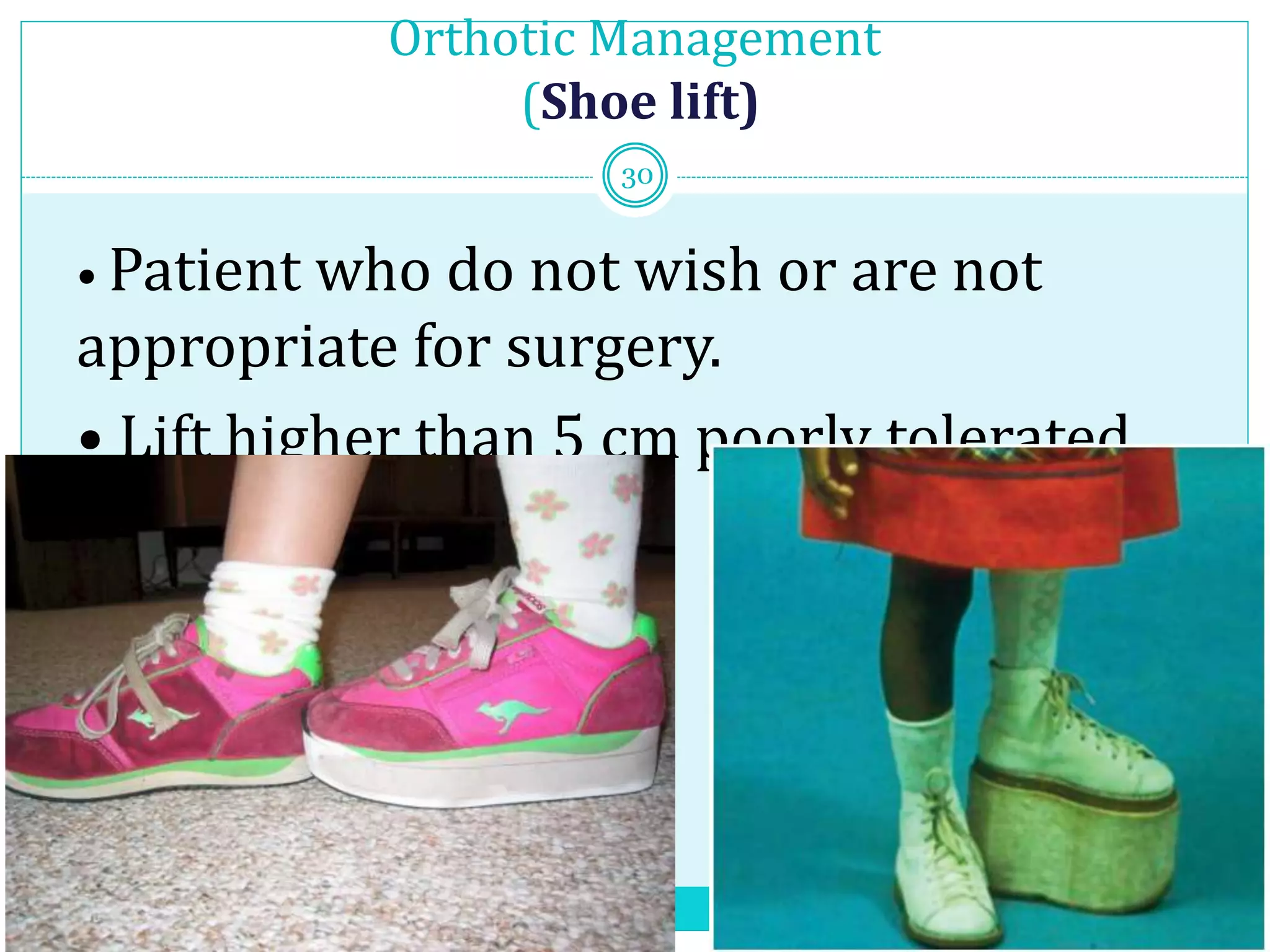
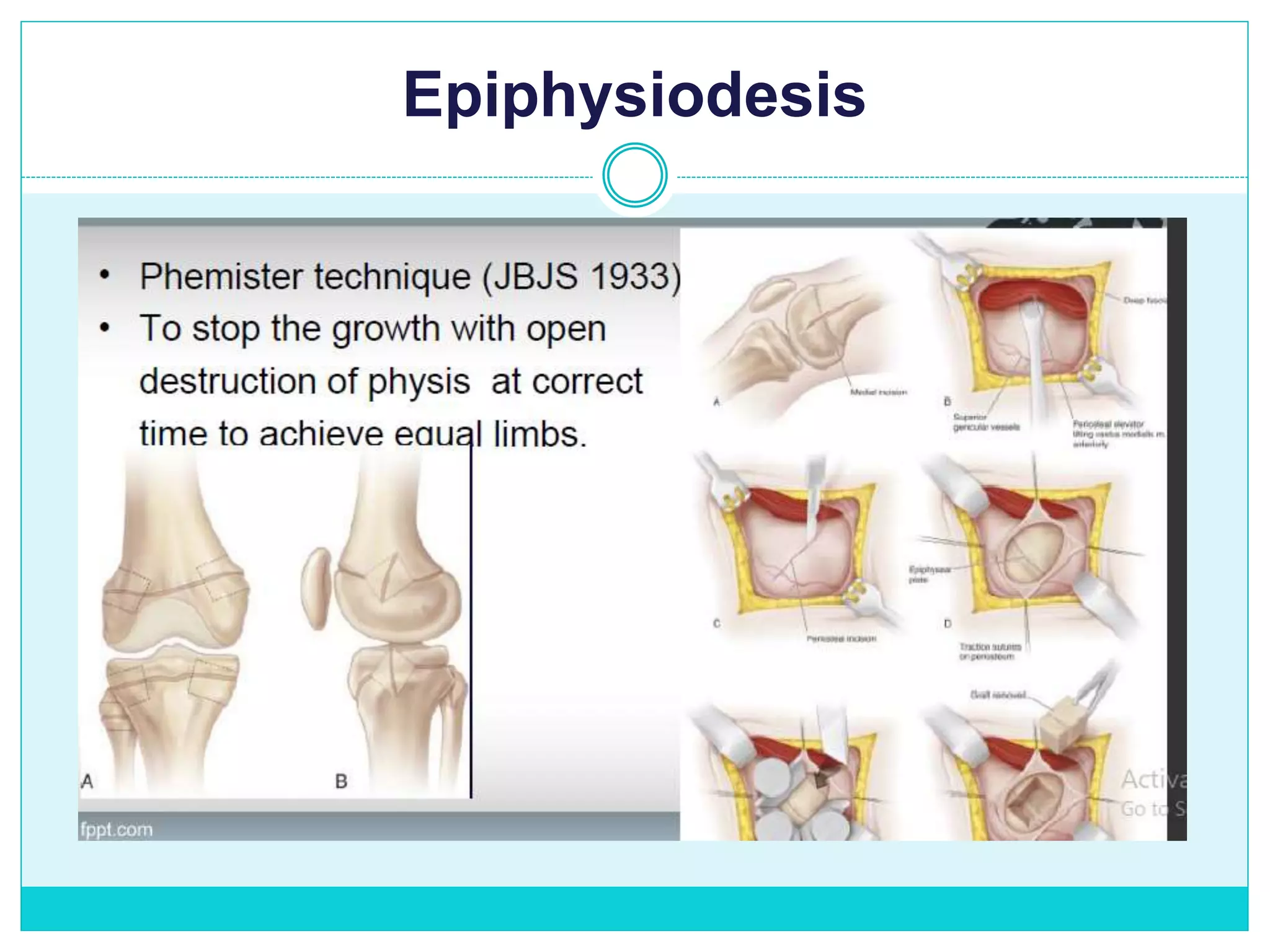
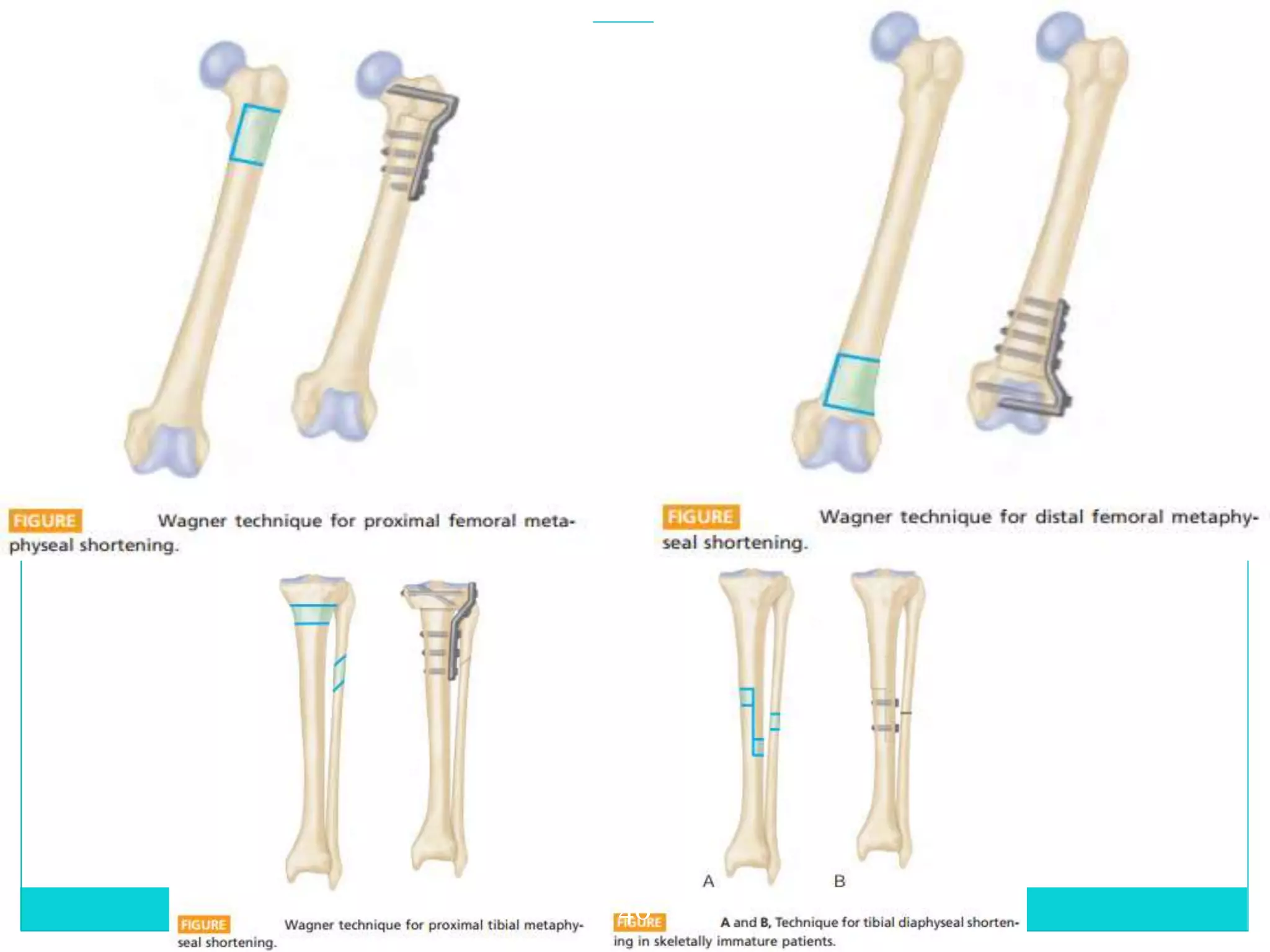
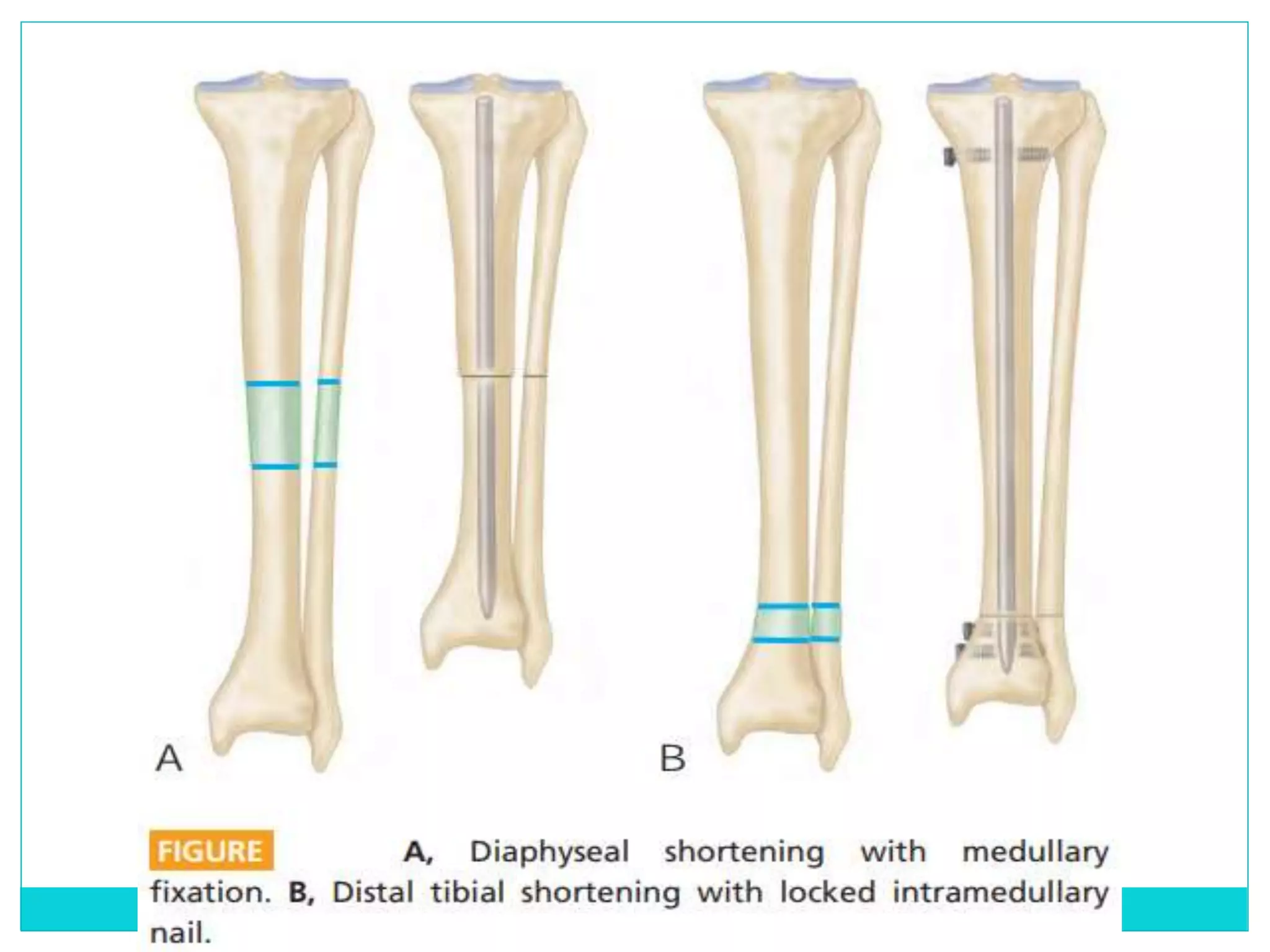
