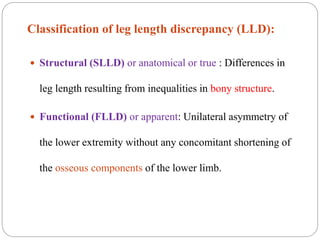
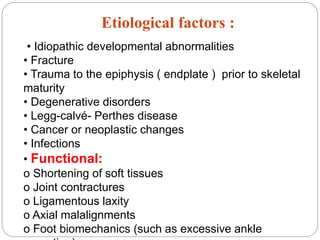
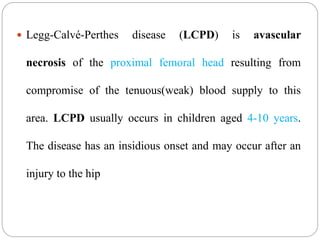
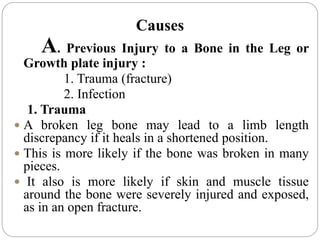
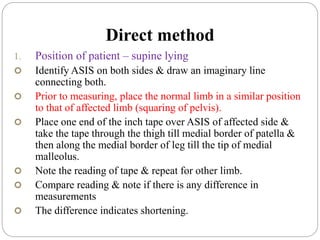
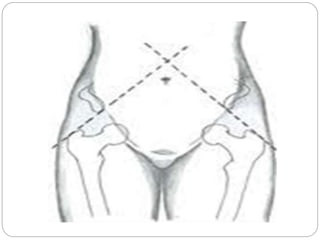
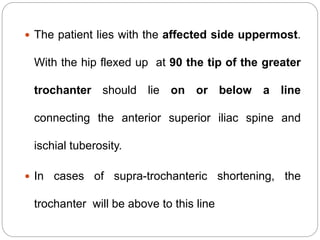
This document provides information on limb length measurement and discrepancies. It defines true and apparent limb length measurement and describes various methods to measure limb lengths, including using a tape measure between bony landmarks or blocks under the shorter limb. Causes of limb length discrepancies include fractures, infections, bone diseases, tumors and more. Supra-trochanteric and infra-trochanteric shortening are distinguished and different measurement techniques are outlined for each.