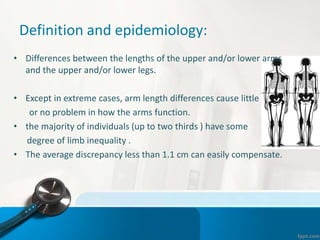
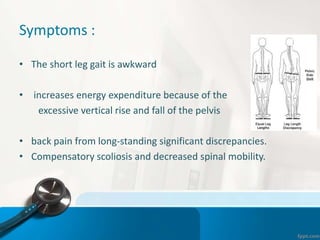
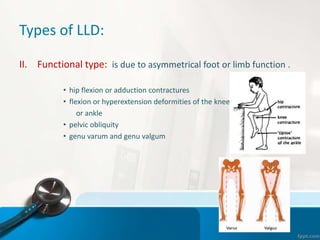
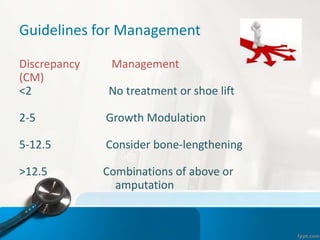
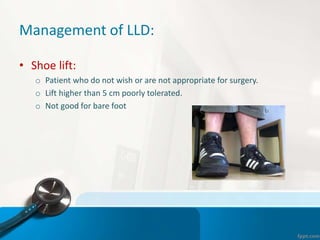
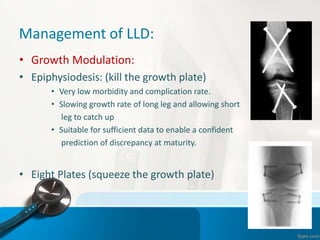
Limb-length discrepancy can be caused by structural, functional, or environmental factors that result in one leg being longer or shorter than the other. Symptoms of discrepancy include an awkward gait, back pain, and compensatory scoliosis. Discrepancies are classified as mild (<3cm), moderate (3-6cm), or severe (>6cm). Treatment depends on the magnitude of discrepancy and may include shoe lifts for mild cases, growth modulation for moderate, and limb lengthening or shortening surgery for severe discrepancies. The goal of treatment is to alleviate symptoms and prevent long-term complications.










![References:
• Robert M. Kliegman, Bonita F. Stanton, [2016]Nelson TEXTBOOK of PEDIATRICS,
20th ed. by Elsevier, Inc. Canada.
• Albert J. Pomeranz, Svapna Sabnis, [2016] PEDIATRIC DECISION-MAKING
STRATEGIES, SECOND EDITION, 2nd ed. An Imprint of Elsevier , Tennessee, USA.
• Solomon L., Warwick D. , Nayagam S.,[2010] Apley’s System of Orthopaedics and
Fractures, 9th ed. Hodderarnold comp.,London, UK.
• Miller M. , Thompson S. , Hart J. ,[2012] REVIEW OF ORTHOPAEDICS [PDF], 6th
ed. by Saunders, an imprint of Elsevier Inc. , Philadelphia, USA.
• Canale S. , Beaty J. , [2007] Campbell’s Operative Orthopaedics [PDF], 11th ed. By
Mosby, An Imprint of Elsevier , Tennessee, USA.
• Jay R. Lieberman, MD. , [2009] AAOS Comprehensive Orthopaedic Review,2nd ed.
American Academy of Orthopaedic Surgeons, USA.
• L. Ombregt, [2013] A System of Orthopaedic Medicine, 3rd ed. Elsevier Ltd. China.](https://image.slidesharecdn.com/limb-lengthdiscrepancyevaluation-160412102533/85/Limb-length-discrepancy-evaluation-28-320.jpg)