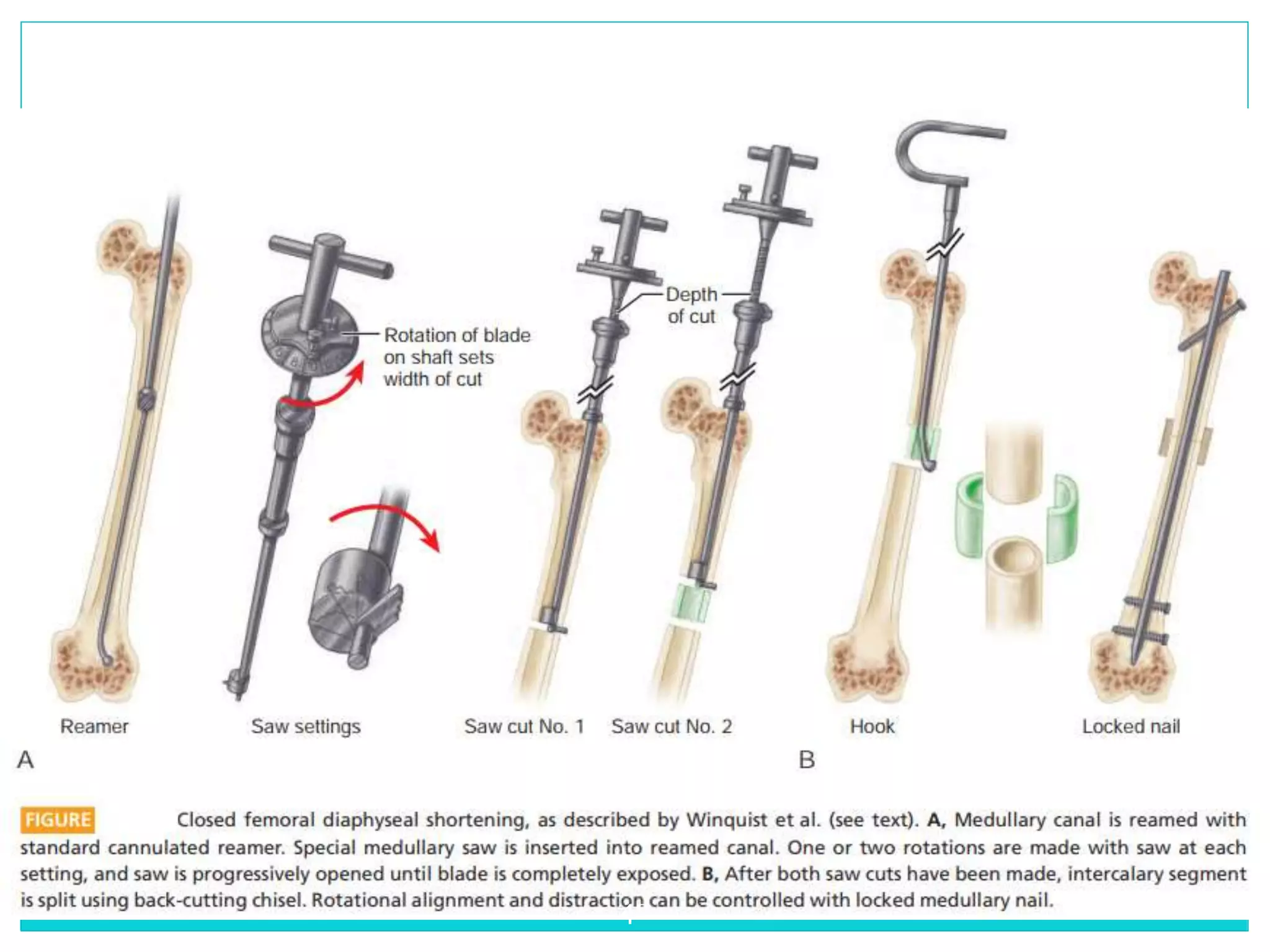
Limb length discrepancy can be structural or functional in nature. Structural discrepancies result from actual differences in bone length, while functional discrepancies appear due to other factors like pelvic tilt. Discrepancies over 2.5 cm are considered significant and can be classified as mild, moderate, or severe based on the size of the difference. Treatment depends on the size of the discrepancy and may include orthotics, epiphysiodesis, shortening osteotomies, limb lengthening procedures, or amputation in more severe cases. The goals of treatment are to achieve balanced alignment of the spine and pelvis and equalize limb lengths.